Table of Contents
Introduction
Dexamethasone is a long-acting, highly potent synthetic glucocorticoid with negligible mineralocorticoid activity. It is extensively used for its anti-inflammatory, immunosuppressive, anti-edema, and antiemetic properties across multiple specialties, including internal medicine, oncology, neurology, pulmonology, and critical care. Because of its strong genomic effects and long duration of action, dexamethasone is a high-yield corticosteroid in pharmacology and clinical entrance examinations.

Mechanism of Action (Step-wise)
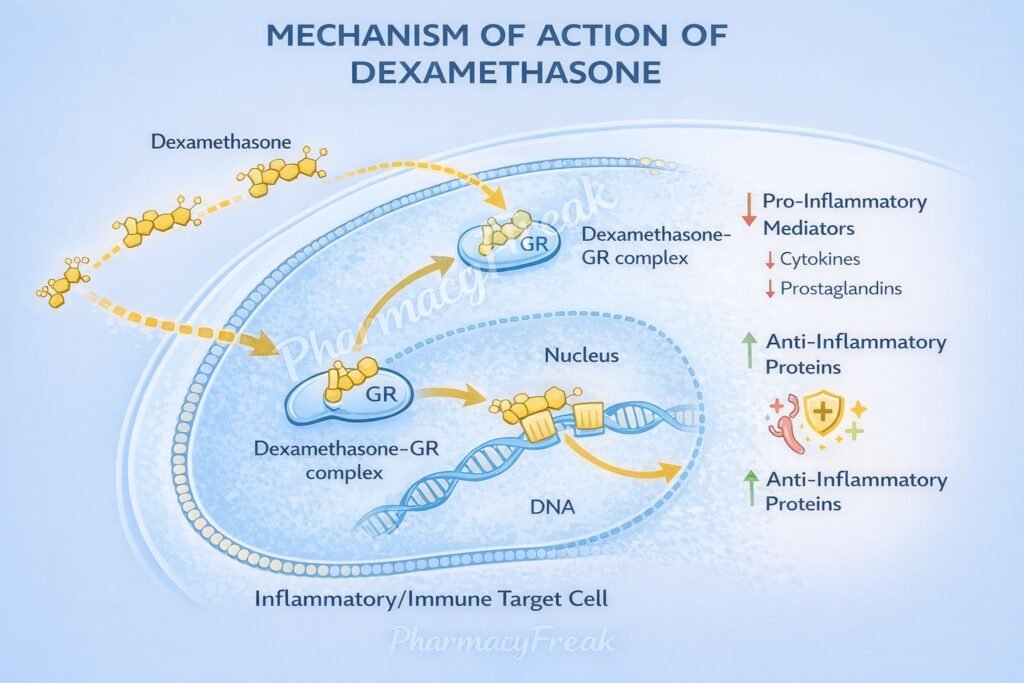
Dexamethasone acts primarily through intracellular glucocorticoid receptor–mediated genomic mechanisms, leading to broad suppression of inflammatory and immune pathways.
Step-wise mechanism:
- Cell Membrane Diffusion
Dexamethasone is lipophilic and freely diffuses across the cell membrane into the cytoplasm. - Binding to Glucocorticoid Receptor (GR)
In the cytoplasm, it binds to inactive glucocorticoid receptors associated with heat-shock proteins (HSPs). - Receptor Activation and Nuclear Translocation
Binding causes dissociation of HSPs, allowing the steroid–receptor complex to translocate into the nucleus. - Interaction with Glucocorticoid Response Elements (GREs)
The complex binds to GREs on DNA, modulating transcription of specific genes. - Upregulation of Anti-inflammatory Proteins
Increased synthesis of:- Lipocortin-1 (annexin A1), which inhibits phospholipase A₂
- Anti-inflammatory cytokines (e.g., IL-10)
- Downregulation of Pro-inflammatory Genes
Suppression of transcription of:- Pro-inflammatory cytokines (IL-1, IL-2, IL-6, TNF-α)
- COX-2
- Inducible nitric oxide synthase (iNOS)
- Inhibition of Arachidonic Acid Cascade
Reduced formation of prostaglandins and leukotrienes leads to powerful anti-inflammatory effects. - Immunosuppression and Anti-edema Effects
Decreased leukocyte migration, capillary permeability, and lymphocyte proliferation result in immunosuppression and reduction of cerebral and tumor-related edema.
Pharmacokinetics
- Absorption: Well absorbed orally; effective IV and IM
- Distribution: Widely distributed; crosses blood–brain barrier and placenta
- Protein binding: Moderate
- Metabolism: Hepatic metabolism
- Elimination: Renal excretion of metabolites
- Plasma half-life: ~4–5 hours
- Biological half-life: 36–72 hours (long-acting)
- Mineralocorticoid activity: Negligible
Clinical Uses
Dexamethasone is used in a wide variety of inflammatory, immune, and oncologic conditions:
- Cerebral edema (brain tumors, head injury)
- Severe allergic and inflammatory disorders
- Autoimmune diseases
- Acute respiratory distress and severe COVID-19
- Antiemetic in chemotherapy-induced nausea and vomiting
- Adjuvant therapy in malignancies (leukemia, lymphoma)
- Diagnostic suppression test for Cushing syndrome
- Prevention of neonatal respiratory distress syndrome
Adverse Effects
Adverse effects depend on dose and duration of therapy:
- Endocrine & metabolic:
- Hyperglycemia
- Cushingoid features
- Adrenal suppression
- Musculoskeletal:
- Osteoporosis
- Proximal myopathy
- Immune:
- Increased infection risk
- Reactivation of latent infections
- Gastrointestinal:
- Peptic ulcer disease
- Neuropsychiatric:
- Mood changes
- Psychosis
Abrupt discontinuation after prolonged use may precipitate acute adrenal insufficiency.
Comparative Analysis (must include a table + explanation)
Comparison of Common Glucocorticoids
| Feature | Dexamethasone | Prednisolone | Hydrocortisone |
|---|---|---|---|
| Anti-inflammatory potency | Very high | Moderate | Low |
| Duration of action | Long | Intermediate | Short |
| Mineralocorticoid activity | Negligible | Low | High |
| Use in cerebral edema | Yes | Limited | No |
| HPA axis suppression | Strong | Moderate | Mild |
Explanation:
Dexamethasone is preferred when potent and sustained anti-inflammatory action is required without fluid retention. Hydrocortisone is used mainly for adrenal replacement, while prednisolone is commonly used for chronic inflammatory conditions.
MCQs (10–15)
- Dexamethasone exerts its effects primarily by:
a) Blocking COX enzymes directly
b) Activating membrane receptors
c) Modulating gene transcription
d) Inhibiting histamine release
Answer: c) Modulating gene transcription
- Dexamethasone binds to which receptor?
a) G-protein–coupled receptor
b) Tyrosine kinase receptor
c) Nuclear glucocorticoid receptor
d) Ion channel receptor
Answer: c) Nuclear glucocorticoid receptor
- The anti-inflammatory effect of dexamethasone involves inhibition of:
a) Phospholipase A₂
b) DNA gyrase
c) Na⁺/K⁺-ATPase
d) Acetylcholinesterase
Answer: a) Phospholipase A₂
- Dexamethasone has minimal mineralocorticoid activity, so it causes:
a) Sodium retention
b) Potassium retention
c) Minimal fluid retention
d) Severe hypertension
Answer: c) Minimal fluid retention
- Which condition is dexamethasone especially useful for?
a) Addison disease
b) Cerebral edema
c) Hypotension
d) Heart failure
Answer: b) Cerebral edema
- Dexamethasone reduces prostaglandin synthesis by:
a) Direct COX inhibition
b) Reducing arachidonic acid availability
c) Blocking prostaglandin receptors
d) Increasing lipoxygenase activity
Answer: b) Reducing arachidonic acid availability
- Long-term dexamethasone therapy may cause:
a) Hyperkalemia
b) Osteoporosis
c) Hypoglycemia
d) Bradycardia
Answer: b) Osteoporosis
- Dexamethasone suppresses immunity mainly by inhibiting:
a) Neutrophil migration and T-cell function
b) Antibody degradation
c) Complement activation
d) Mast cell stabilization
Answer: a) Neutrophil migration and T-cell function
- Dexamethasone is classified as a:
a) Mineralocorticoid
b) Short-acting glucocorticoid
c) Long-acting glucocorticoid
d) NSAID
Answer: c) Long-acting glucocorticoid
- Abrupt withdrawal of dexamethasone can lead to:
a) Thyroid storm
b) Neuroleptic malignant syndrome
c) Adrenal insufficiency
d) Serotonin syndrome
Answer: c) Adrenal insufficiency
FAQs (minimum 5)
- What is the primary mechanism of dexamethasone?
Genomic modulation of inflammatory and immune gene transcription via glucocorticoid receptors. - Why is dexamethasone preferred in cerebral edema?
Due to its strong anti-edema effect and minimal mineralocorticoid activity. - Does dexamethasone act faster than NSAIDs?
No, its onset is slower because it requires gene transcription. - Why must dexamethasone be tapered?
To prevent adrenal insufficiency from HPA axis suppression. - Does dexamethasone cause fluid retention?
Minimal, because it has negligible mineralocorticoid activity. - Is dexamethasone immunosuppressive?
Yes, it strongly suppresses both innate and adaptive immunity.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accessmedicine.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
https://www.jaypeebrothers.com - Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com

