Table of Contents
Introduction
Metformin is the first-line oral antidiabetic drug used in the treatment of type 2 diabetes mellitus. It belongs to the class of biguanides and is known for its ability to lower blood glucose without causing significant hypoglycemia.
Due to its high safety margin, affordability, and cardiometabolic benefits, Metformin is a key drug across various guidelines, including those by ADA (American Diabetes Association) and AACE (American Association of Clinical Endocrinologists).
Metformin is also used in other insulin-resistant conditions such as:
- Polycystic ovary syndrome (PCOS)
- Non-alcoholic fatty liver disease (NAFLD)
- Prediabetes
It is frequently tested in USMLE, NCLEX, NAPLEX, GPAT, and NEET-PG.
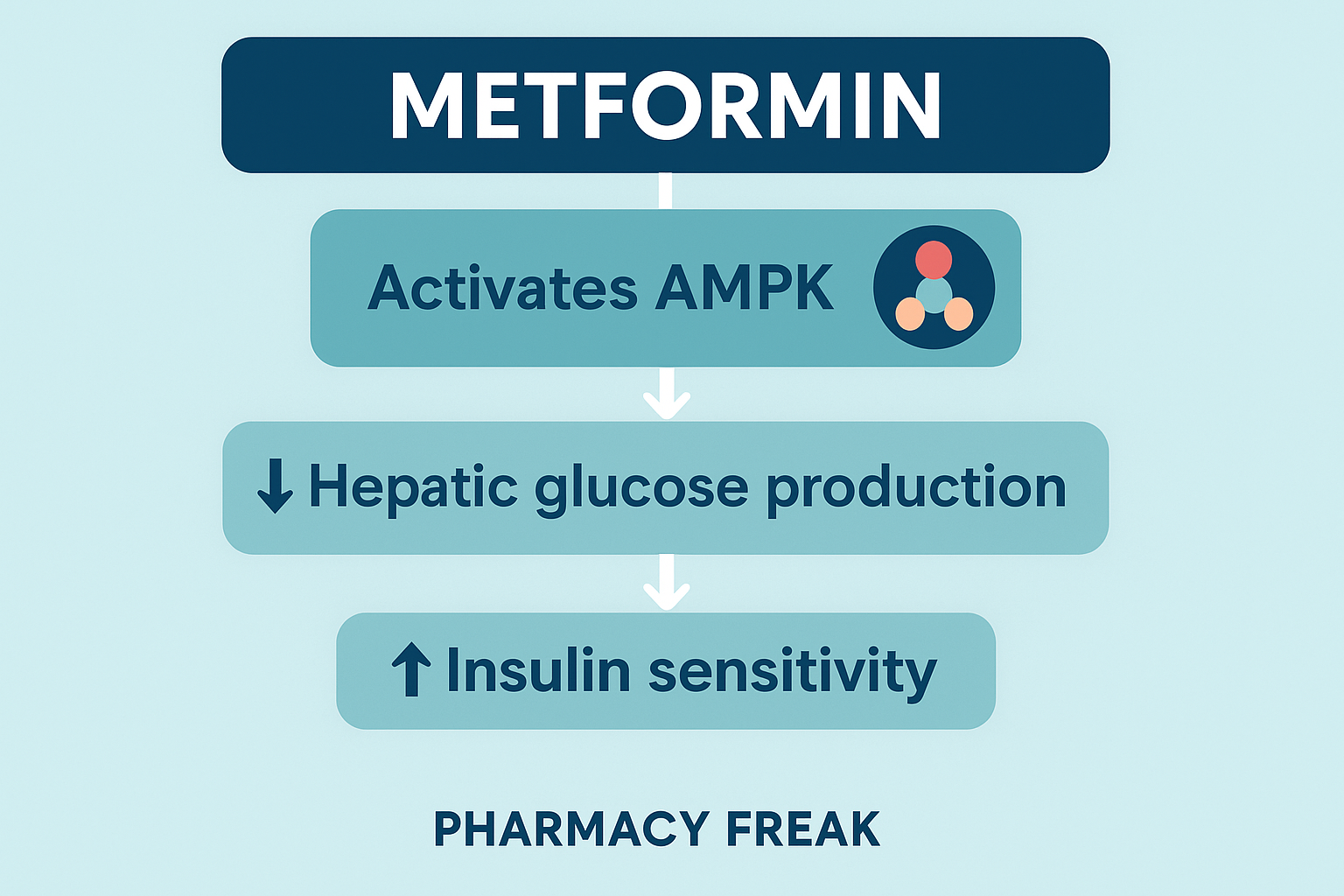
Stepwise Mechanism of Action of Metformin
- Primary Site of Action – Liver
Metformin primarily acts on the liver to reduce hepatic glucose production by inhibiting gluconeogenesis. - Activation of AMP-activated protein kinase (AMPK):
Metformin activates AMPK, a cellular energy sensor, which inhibits key enzymes involved in hepatic gluconeogenesis, thereby reducing glucose output. - Improved Insulin Sensitivity:
It increases insulin sensitivity in muscle and adipose tissues, promoting enhanced peripheral glucose uptake and utilization. - Reduced Intestinal Glucose Absorption:
Metformin modestly decreases the absorption of glucose from the gastrointestinal tract, further contributing to glucose control. - Does Not Stimulate Insulin Secretion:
Unlike sulfonylureas, metformin does not increase insulin secretion, and hence, does not cause hypoglycemia. - Lipid and Cardiovascular Effects:
Metformin also improves lipid profile and has cardiovascular benefits, including weight neutrality or modest weight loss.

Pharmacokinetic Parameters of Metformin
| Parameter | Value |
|---|---|
| Bioavailability | ~50–60% (oral) |
| Onset of Action | Within days; maximum effect in 1–2 weeks |
| Half-life | ~4–8 hours |
| Protein Binding | Negligible |
| Metabolism | Not metabolized; excreted unchanged |
| Excretion | Renal via active tubular secretion |
Clinical Uses of Metformin
- Type 2 diabetes mellitus (first-line therapy)
- Polycystic ovary syndrome (PCOS)
- Prediabetes or impaired glucose tolerance
- Non-alcoholic fatty liver disease (NAFLD)
- Obesity and insulin resistance syndromes
Adverse Effects of Metformin
- Gastrointestinal upset: Nausea, diarrhea, abdominal discomfort
- Metallic taste in mouth
- Vitamin B12 deficiency with long-term use
- Lactic acidosis (rare but serious, especially in renal or hepatic impairment)
- Contraindicated in patients with:
- Severe renal impairment (eGFR <30 mL/min)
- Acute or chronic metabolic acidosis
- History of lactic acidosis
Comparative Analysis: Metformin vs Sulfonylureas
| Feature | Metformin | Sulfonylureas |
|---|---|---|
| Site of Action | Liver, muscle, gut | Pancreatic beta cells |
| Risk of Hypoglycemia | Very low | High |
| Weight Effect | Neutral or weight loss | Weight gain |
| Cardiovascular Benefit | Proven (e.g., UKPDS trial) | Less clear |
| Insulin Secretion | No | Yes (stimulates) |
| Use in PCOS | Yes | No |
Practice MCQs
Q1. What is the primary mechanism of action of Metformin?
a. Stimulates insulin release from beta cells
b. Inhibits renal glucose reabsorption
c. Inhibits hepatic gluconeogenesis ✅
d. Activates SGLT2 in proximal tubule
Q2. Metformin primarily activates which enzyme to exert its effect?
a. Na⁺/K⁺ ATPase
b. AMPK ✅
c. Adenylate cyclase
d. Protein kinase A
Q3. Which of the following is NOT a known benefit of Metformin?
a. Weight loss
b. Increased insulin secretion ✅
c. Improved lipid profile
d. Reduced hepatic glucose output
Q4. Which of the following is the most serious potential adverse effect of Metformin?
a. Lactic acidosis ✅
b. Hypoglycemia
c. Pancreatitis
d. QT prolongation
Q5. How is Metformin excreted?
a. Bile
b. Sweat
c. Lungs
d. Kidneys (unchanged) ✅
Q6. Metformin is contraindicated in:
a. Mild GERD
b. Iron-deficiency anemia
c. Severe renal impairment ✅
d. Hypertension
Q7. Which of the following best describes Metformin’s hypoglycemia risk?
a. Very high
b. Moderate
c. Low ✅
d. Same as insulin
Q8. Metformin’s effect on insulin levels is best described as:
a. Direct stimulation
b. No effect on insulin secretion ✅
c. Beta cell destruction
d. Delayed insulin release
Q9. Metformin is commonly associated with:
a. Blurred vision
b. Rash
c. GI upset ✅
d. Hypokalemia
Q10. Long-term use of Metformin can result in deficiency of:
a. Iron
b. Calcium
c. Vitamin D
d. Vitamin B12 ✅
FAQs
Q1: Can Metformin be used in type 1 diabetes?
No. It is ineffective as monotherapy in type 1 diabetes, but may be used as adjunct in insulin-resistant type 1 patients under supervision.
Q2: Why is Metformin the first-line drug in type 2 diabetes?
It lowers glucose effectively without causing hypoglycemia or weight gain, and improves cardiovascular outcomes.
Q3: Can Metformin be used in pregnancy?
Yes, it may be used in gestational diabetes if lifestyle changes are insufficient, under strict medical supervision.
Q4: How is the risk of lactic acidosis minimized?
Avoid Metformin in patients with severe renal, hepatic, or cardiac dysfunction and monitor renal function regularly.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Review of Pharmacology – Sparsh Gupta

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com