Table of Contents
Introduction
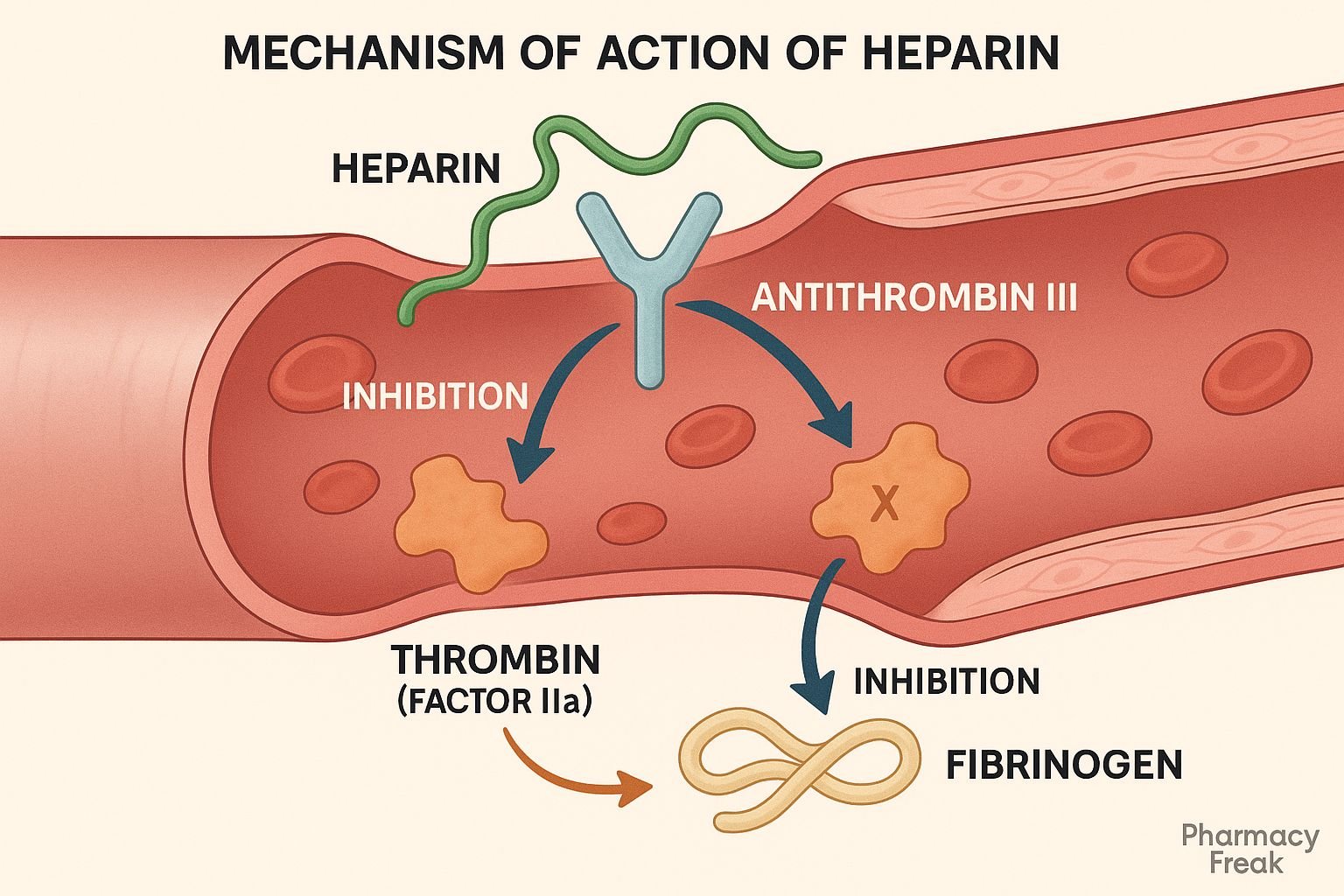
Heparin is a widely used anticoagulant primarily employed in the prevention and treatment of thromboembolic disorders such as deep vein thrombosis, pulmonary embolism, and myocardial infarction. As a naturally occurring glycosaminoglycan, heparin exerts its anticoagulant effects by enhancing the activity of antithrombin III (AT III), leading to the inactivation of key coagulation factors. It is available in both unfractionated and low molecular weight forms, each with distinct pharmacokinetic properties but a similar mechanism of action.
Step-by-Step Mechanism of Action
- Binding to Antithrombin III (AT III)
Heparin binds to antithrombin III via a unique pentasaccharide sequence in its structure, inducing a conformational change that significantly enhances the activity of AT III. - Acceleration of Factor Inhibition
Activated antithrombin III rapidly inactivates clotting enzymes, primarily thrombin (Factor IIa) and Factor Xa. The rate of this inhibition increases by 1000-fold in the presence of heparin. - Inhibition of the Common Pathway
By neutralizing thrombin and Factor Xa, heparin prevents the conversion of fibrinogen to fibrin, effectively halting the formation of a stable clot. - Unfractionated vs. Low Molecular Weight Heparin (LMWH)
- Unfractionated heparin (UFH) inhibits both Factor Xa and thrombin (IIa).
- LMWH, due to its smaller size, predominantly inhibits Factor Xa and has minimal effect on thrombin.
- Immediate Anticoagulant Effect
Because heparin acts directly in the blood and does not require hepatic activation, its onset of action is immediate when administered intravenously.
Pharmacokinetic Parameters
| Parameter | Unfractionated Heparin | Low Molecular Weight Heparin (LMWH) |
|---|---|---|
| Bioavailability | Poor (IV or SC only) | ~90% (SC) |
| Onset of action | Immediate (IV), 20–60 min (SC) | 3–5 hours |
| Half-life | 1–2 hours (dose-dependent) | 4–6 hours |
| Excretion | Reticuloendothelial system, renal | Primarily renal |
| Monitoring | aPTT | Anti-Xa level (optional) |
Clinical Uses
- Deep vein thrombosis (DVT)
- Pulmonary embolism (PE)
- Acute coronary syndromes (ACS)
- Atrial fibrillation (prevention of stroke)
- During cardiac and vascular surgery
- Hemodialysis anticoagulation
Adverse Effects
- Bleeding (major complication)
- Heparin-induced thrombocytopenia (HIT)
- Osteoporosis (with prolonged use)
- Hypersensitivity reactions
- Elevation of liver enzymes
- Hyperkalemia (via aldosterone suppression)
Comparative Analysis
Unfractionated Heparin vs. LMWH:
- UFH has a shorter half-life and requires close monitoring (aPTT).
- LMWH has a more predictable dose-response, longer half-life, and is administered subcutaneously.
- UFH is preferred when rapid reversal is required (e.g., surgery), while LMWH is favored in outpatient settings.
MCQs
1. What is the primary mechanism of action of heparin?
a) Platelet aggregation inhibition
b) Direct thrombin inhibition
c) Enhancing antithrombin III activity
d) Vitamin K antagonism
Answer: c) Enhancing antithrombin III activity
2. Heparin mainly inactivates which coagulation factors?
a) IIa and Xa
b) VII and IX
c) IXa and XIa
d) V and VIII
Answer: a) IIa and Xa
3. Which of the following is a serious adverse effect of heparin therapy?
a) Agranulocytosis
b) Heparin-induced thrombocytopenia
c) Stevens-Johnson Syndrome
d) Torsades de Pointes
Answer: b) Heparin-induced thrombocytopenia
4. LMWH differs from unfractionated heparin by:
a) Increased risk of HIT
b) Predominant inhibition of Factor Xa
c) Poor subcutaneous bioavailability
d) Requirement of IV administration
Answer: b) Predominant inhibition of Factor Xa
5. What test is commonly used to monitor unfractionated heparin therapy?
a) PT
b) INR
c) aPTT
d) Platelet count
Answer: c) aPTT
6. Heparin’s anticoagulant action begins:
a) After 2–4 hours
b) Within 20 minutes
c) Immediately after IV administration
d) After hepatic metabolism
Answer: c) Immediately after IV administration
7. Which of the following is an antidote for heparin overdose?
a) Vitamin K
b) Protamine sulfate
c) Desmopressin
d) Fresh frozen plasma
Answer: b) Protamine sulfate
8. What is the route of elimination for LMWH?
a) Hepatic
b) Biliary
c) Renal
d) Pulmonary
Answer: c) Renal
9. Long-term use of heparin can cause:
a) Cardiac arrhythmias
b) Hypokalemia
c) Osteoporosis
d) Retinopathy
Answer: c) Osteoporosis
10. Which of the following does NOT require routine aPTT monitoring?
a) Unfractionated heparin
b) Warfarin
c) LMWH
d) Argatroban
Answer: c) LMWH
FAQs
1. Can heparin be given orally?
No, it is not absorbed orally and must be given parenterally.
2. Is monitoring always required for LMWH?
Routine monitoring is not usually necessary but may be done in renal impairment or pregnancy.
3. What is the antidote for heparin overdose?
Protamine sulfate neutralizes the anticoagulant effect of heparin.
4. Can heparin be used in pregnancy?
Yes, it does not cross the placenta and is considered safe in pregnancy.
5. What is Heparin-induced thrombocytopenia (HIT)?
A rare immune-mediated reaction where heparin forms complexes with platelets, leading to their destruction and paradoxical thrombosis.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 13th Edition.
- KD Tripathi. Essentials of Medical Pharmacology, 8th Edition.
- https://pubmed.ncbi.nlm.nih.gov/11312884/
- https://pubmed.ncbi.nlm.nih.gov/12730086/
I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com