Table of Contents
Introduction
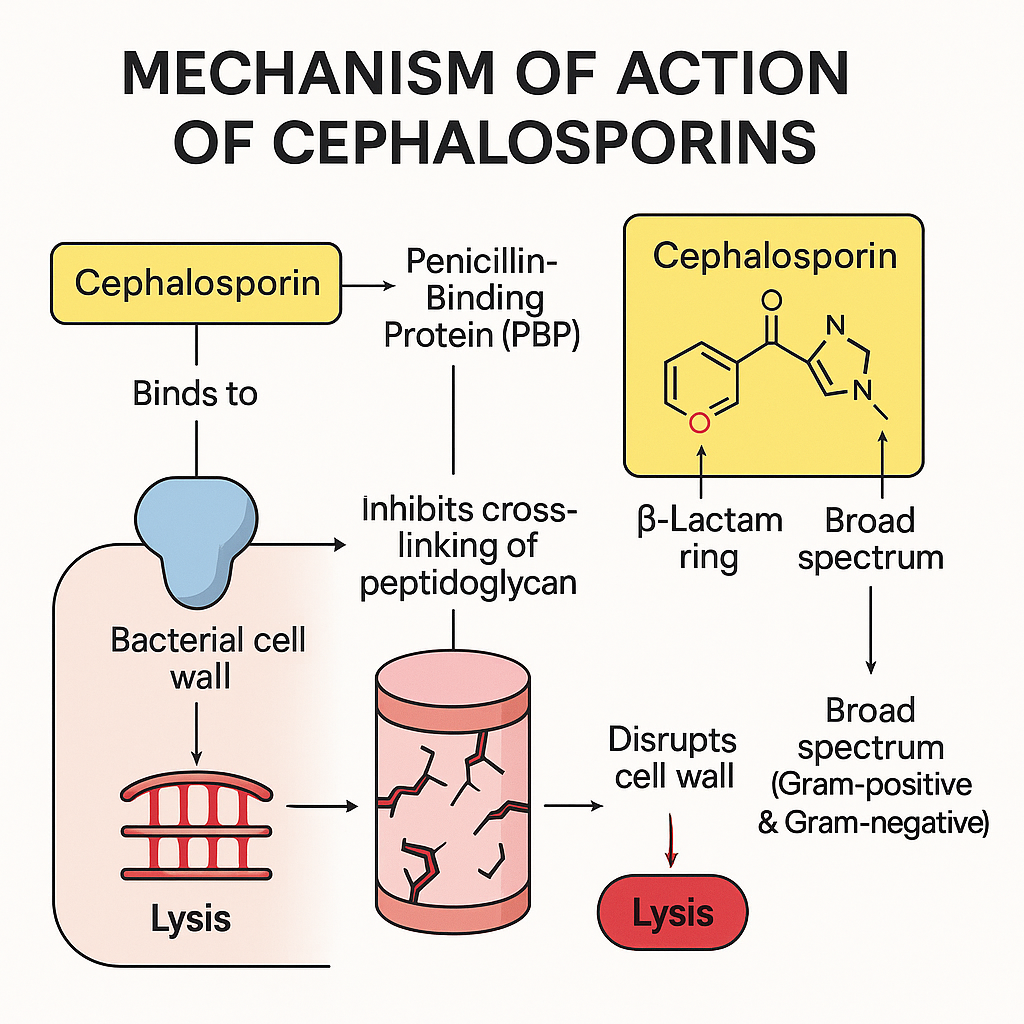
Cephalosporins are a large group of β-lactam antibiotics, structurally and functionally similar to penicillins. They are classified into five generations, each with expanding coverage against Gram-negative organisms and β-lactamase-producing bacteria. Like penicillins, their core mechanism involves inhibition of bacterial cell wall synthesis, making them bactericidal.
They are high-yield in USMLE, NCLEX, GPAT, and NEET-PG, especially for understanding generation-wise coverage, resistance, and clinical use.
Stepwise Mechanism of Action of Cephalosporins
- Target: Penicillin-Binding Proteins (PBPs)
Cephalosporins bind to PBPs, enzymes involved in bacterial cell wall cross-linking. - Inhibition of transpeptidation reaction
They block the cross-linking of peptidoglycan chains, which are essential for bacterial cell wall rigidity. - Disruption of peptidoglycan synthesis
This leads to weakening of the cell wall, especially in growing and dividing bacteria. - Activation of autolytic enzymes
Cephalosporins may promote bacterial autolysins, accelerating cell wall breakdown. - Cell lysis and death
The net result is osmotic instability, cell swelling, and bacterial lysis — hence, they are bactericidal.
Pharmacokinetic Parameters of Cephalosporins
| Parameter | Value (varies by generation) |
|---|---|
| Bioavailability | Moderate to high (many oral forms) |
| Half-life | 1–2 hours (longer for ceftriaxone) |
| Metabolism | Minimal; mostly excreted unchanged |
| Excretion | Renal (ceftriaxone also via bile) |
| Protein binding | Moderate to high |
| Therapeutic range | Dose-specific for type/severity |
Generation-wise Spectrum
| Generation | Spectrum | Key Examples |
|---|---|---|
| 1st | Gram+ (Staph, Strep) | Cefazolin, Cephalexin |
| 2nd | + Anaerobes, some Gram– | Cefuroxime, Cefaclor |
| 3rd | Enhanced Gram–, CNS penetration | Ceftriaxone, Cefotaxime |
| 4th | Broadest, incl. Pseudomonas | Cefepime |
| 5th | MRSA coverage | Ceftaroline |
Clinical Uses of Cephalosporins
- 1st Gen: Skin/soft tissue infections, surgical prophylaxis
- 2nd Gen: Sinusitis, otitis media, respiratory infections
- 3rd Gen: Meningitis, pneumonia, gonorrhea, typhoid
- 4th Gen: Nosocomial infections, febrile neutropenia
- 5th Gen: MRSA, skin infections, CAP
Adverse Effects of Cephalosporins
- Hypersensitivity reactions (cross-reactivity with penicillins)
- GI upset – nausea, diarrhea
- Superinfections – C. difficile colitis
- Nephrotoxicity (when combined with aminoglycosides)
- Disulfiram-like reaction (cefoperazone, cefotetan)
- Bleeding tendency (due to hypoprothrombinemia)
Comparative Analysis: Cephalosporins vs Penicillins
| Feature | Cephalosporins | Penicillins |
|---|---|---|
| Generations | 5 | None |
| β-lactamase stable | Mostly (later gens) | Mostly sensitive |
| Gram– coverage | Better (3rd/4th gens) | Limited (esp. older ones) |
| MRSA activity | 5th gen only (ceftaroline) | Ineffective |
Practice MCQs
Q1. Cephalosporins act by inhibiting:
a. DNA synthesis
b. RNA polymerase
c. Peptidoglycan cross-linking ✅
d. Protein synthesis
Q2. What is the target of cephalosporins?
a. DNA gyrase
b. Penicillin-binding proteins ✅
c. Ribosomes
d. Topoisomerase
Q3. Third-generation cephalosporins are used in:
a. Skin infections
b. Typhoid, meningitis ✅
c. Malaria
d. Viral encephalitis
Q4. Which generation covers MRSA?
a. 1st
b. 3rd
c. 5th ✅
d. 4th
Q5. Ceftriaxone is excreted via:
a. Kidneys only
b. Lungs
c. Bile and kidneys ✅
d. Skin
Q6. Which side effect is linked to cefoperazone?
a. Rash
b. Bleeding ✅
c. Convulsion
d. Tremors
Q7. Cephalosporin cross-reactivity with penicillin is due to:
a. Similar side chains ✅
b. GABAergic activity
c. CYP450 interaction
d. Renal excretion
Q8. Which is best for pseudomonas?
a. Cefazolin
b. Ceftriaxone
c. Cefepime ✅
d. Cephalexin
Q9. Ceftriaxone can be used for:
a. MRSA
b. Gonorrhea ✅
c. UTI in pregnancy
d. MRSE
Q10. Cephalexin belongs to:
a. 3rd generation
b. 5th generation
c. 1st generation ✅
d. 2nd generation
FAQs
Q1: Can cephalosporins be given to penicillin-allergic patients?
In mild allergy, yes. In anaphylaxis, avoid all β-lactams.
Q2: Which cephalosporin is used for meningitis?
Ceftriaxone or cefotaxime due to good CNS penetration.
Q3: Why avoid alcohol with cefoperazone?
It causes disulfiram-like reaction — nausea, flushing, vomiting.
Q4: Which is safe in renal failure?
Ceftriaxone (partly biliary excretion) is preferred.
Q5: Do cephalosporins cover atypicals?
No — they’re ineffective against atypical organisms like Mycoplasma and Chlamydia.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK548553/

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com