Table of Contents
Introduction
Diclofenac is a widely used nonsteroidal anti-inflammatory drug (NSAID) belonging to the phenylacetic acid class. It exhibits potent anti-inflammatory, analgesic, and antipyretic properties and is commonly prescribed for musculoskeletal disorders, postoperative pain, arthritis, and dysmenorrhea. Diclofenac is a high-yield NSAID in pharmacology and clinical examinations because of its strong COX inhibition, relative COX-2 preference, and characteristic safety profile.
Mechanism of Action (Step-wise)
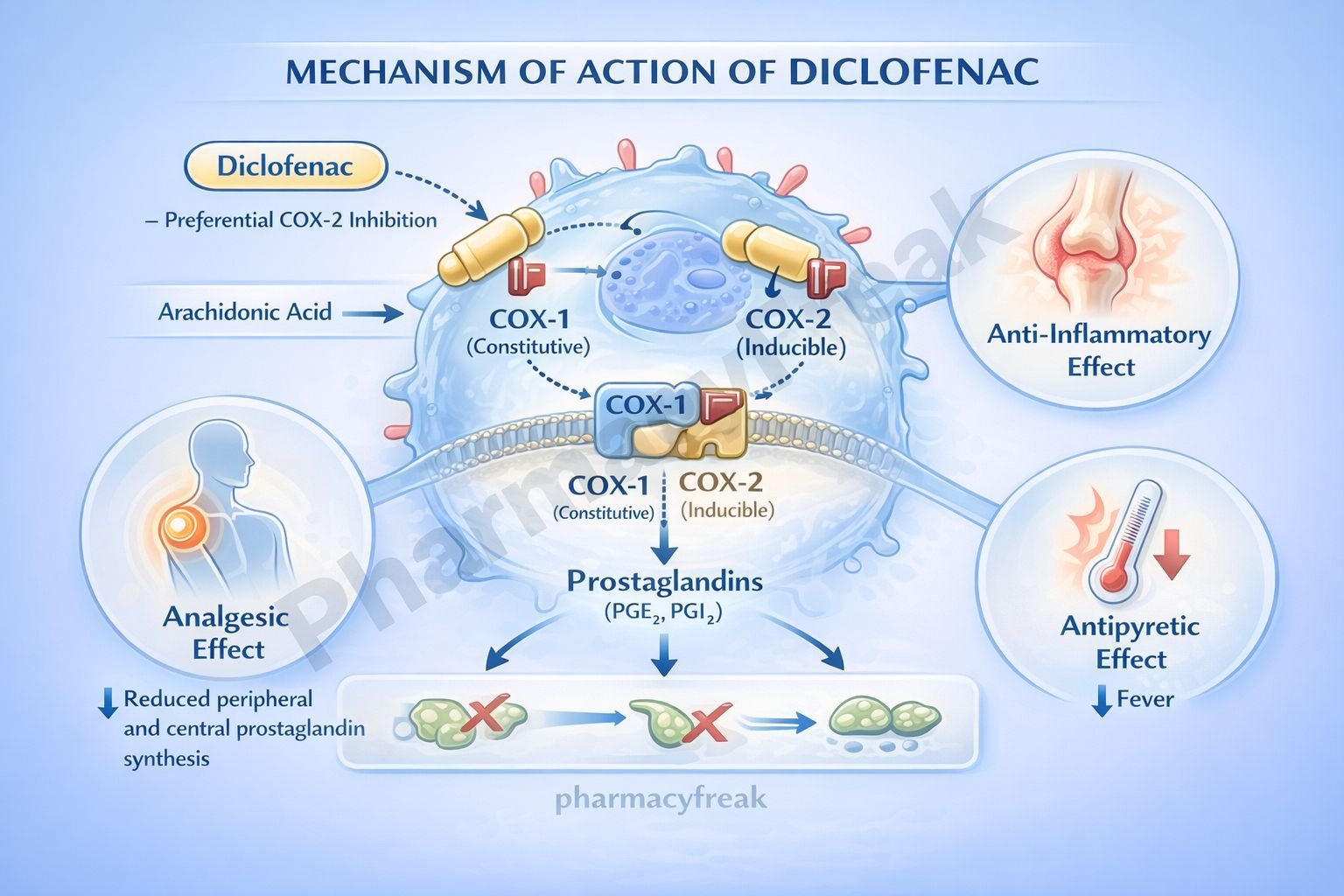
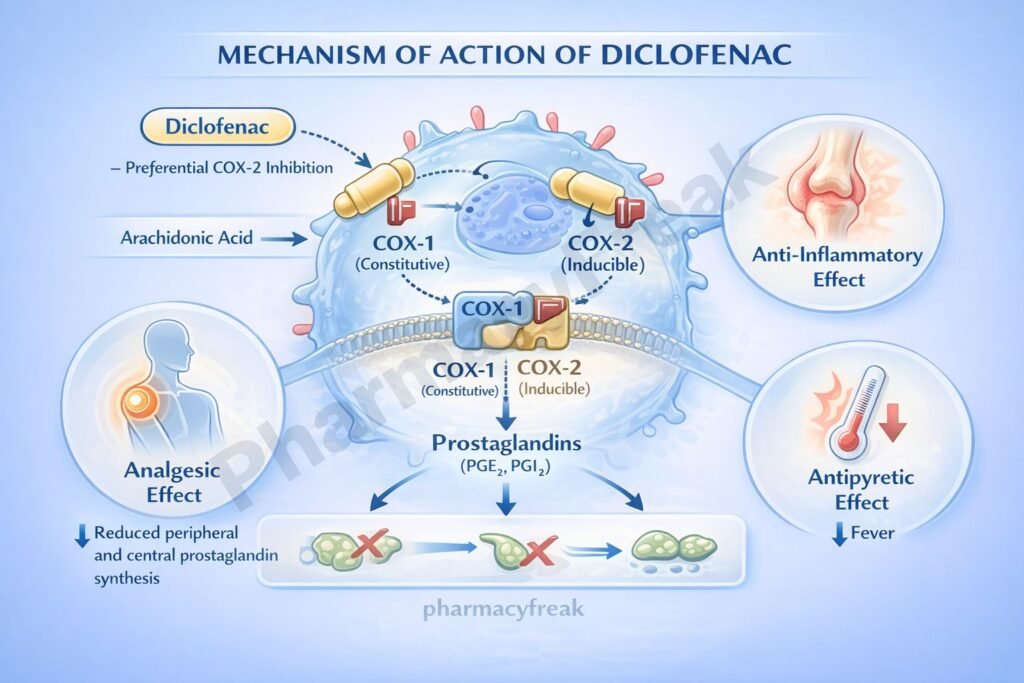
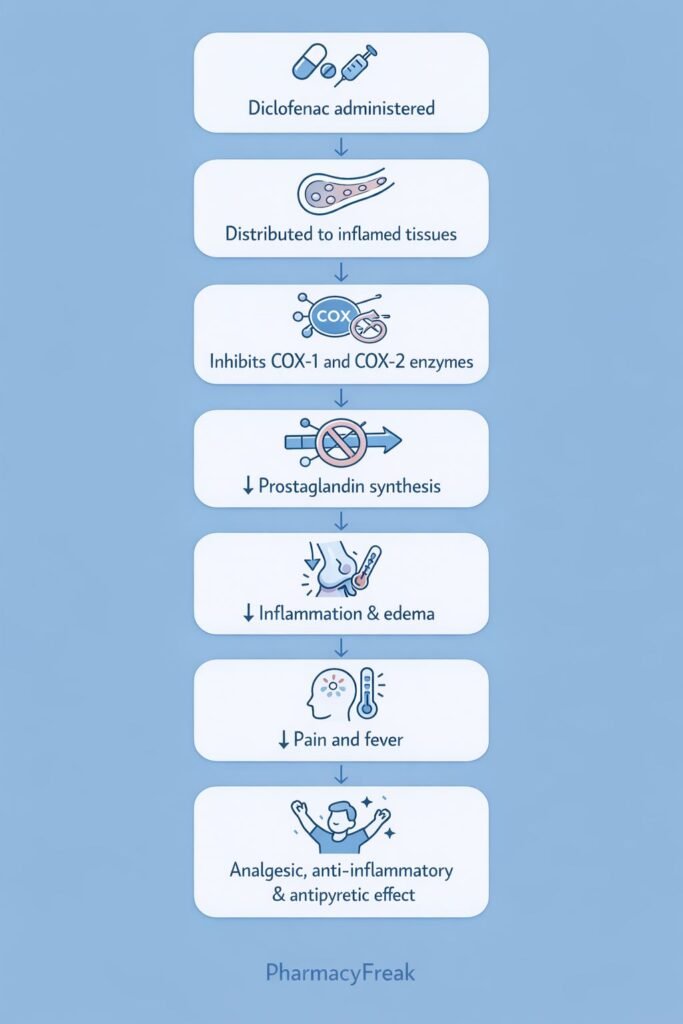
Diclofenac exerts its effects primarily by inhibiting cyclooxygenase-mediated prostaglandin synthesis.
Step-wise mechanism:
- Arachidonic Acid Release
Tissue injury or inflammation activates phospholipase A₂, releasing arachidonic acid from cell membrane phospholipids. - Cyclooxygenase (COX) Enzymes
Arachidonic acid is converted into prostaglandin H₂ by cyclooxygenase enzymes (COX-1 and COX-2). - Inhibition of COX Enzymes
Diclofenac reversibly inhibits both COX-1 and COX-2, with a relatively higher functional selectivity toward COX-2 at therapeutic doses. - Reduced Prostaglandin Synthesis
Inhibition of COX enzymes decreases formation of pro-inflammatory prostaglandins (PGE₂, PGI₂). - Anti-inflammatory Effect
Reduced prostaglandins lead to decreased vasodilation, capillary permeability, and inflammatory mediator sensitization. - Analgesic Effect
Lower prostaglandin levels reduce peripheral and central nociceptor sensitization. - Antipyretic Effect
Inhibition of prostaglandin synthesis in the hypothalamus lowers the fever set point. - Additional Actions
Diclofenac also inhibits leukocyte migration and reduces free radical formation, contributing to its strong anti-inflammatory efficacy.
Pharmacokinetics
- Absorption: Well absorbed orally; also available IM, IV, topical, and rectal
- Bioavailability: ~50% due to first-pass hepatic metabolism
- Distribution: Highly protein bound (>99%)
- Metabolism: Hepatic metabolism (CYP2C9)
- Elimination: Renal and biliary excretion of metabolites
- Half-life: Short plasma half-life (~1–2 hours), but prolonged tissue persistence
Clinical Uses
Diclofenac is widely used in inflammatory and painful conditions:
- Osteoarthritis
- Rheumatoid arthritis
- Ankylosing spondylitis
- Acute musculoskeletal pain
- Postoperative and post-traumatic pain
- Dysmenorrhea
- Migraine (acute attacks)
- Gout (acute attacks, short-term use)
Topical diclofenac is preferred for localized pain to reduce systemic adverse effects.
Adverse Effects
Adverse effects are characteristic of NSAIDs and dose dependent:
- Gastrointestinal:
- Gastritis
- Peptic ulcer disease
- GI bleeding
- Renal:
- Reduced renal perfusion
- Fluid retention
- Cardiovascular:
- Increased risk of thrombotic events (MI, stroke)
- Hepatic:
- Elevated liver enzymes
- Rare hepatotoxicity
- Hypersensitivity:
- Rash
- Bronchospasm (aspirin-sensitive asthma)
Comparative Analysis (must include a table + explanation)
Comparison of Common NSAIDs
| Feature | Diclofenac | Ibuprofen | Celecoxib |
|---|---|---|---|
| COX selectivity | COX-2 > COX-1 (functional) | Non-selective | COX-2 selective |
| Anti-inflammatory potency | High | Moderate | High |
| GI risk | Moderate–High | Moderate | Low |
| CV risk | Moderate–High | Low–Moderate | High |
| Topical availability | Yes | Limited | No |
Explanation:
Diclofenac provides strong anti-inflammatory action comparable to selective COX-2 inhibitors but with higher gastrointestinal and cardiovascular risk. Ibuprofen is safer for short-term use, while celecoxib offers GI protection at the cost of increased cardiovascular risk.
MCQs (10–15)
- Diclofenac exerts its effect primarily by inhibiting:
a) Phospholipase A₂
b) Cyclooxygenase
c) Lipoxygenase
d) Histamine receptors
Answer: b) Cyclooxygenase
- Diclofenac belongs to which drug class?
a) Salicylates
b) Propionic acid derivatives
c) Phenylacetic acid derivatives
d) Oxicams
Answer: c) Phenylacetic acid derivatives
- Diclofenac reduces inflammation by decreasing synthesis of:
a) Leukotrienes
b) Bradykinin
c) Prostaglandins
d) Cytokines directly
Answer: c) Prostaglandins
- The analgesic effect of diclofenac is due to:
a) Opioid receptor activation
b) Reduced nociceptor sensitization
c) NMDA receptor blockade
d) Sodium channel inhibition
Answer: b) Reduced nociceptor sensitization
- Diclofenac has relatively greater inhibition of:
a) COX-1 only
b) COX-2 only
c) COX-2 over COX-1
d) Lipoxygenase
Answer: c) COX-2 over COX-1
- A major gastrointestinal adverse effect of diclofenac is:
a) Constipation
b) Pancreatitis
c) Peptic ulcer
d) Hepatitis
Answer: c) Peptic ulcer
- Diclofenac is contraindicated in patients with:
a) Osteoarthritis
b) Active peptic ulcer disease
c) Migraine
d) Dysmenorrhea
Answer: b) Active peptic ulcer disease
- Diclofenac reduces fever by acting on the:
a) Pituitary gland
b) Cerebellum
c) Hypothalamus
d) Brainstem
Answer: c) Hypothalamus
- Which route reduces systemic adverse effects of diclofenac?
a) Oral
b) Intramuscular
c) Intravenous
d) Topical
Answer: d) Topical
- Diclofenac increases cardiovascular risk primarily by:
a) Platelet activation
b) COX-2 inhibition
c) Sodium retention only
d) Bradycardia
Answer: b) COX-2 inhibition
FAQs (minimum 5)
- What is the primary mechanism of diclofenac?
Inhibition of COX enzymes leading to reduced prostaglandin synthesis. - Is diclofenac COX-2 selective?
It shows functional preference for COX-2 but is not fully selective. - Why does diclofenac cause gastric irritation?
Due to inhibition of COX-1–mediated protective prostaglandins in the stomach. - Does diclofenac affect renal function?
Yes, it can reduce renal prostaglandins and impair renal perfusion. - Is diclofenac safe for long-term use?
Long-term use increases GI, renal, and cardiovascular risks. - Why is topical diclofenac preferred in elderly patients?
To minimize systemic adverse effects.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accessmedicine.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
https://www.jaypeebrothers.com - Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com