Table of Contents
Introduction
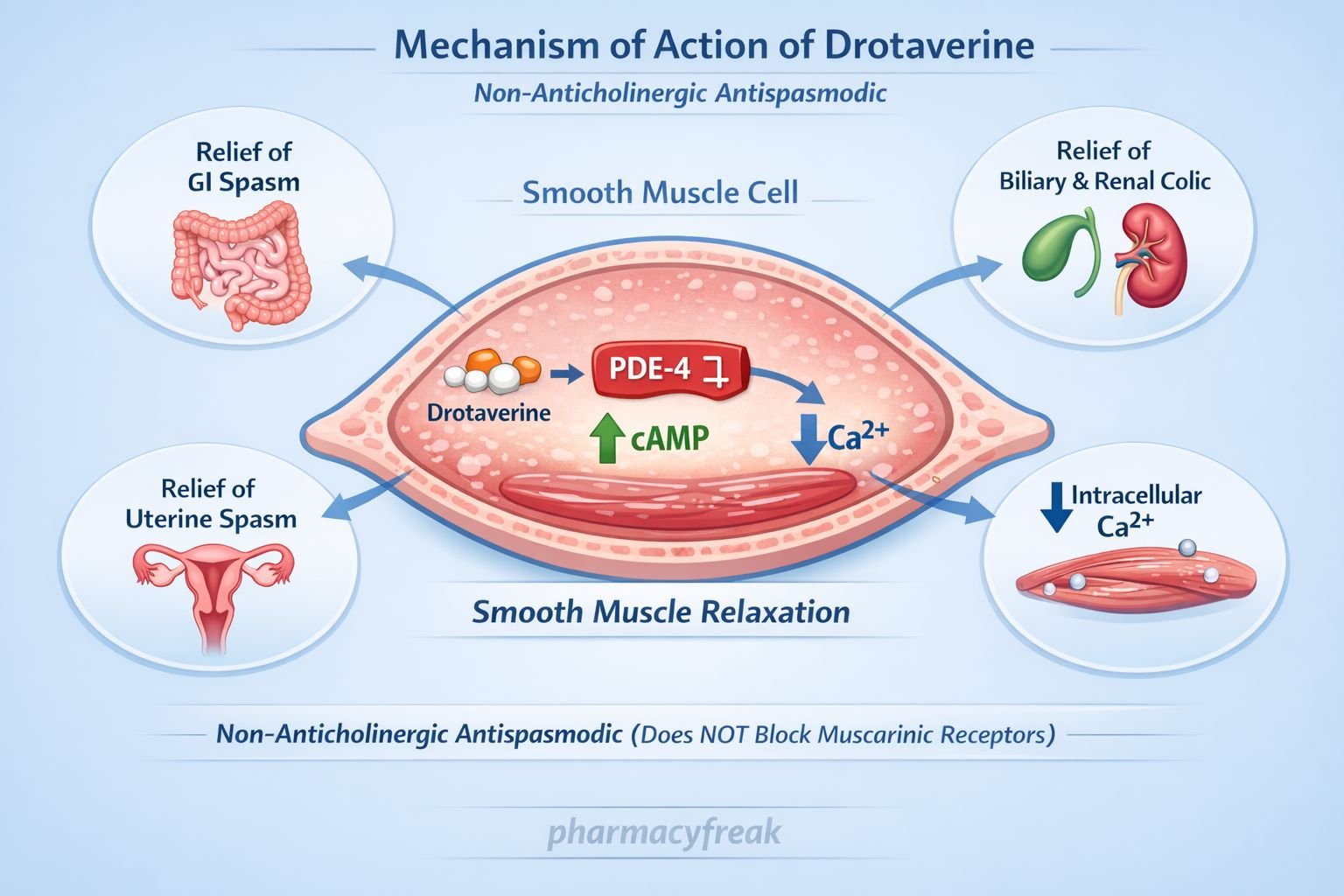
Drotaverine is a myotropic antispasmodic agent widely used for the relief of smooth muscle spasm–related pain involving the gastrointestinal, biliary, genitourinary, and uterine systems. Unlike anticholinergic antispasmodics, drotaverine acts directly on smooth muscle without significant effects on autonomic receptors. It is a high-yield drug in pharmacology and clinical examinations because of its phosphodiesterase inhibition–based mechanism and favorable safety profile with minimal anticholinergic adverse effects.

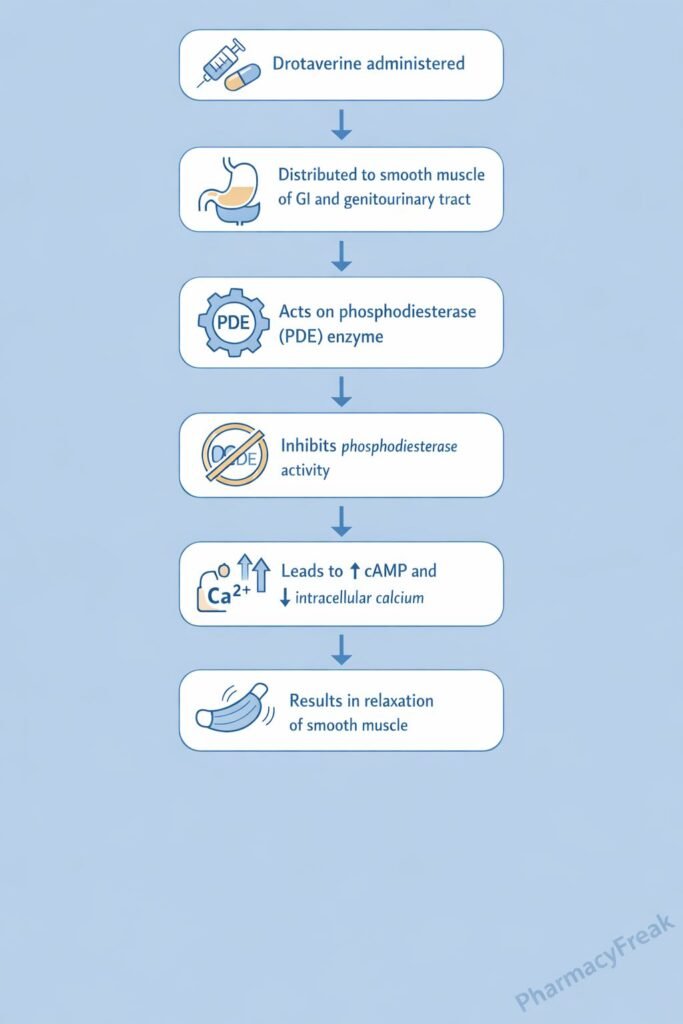
Mechanism of Action (Step-wise)
Drotaverine relaxes smooth muscle by increasing intracellular cyclic nucleotides and reducing calcium availability.
- Presence of Smooth Muscle Spasm
Spasm of smooth muscle is mediated by increased intracellular calcium leading to sustained contraction. - Inhibition of Phosphodiesterase (PDE-4)
Drotaverine selectively inhibits phosphodiesterase-4 in smooth muscle cells. - Reduced Breakdown of cAMP
PDE inhibition prevents degradation of cyclic adenosine monophosphate (cAMP). - Increase in Intracellular cAMP Levels
Elevated cAMP activates protein kinase A (PKA). - Reduction in Intracellular Calcium
PKA activity decreases calcium influx and promotes calcium sequestration. - Smooth Muscle Relaxation
Reduced calcium availability leads to relaxation of smooth muscle fibers. - Antispasmodic Effect
Relief of spasm reduces pain and improves functional obstruction. - No Anticholinergic Action
Drotaverine does not block muscarinic receptors, preserving normal autonomic function.
Pharmacokinetics
- Absorption: Well absorbed orally
- Bioavailability: Moderate
- Distribution: Widely distributed in smooth muscle–rich tissues
- Metabolism: Hepatic metabolism
- Elimination: Renal excretion of metabolites
- Half-life: Approximately 7–12 hours
- Special feature: Does not cross the blood–brain barrier significantly
Clinical Uses
Drotaverine is used to relieve smooth muscle spasm–associated pain:
- Gastrointestinal colic (intestinal spasm, IBS)
- Biliary colic
- Renal colic (adjunct)
- Dysmenorrhea
- Uterine spasm
- Spastic conditions of the urinary tract
It is often preferred when anticholinergic drugs are contraindicated.
Adverse Effects
Drotaverine is generally well tolerated:
- Common:
- Headache
- Dizziness
- Nausea
- Cardiovascular (rare):
- Hypotension
- Palpitations (high doses)
- Others:
- Flushing
Notably, anticholinergic adverse effects are absent.
Comparative Analysis (must include a table + explanation)
Comparison of Antispasmodic Drugs
| Feature | Drotaverine | Dicyclomine | Hyoscine |
|---|---|---|---|
| Mechanism | PDE inhibition | Muscarinic blockade | Muscarinic blockade |
| Anticholinergic effects | No | Yes | Yes |
| CNS effects | Minimal | Moderate | Significant |
| Use in colic | Yes | Yes | Yes |
| Safety in glaucoma/BPH | Safer | Caution | Caution |
Explanation:
Drotaverine acts directly on smooth muscle via PDE inhibition, unlike dicyclomine and hyoscine which exert anticholinergic effects. This makes drotaverine safer in patients prone to anticholinergic complications such as glaucoma and prostatic hypertrophy.
MCQs (10–15)
- Drotaverine relieves smooth muscle spasm by inhibiting:
a) Cyclooxygenase
b) Phosphodiesterase
c) Acetylcholinesterase
d) Calcium channels directly
Answer: b) Phosphodiesterase
- Drotaverine increases intracellular levels of:
a) Calcium
b) Sodium
c) cAMP
d) cGMP only
Answer: c) cAMP
- The antispasmodic effect of drotaverine is due to:
a) Muscarinic blockade
b) Alpha receptor blockade
c) Reduction in intracellular calcium
d) Increased acetylcholine release
Answer: c) Reduction in intracellular calcium
- Drotaverine differs from dicyclomine because it:
a) Is anticholinergic
b) Acts centrally
c) Has no anticholinergic effects
d) Causes sedation
Answer: c) Has no anticholinergic effects
- Drotaverine is most useful in:
a) Bronchial asthma
b) Dysmenorrhea
c) Hypertension
d) Peptic ulcer disease
Answer: b) Dysmenorrhea
- Which enzyme is selectively inhibited by drotaverine?
a) PDE-1
b) PDE-3
c) PDE-4
d) PDE-5
Answer: c) PDE-4
- Drotaverine relaxes smooth muscle by activating:
a) Protein kinase C
b) Protein kinase A
c) Tyrosine kinase
d) MAP kinase
Answer: b) Protein kinase A
- A major advantage of drotaverine is absence of:
a) Analgesic effect
b) Antispasmodic action
c) Anticholinergic side effects
d) Oral absorption
Answer: c) Anticholinergic side effects
- Drotaverine is primarily eliminated by:
a) Lungs
b) Kidney
c) Skin
d) Saliva
Answer: b) Kidney
- Drotaverine acts directly on:
a) Autonomic nerves
b) Smooth muscle
c) CNS neurons
d) Sensory receptors
Answer: b) Smooth muscle
FAQs (minimum 5)
- What is the primary mechanism of drotaverine?
Inhibition of phosphodiesterase-4 leading to increased cAMP and smooth muscle relaxation. - Does drotaverine have anticholinergic effects?
No, it acts independently of muscarinic receptors. - Why is drotaverine preferred in dysmenorrhea?
It relieves uterine smooth muscle spasm without anticholinergic adverse effects. - Is drotaverine a central muscle relaxant?
No, it acts directly on peripheral smooth muscle. - Can drotaverine be used in glaucoma or BPH?
Yes, it is safer than anticholinergic antispasmodics. - Does drotaverine reduce intestinal motility?
It relieves spasm but does not significantly impair normal motility.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accessmedicine.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
https://www.jaypeebrothers.com - Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com