Table of Contents
Introduction
Cimetidine is a first-generation histamine H₂-receptor antagonist (H₂ blocker) widely used in the management of acid-related gastrointestinal disorders. It was the first clinically successful H₂ receptor antagonist and marked a major advance in the treatment of peptic ulcer disease by directly reducing gastric acid secretion. Although newer H₂ blockers and proton pump inhibitors (PPIs) have largely replaced it due to safety and interaction concerns, cimetidine remains pharmacologically important and is frequently tested in medical and pharmacy entrance and licensure examinations.
Mechanism of Action (Step-wise)
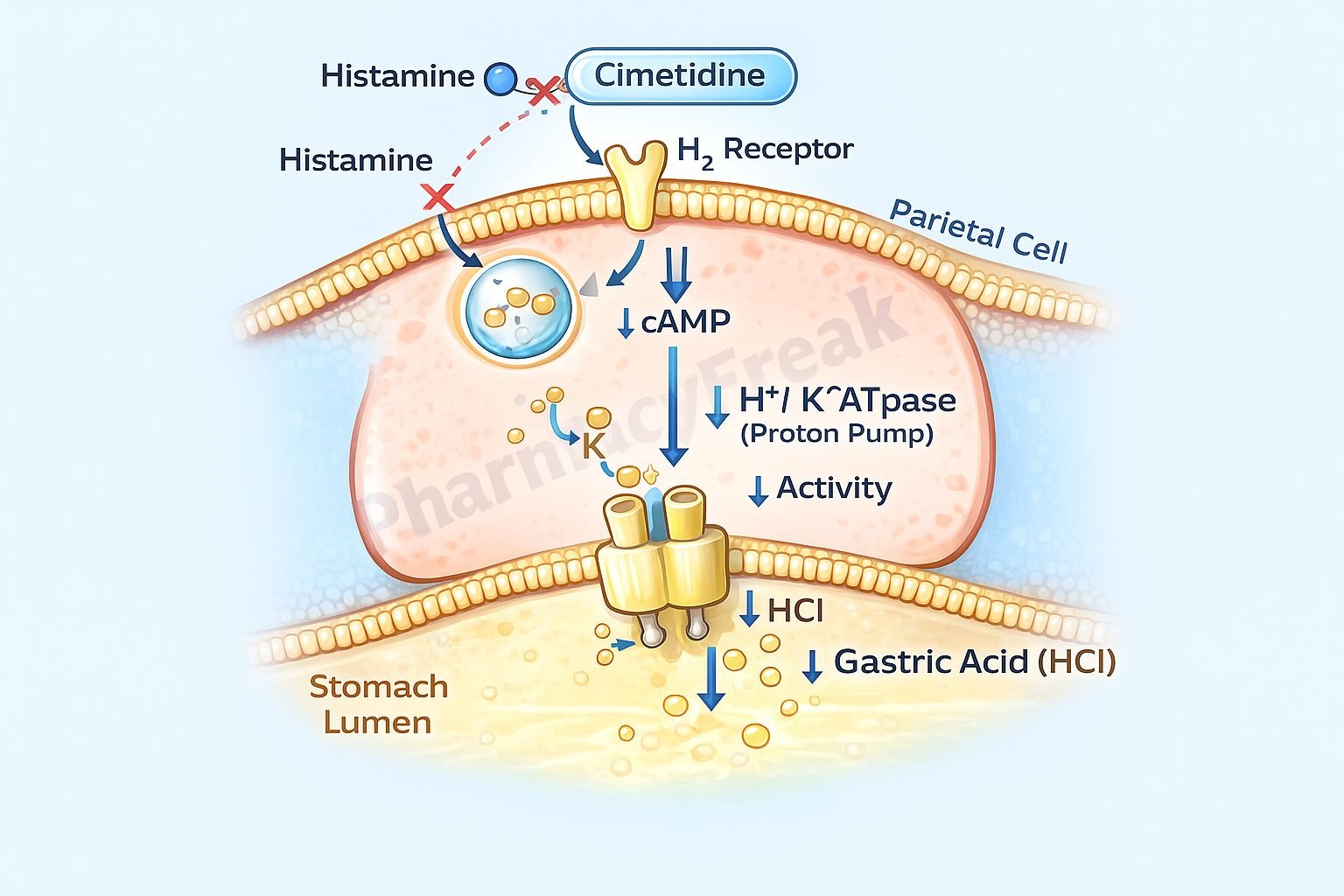
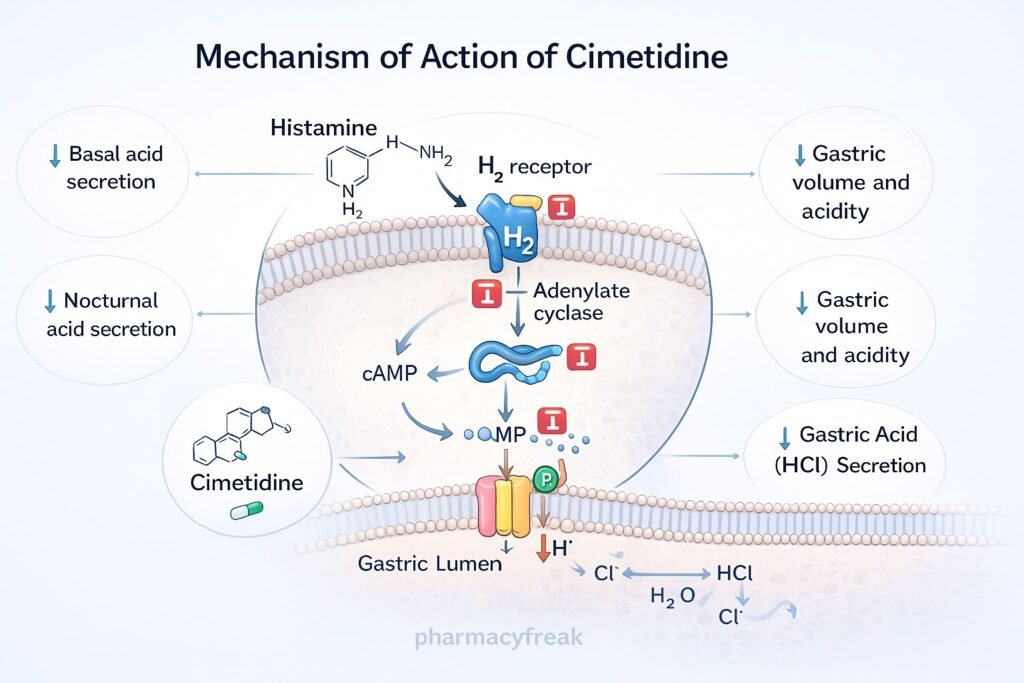
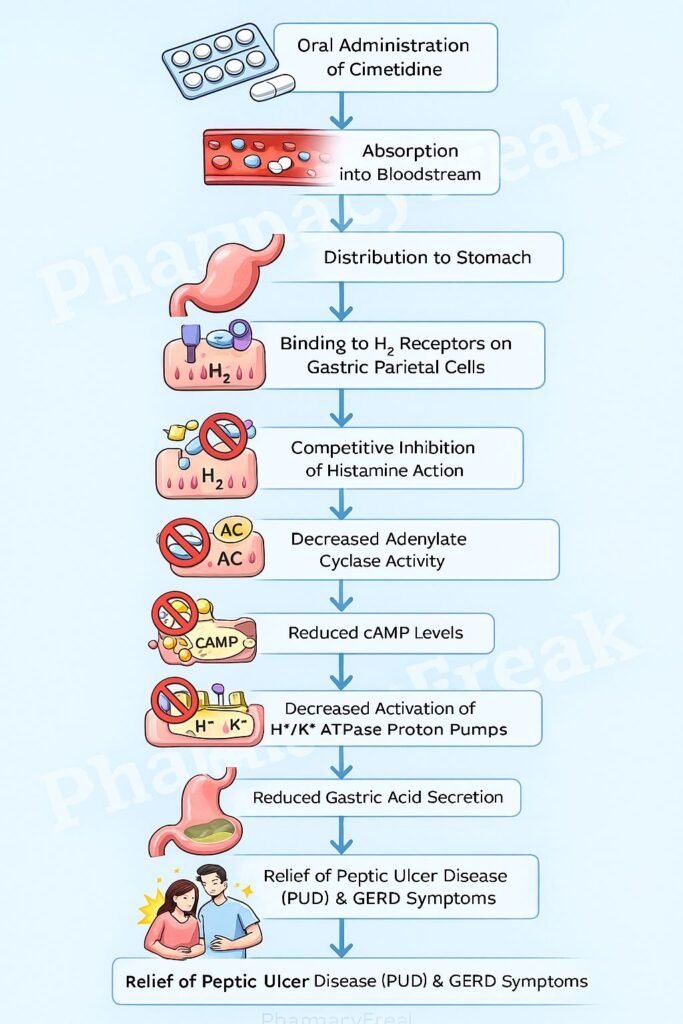
Cimetidine reduces gastric acid secretion by selectively and competitively inhibiting histamine H₂ receptors on gastric parietal cells.
Step-wise mechanism:
- Histamine Release
Histamine is released from enterochromaffin-like (ECL) cells in the gastric mucosa in response to gastrin and vagal stimulation. - H₂ Receptor Activation
Histamine binds to H₂ receptors located on the basolateral membrane of gastric parietal cells. - Adenylate Cyclase Activation
H₂ receptor activation stimulates adenylate cyclase via Gs protein coupling, increasing intracellular cyclic AMP (cAMP). - Proton Pump Activation
Increased cAMP activates protein kinase A, which enhances the activity of the H⁺/K⁺-ATPase (proton pump) on the luminal surface of parietal cells. - Competitive H₂ Blockade by Cimetidine
Cimetidine competitively blocks H₂ receptors, preventing histamine-induced cAMP generation. - Reduced Acid Secretion
This results in decreased basal, nocturnal, and stimulated (food-induced) gastric acid secretion, along with reduced gastric volume and hydrogen ion concentration.
Pharmacokinetics
- Absorption: Well absorbed orally; bioavailability approximately 60–70%
- Distribution: Widely distributed; crosses the blood–brain barrier and placenta
- Metabolism: Partial hepatic metabolism
- Elimination: Primarily renal excretion (unchanged drug)
- Half-life: Approximately 2 hours (prolonged in renal impairment)
- Onset of action: Within 1 hour
- Duration of action: 4–6 hours
Dose adjustment is required in patients with renal dysfunction.
Clinical Uses
Cimetidine is used in the treatment and prevention of acid-related disorders, including:
- Peptic ulcer disease (gastric and duodenal ulcers)
- Gastroesophageal reflux disease (GERD)
- Zollinger–Ellison syndrome
- Stress ulcer prophylaxis in critically ill patients
- Prevention of aspiration pneumonitis (preoperative use)
Due to drug–drug interactions and endocrine adverse effects, its use has declined in favor of newer agents.
Adverse Effects
Cimetidine is associated with several notable adverse effects:
- Endocrine effects:
- Gynecomastia
- Decreased libido
- Impotence
(due to antiandrogenic effects and inhibition of estradiol metabolism)
- Central nervous system:
- Confusion (especially in elderly or renal impairment)
- Dizziness
- Gastrointestinal:
- Diarrhea
- Constipation
- Hematologic (rare):
- Thrombocytopenia
- Neutropenia
- Drug interactions:
- Potent inhibitor of CYP450 enzymes (CYP1A2, CYP2C9, CYP2D6, CYP3A4)
Comparative Analysis (must include a table + explanation)
Comparison of Acid-Suppressing Drugs
| Feature | Cimetidine | Ranitidine | Famotidine | Proton Pump Inhibitors |
|---|---|---|---|---|
| Drug class | H₂ blocker | H₂ blocker | H₂ blocker | PPI |
| Potency | Lowest | Moderate | Highest | Very high |
| CYP450 inhibition | Strong | Minimal | Negligible | Minimal |
| Endocrine effects | Present | Rare | Absent | Absent |
| Duration of action | Short | Moderate | Long | Longest |
| Clinical preference | Rarely used | Limited | Preferred H₂ blocker | First-line therapy |
Explanation:
Cimetidine is less potent and has more adverse effects compared to newer H₂ blockers like famotidine. PPIs are superior in acid suppression and ulcer healing, making them the preferred agents in most clinical settings. However, cimetidine remains relevant for exam questions due to its unique CYP450 inhibition and antiandrogenic effects.
MCQs (10–15)
- Cimetidine reduces gastric acid secretion by blocking which receptor?
a) H₁
b) H₂
c) M₃
d) CCK₂
Answer: b) H₂
- The primary intracellular messenger reduced by cimetidine is:
a) IP₃
b) DAG
c) cAMP
d) Calcium
Answer: c) cAMP
- Which enzyme system is inhibited by cimetidine leading to drug interactions?
a) MAO
b) COX
c) CYP450
d) COMT
Answer: c) CYP450
- Which adverse effect is characteristic of cimetidine?
a) Ototoxicity
b) Gynecomastia
c) Nephrotoxicity
d) Photosensitivity
Answer: b) Gynecomastia
- Cimetidine primarily reduces which type of acid secretion?
a) Basal only
b) Stimulated only
c) Basal and nocturnal
d) Pancreatic
Answer: c) Basal and nocturnal
- Which H₂ blocker has the least CYP450 inhibition?
a) Cimetidine
b) Ranitidine
c) Famotidine
d) Nizatidine
Answer: c) Famotidine
- Cimetidine crosses the blood–brain barrier and may cause:
a) Seizures
b) Confusion
c) Ataxia
d) Tremors
Answer: b) Confusion
- The antiandrogenic effect of cimetidine is due to:
a) Androgen receptor activation
b) Increased testosterone synthesis
c) Estrogen metabolism inhibition
d) Aldosterone suppression
Answer: c) Estrogen metabolism inhibition
- Which condition requires dose adjustment of cimetidine?
a) Liver cirrhosis
b) Renal failure
c) Heart failure
d) Diabetes
Answer: b) Renal failure
- Cimetidine is least preferred today mainly because of:
a) Low bioavailability
b) Severe hepatotoxicity
c) Drug interactions
d) Poor efficacy
Answer: c) Drug interactions
FAQs (minimum 5)
- Is cimetidine a competitive inhibitor?
Yes, cimetidine competitively inhibits histamine at H₂ receptors on parietal cells. - Why is cimetidine rarely used today?
Due to CYP450 inhibition, endocrine side effects, and availability of safer alternatives. - Does cimetidine affect gastrin levels?
It may cause a mild increase due to reduced acid-mediated feedback inhibition. - Can cimetidine cause hormonal side effects?
Yes, it has antiandrogenic effects leading to gynecomastia and impotence. - Which acid suppressant is preferred over cimetidine?
Proton pump inhibitors and famotidine are preferred.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accessmedicine.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
https://www.jaypeebrothers.com - Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com