Table of Contents
Introduction
Clonazepam is a high-potency benzodiazepine derivative used primarily for its anticonvulsant and anxiolytic properties. First patented in 1964 and appearing in clinical use by 1975, it belongs to the nitro-benzodiazepine class. Clonazepam is widely utilized in the management of seizure disorders, including Lennox-Gastaut syndrome, akinetic, and myoclonic seizures, as well as panic disorder with or without agoraphobia. Unlike shorter-acting benzodiazepines, clonazepam has a long half-life and a rapid onset of action, making it effective for both acute symptom control and long-term prophylaxis. Its primary clinical value lies in its ability to suppress the spike-and-wave discharge in absence seizures and decrease the frequency, amplitude, and duration of minor motor seizures.

Mechanism of Action (Step-wise)
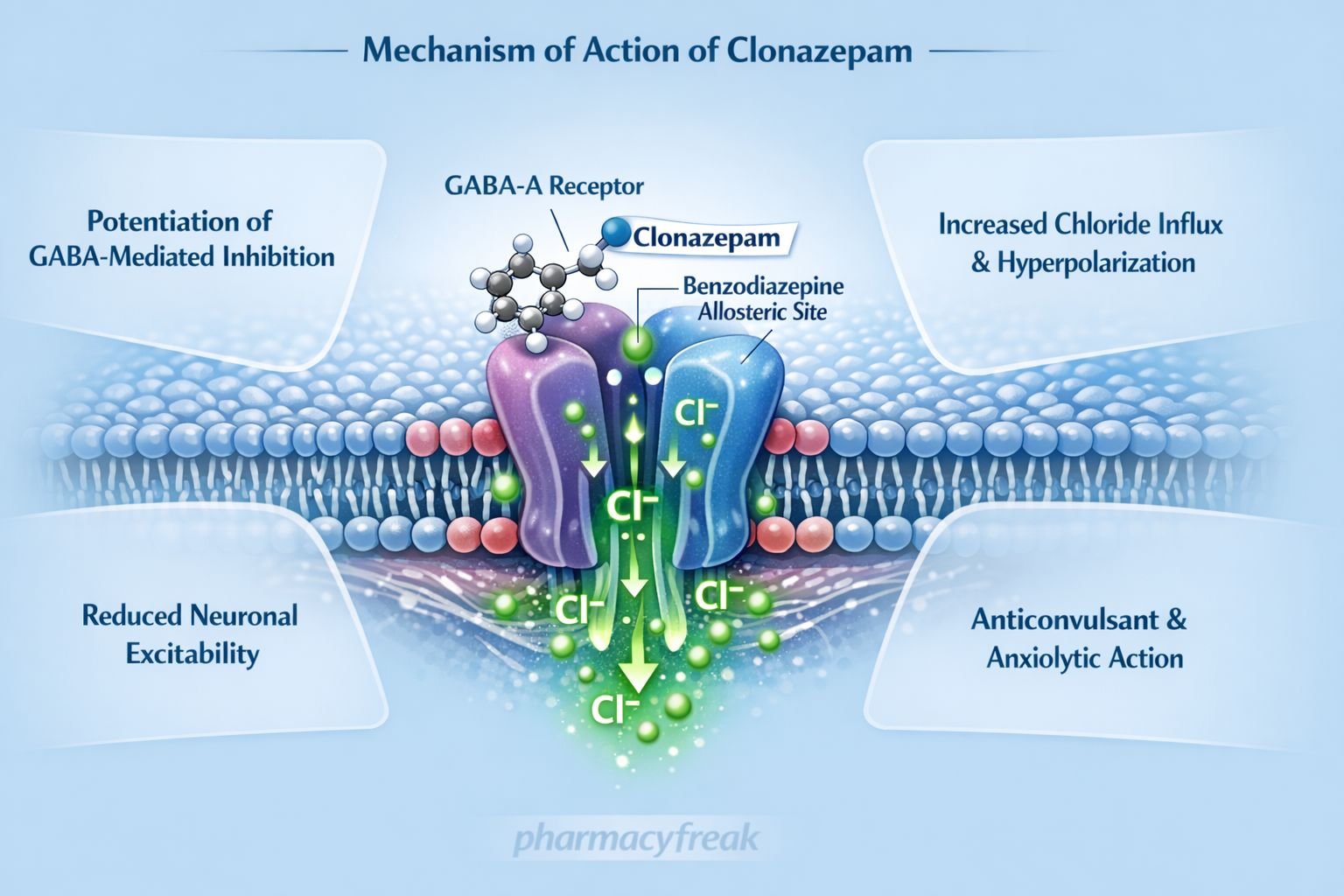
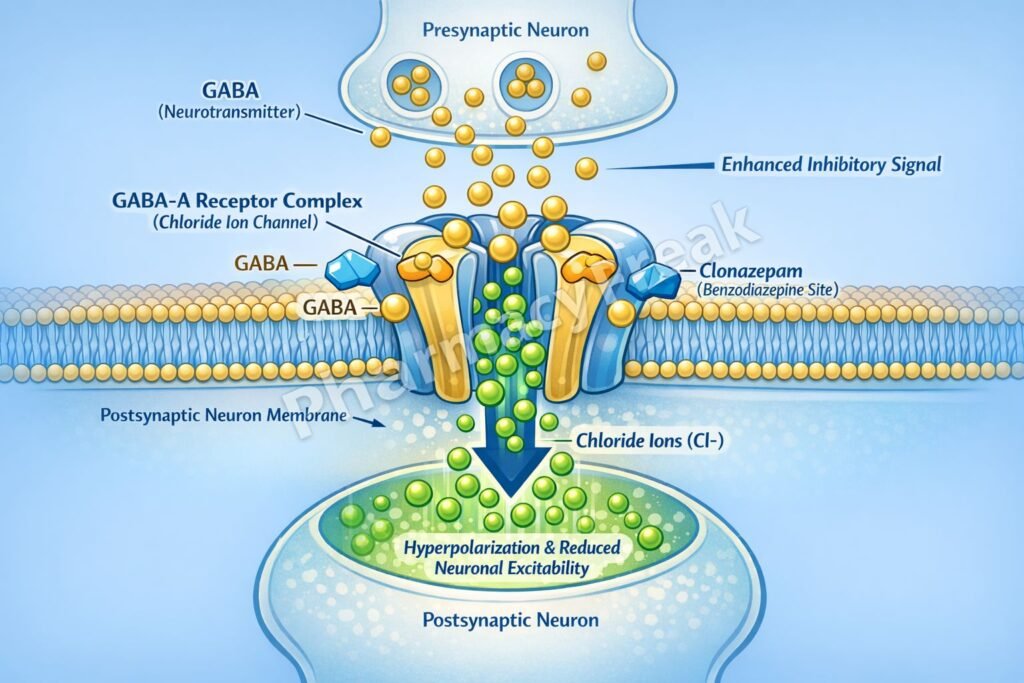
The mechanism of action of Clonazepam involves the potentiation of the major inhibitory neurotransmitter in the central nervous system (CNS), Gamma-Aminobutyric Acid (GABA).
- Binding to GABA-A Receptors: Clonazepam binds to a specific site on the GABAA receptor complex, located at the interface of the α and γ subunits. This site is distinct from the primary GABA binding site.
- Allosteric Modulation: By binding to this site, clonazepam acts as a positive allosteric modulator. It does not activate the receptor directly but increases the receptor’s affinity for endogenous GABA.
- Increased Chloride Channel Opening: When GABA binds in the presence of clonazepam, there is an increase in the frequency of the chloride channel opening events.
- Hyperpolarization: The increased frequency of channel opening leads to a greater influx of chloride ions (Cl−) into the post-synaptic neuron. This negative ion influx causes hyperpolarization of the neuronal membrane.
- Neuronal Inhibition: Hyperpolarization shifts the membrane potential further away from the firing threshold, making the neuron less excitable. In the context of epilepsy, this raises the seizure threshold and limits the spread of electrical discharge in the brain.
Pharmacokinetics
- Absorption: Clonazepam is rapidly and completely absorbed after oral administration, with bioavailability reaching approximately 90%. Peak plasma concentrations occur within 1 to 4 hours.
- Distribution: It is highly lipophilic and crosses the blood-brain barrier easily. It is approximately 85% bound to plasma proteins.
- Metabolism: It undergoes extensive hepatic metabolism, primarily via CYP3A4. The main metabolic pathway involves the reduction of the 7-nitro group to form 7-amino-clonazepam, which has little to no pharmacological activity.
- Excretion: Metabolites are excreted mainly in the urine. The elimination half-life is long, ranging from 30 to 40 hours, which allows for twice-daily dosing in many patients.
Clinical Uses
- Seizure Disorders: Used as monotherapy or adjunct therapy for absence seizures (petit mal), myoclonic seizures, and Lennox-Gastaut syndrome.
- Panic Disorder: Effective in the short-term and long-term management of panic attacks and associated agoraphobia.
- Akathisia: Sometimes used to treat movement disorders and restlessness induced by neuroleptic medications.
- Status Epilepticus: Occasionally used as a second-line agent if other benzodiazepines are unavailable, though IV formulations are preferred for acute status.
Adverse Effects
- CNS Depression: Drowsiness, sedation, ataxia, and dizziness are the most common side effects, particularly at the start of therapy.
- Respiratory Depression: Can occur at high doses or when combined with other CNS depressants like alcohol or opioids.
- Cognitive Impairment: Long-term use may lead to memory disturbances, confusion, and reduced concentration.
- Paradoxical Reactions: Rarely, it may cause increased aggression, irritability, or agitation, especially in pediatric or elderly patients.
- Dependence and Withdrawal: Prolonged use carries a high risk of physical and psychological dependence. Abrupt discontinuation can trigger severe withdrawal symptoms, including seizures.
Comparative Analysis
| Feature | Clonazepam | Diazepam |
| Potency | High (0.5 mg equivalent) | Moderate (10 mg equivalent) |
| Primary Use | Anticonvulsant / Panic Disorder | Muscle Relaxant / Status Epilepticus |
| Half-life | Long (30–40 hours) | Very Long (20–100 hours with metabolites) |
| Metabolism | Nitro-reduction (7-amino) | Dealkylation & Hydroxylation (Active metabolites) |
| Onset of Action | Intermediate to Rapid | Very Rapid |
Explanation: Clonazepam is preferred over Diazepam for long-term seizure prophylaxis and panic disorder due to its higher potency at the GABAA receptor and its lack of long-acting active metabolites that can accumulate excessively, although its own half-life remains significant.
MCQs
- Clonazepam primarily acts by increasing the frequency of opening of which ion channel?
a) Sodium channel b) Potassium channel c) Chloride channel d) Calcium channel
Answer: c) Chloride channel
- To which specific receptor does Clonazepam bind to exert its effect?
a) GABAB receptor b) NMDA receptor c) GABAA receptor d) Alpha-2 adrenergic receptor
Answer: c) GABAA receptor
- Which hepatic enzyme is primarily responsible for the metabolism of Clonazepam?
a) CYP2D6 b) CYP3A4 c) CYP2C19 d) CYP1A2
Answer: b) CYP3A4
- What is the characteristic effect of benzodiazepines like Clonazepam on GABA receptor kinetics?
a) Increase in channel opening duration b) Increase in channel opening frequency c) Decrease in GABA binding affinity d) Direct activation without GABA
Answer: b) Increase in channel opening frequency
- Clonazepam is chemically classified as a:
a) Imidazopyridine b) Nitro-benzodiazepine c) Triazolo-benzodiazepine d) Barbiturate
Answer: b) Nitro-benzodiazepine
- Which of the following is a major clinical indication for Clonazepam?
a) Schizophrenia b) Lennox-Gastaut syndrome c) Hypertension d) Major Depressive Disorder
Answer: b) Lennox-Gastaut syndrome
- The elimination half-life of Clonazepam is approximately:
a) 2 to 4 hours b) 6 to 12 hours c) 30 to 40 hours d) Over 100 hours
Answer: c) 30 to 40 hours
- Benzodiazepines bind to the GABAA receptor at the interface of which subunits?
a) α and β b) β and γ c) α and γ d) δ and ϵ
Answer: c) α and γ
- Abrupt withdrawal of Clonazepam after chronic use most likely results in:
a) Respiratory failure b) Rebound hypertension c) Seizures d) Bradycardia
Answer: c) Seizures
- Which drug can be used to reverse the effects of Clonazepam in case of an overdose?
a) Naloxone b) Flumazenil c) N-acetylcysteine d) Physostigmine
Answer: b) Flumazenil
FAQs
- How does Clonazepam differ from Alprazolam? Clonazepam has a much longer half-life (30–40 hours) compared to Alprazolam (11–15 hours), making it more suitable for consistent coverage in seizure prevention and panic disorder.
- Can Clonazepam be used for sleep? While it causes sedation, it is not primarily indicated as a hypnotic for insomnia due to its long duration of action, which can lead to significant daytime grogginess.
- What happens if you take alcohol with Clonazepam? Alcohol synergistically potentiates the CNS depressant effects of clonazepam, which can lead to severe respiratory depression, coma, or death.
- Is Clonazepam safe during pregnancy? Benzodiazepines are generally avoided in pregnancy as they cross the placenta and may be associated with an increased risk of cleft lip/palate or neonatal withdrawal syndrome.
- Why is it called a “high-potency” benzodiazepine? It is considered high-potency because very small doses (e.g., 0.25 mg to 0.5 mg) produce significant clinical effects compared to drugs like diazepam, which require 5 mg to 10 mg.
References
- Goodman & Gilman’s Pharmacological Basis of Therapeutics
- Katzung: Basic and Clinical Pharmacology
- Tripathi: Essentials of Medical Pharmacology

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com