Table of Contents
Introduction
Clindamycin is a lincosamide antibiotic primarily used for the treatment of anaerobic bacterial infections and infections caused by Gram-positive cocci, including Staphylococcus aureus and Streptococcus species. It is especially important in clinical practice for skin and soft tissue infections, intra-abdominal infections, pelvic infections, and as an alternative agent in penicillin-allergic patients. Clindamycin is frequently tested in pharmacology and microbiology examinations due to its unique ribosomal binding site, anaerobic coverage, and association with Clostridioides difficile infection.
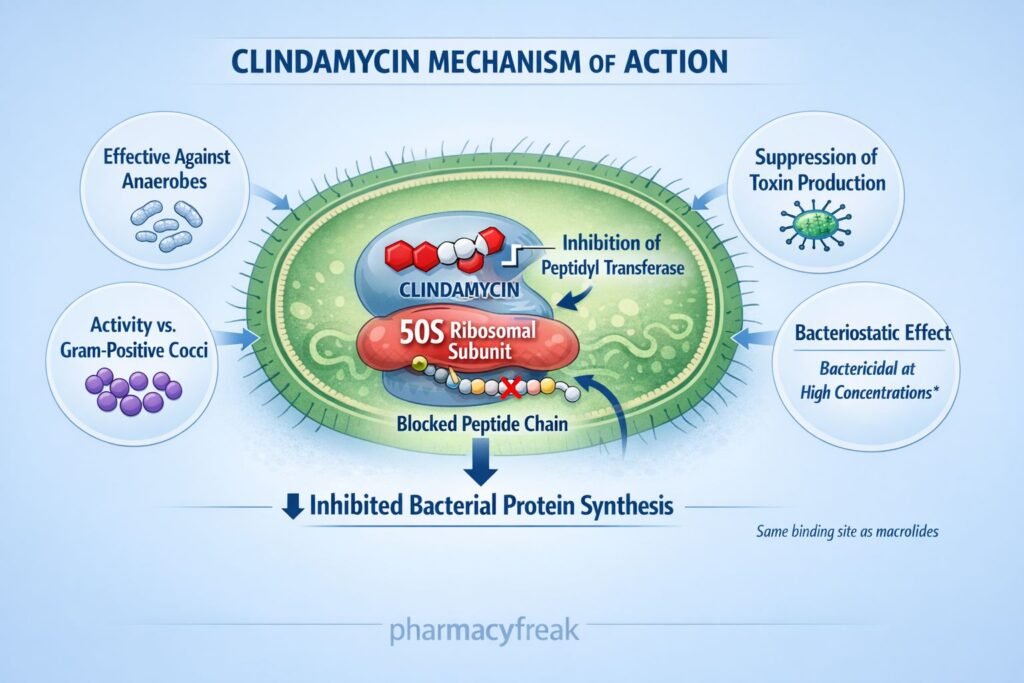
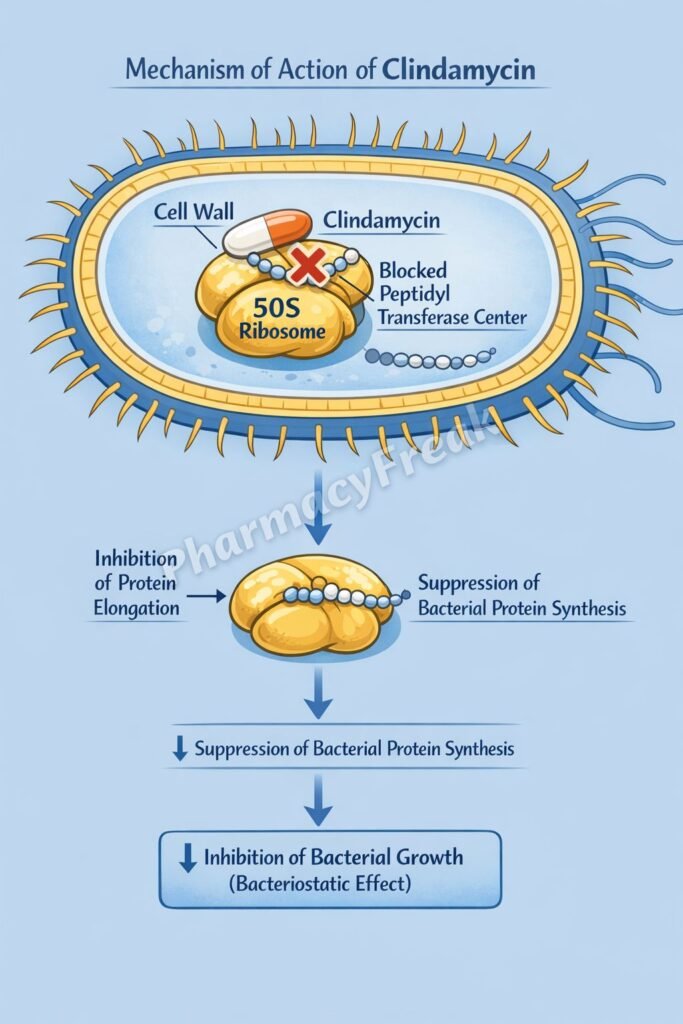
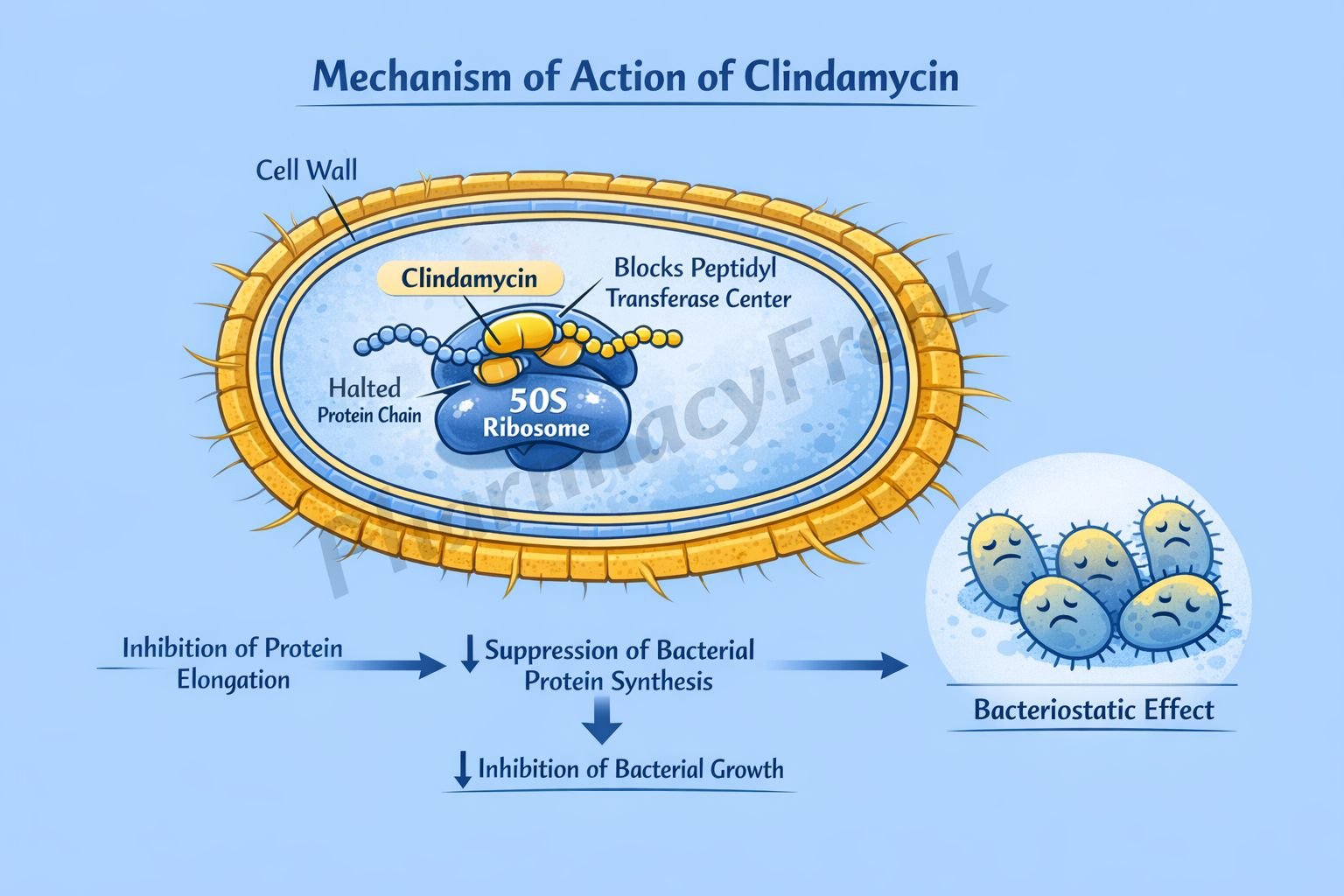
Mechanism of Action (Step-wise)
Clindamycin inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit.
Step-wise mechanism:
- Bacterial Ribosome Structure
Bacterial ribosomes consist of a 30S and a 50S subunit, which together facilitate protein synthesis. - Binding to 50S Ribosomal Subunit
Clindamycin binds reversibly to the 50S ribosomal subunit at a site overlapping with macrolides. - Inhibition of Peptidyl Transferase
Binding interferes with the peptidyl transferase reaction, which is essential for peptide bond formation. - Prevention of Translocation
Clindamycin inhibits translocation of the growing peptide chain from the A site to the P site on the ribosome. - Suppression of Protein Elongation
As a result, bacterial protein synthesis is halted. - Bacteriostatic Effect
The inhibition of protein synthesis leads to a bacteriostatic effect, though it may be bactericidal against certain highly susceptible organisms at high concentrations.
Pharmacokinetics
- Absorption: Well absorbed orally
- Bioavailability: Approximately 90%
- Distribution: Widely distributed in tissues and bone; poor CSF penetration
- Metabolism: Hepatic metabolism
- Elimination: Biliary and renal excretion
- Half-life: Approximately 2–3 hours (prolonged in hepatic impairment)
- Special feature: Excellent penetration into abscesses and necrotic tissue
Dose adjustment is required in severe hepatic dysfunction.
Clinical Uses
Clindamycin is commonly used for infections caused by anaerobic and Gram-positive organisms:
- Anaerobic infections (e.g., Bacteroides fragilis)
- Skin and soft tissue infections
- Necrotizing fasciitis (as adjunct therapy to suppress toxin production)
- Dental infections
- Pelvic inflammatory disease
- Aspiration pneumonia
- Alternative to penicillin in penicillin-allergic patients
Adverse Effects
Clinically important adverse effects include:
- Gastrointestinal:
- Diarrhea
- Nausea
- Abdominal pain
- Clostridioides difficile–associated colitis (most significant adverse effect)
- Rash
- Elevated liver enzymes
- Rare hematologic effects (neutropenia)
Clindamycin is one of the antibiotics most strongly associated with antibiotic-associated pseudomembranous colitis.
Comparative Analysis (must include a table + explanation)
Comparison of Protein Synthesis Inhibitors
| Feature | Clindamycin | Macrolides | Tetracyclines |
|---|---|---|---|
| Ribosomal subunit | 50S | 50S | 30S |
| Anaerobic coverage | Excellent | Poor | Moderate |
| C. difficile risk | High | Moderate | Low |
| Bone penetration | Excellent | Moderate | Good |
| Common use | Anaerobic, SSTI | Respiratory | Broad-spectrum |
Explanation:
Clindamycin is particularly valuable for anaerobic infections and toxin suppression in severe streptococcal infections. However, its high risk of C. difficile–associated diarrhea limits routine use compared to other protein synthesis inhibitors.
MCQs (10–15)
- Clindamycin inhibits bacterial protein synthesis by binding to:
a) 30S ribosomal subunit
b) 40S ribosomal subunit
c) 50S ribosomal subunit
d) DNA gyrase
Answer: c) 50S ribosomal subunit
- The primary action of clindamycin is inhibition of:
a) DNA replication
b) Cell wall synthesis
c) Protein elongation
d) Folate synthesis
Answer: c) Protein elongation
- Clindamycin is classified as a:
a) Macrolide
b) Lincosamide
c) Aminoglycoside
d) Fluoroquinolone
Answer: b) Lincosamide
- Which infection is clindamycin especially useful for?
a) Urinary tract infection
b) Anaerobic infection
c) Viral pneumonia
d) Tuberculosis
Answer: b) Anaerobic infection
- The most serious adverse effect of clindamycin is:
a) Nephrotoxicity
b) Ototoxicity
c) Pseudomembranous colitis
d) QT prolongation
Answer: c) Pseudomembranous colitis
- Clindamycin shares a ribosomal binding site with:
a) Aminoglycosides
b) Fluoroquinolones
c) Macrolides
d) Rifampicin
Answer: c) Macrolides
- Clindamycin is mainly metabolized in the:
a) Kidney
b) Liver
c) Lungs
d) Intestine
Answer: b) Liver
- Clindamycin is primarily bacteriostatic because it:
a) Kills bacteria directly
b) Inhibits cell wall formation
c) Inhibits protein synthesis
d) Inhibits RNA polymerase
Answer: c) Inhibits protein synthesis
- Which organism is typically sensitive to clindamycin?
a) Escherichia coli
b) Pseudomonas aeruginosa
c) Bacteroides fragilis
d) Mycoplasma pneumoniae
Answer: c) Bacteroides fragilis
- Clindamycin is often added in necrotizing fasciitis to:
a) Increase renal clearance
b) Suppress toxin production
c) Enhance immune response
d) Increase bacterial growth
Answer: b) Suppress toxin production
FAQs (minimum 5)
- What is the primary mechanism of clindamycin?
It inhibits bacterial protein synthesis by binding to the 50S ribosomal subunit. - Is clindamycin bactericidal or bacteriostatic?
It is primarily bacteriostatic. - Why is clindamycin associated with C. difficile infection?
It disrupts normal gut flora, allowing C. difficile overgrowth. - Does clindamycin cover Gram-negative aerobes?
No, it has poor activity against Gram-negative aerobic bacteria. - Can clindamycin be used in penicillin-allergic patients?
Yes, it is commonly used as an alternative. - Why is clindamycin useful in bone infections?
Due to excellent bone penetration.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accessmedicine.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
https://www.jaypeebrothers.com - Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com