Table of Contents
Introduction
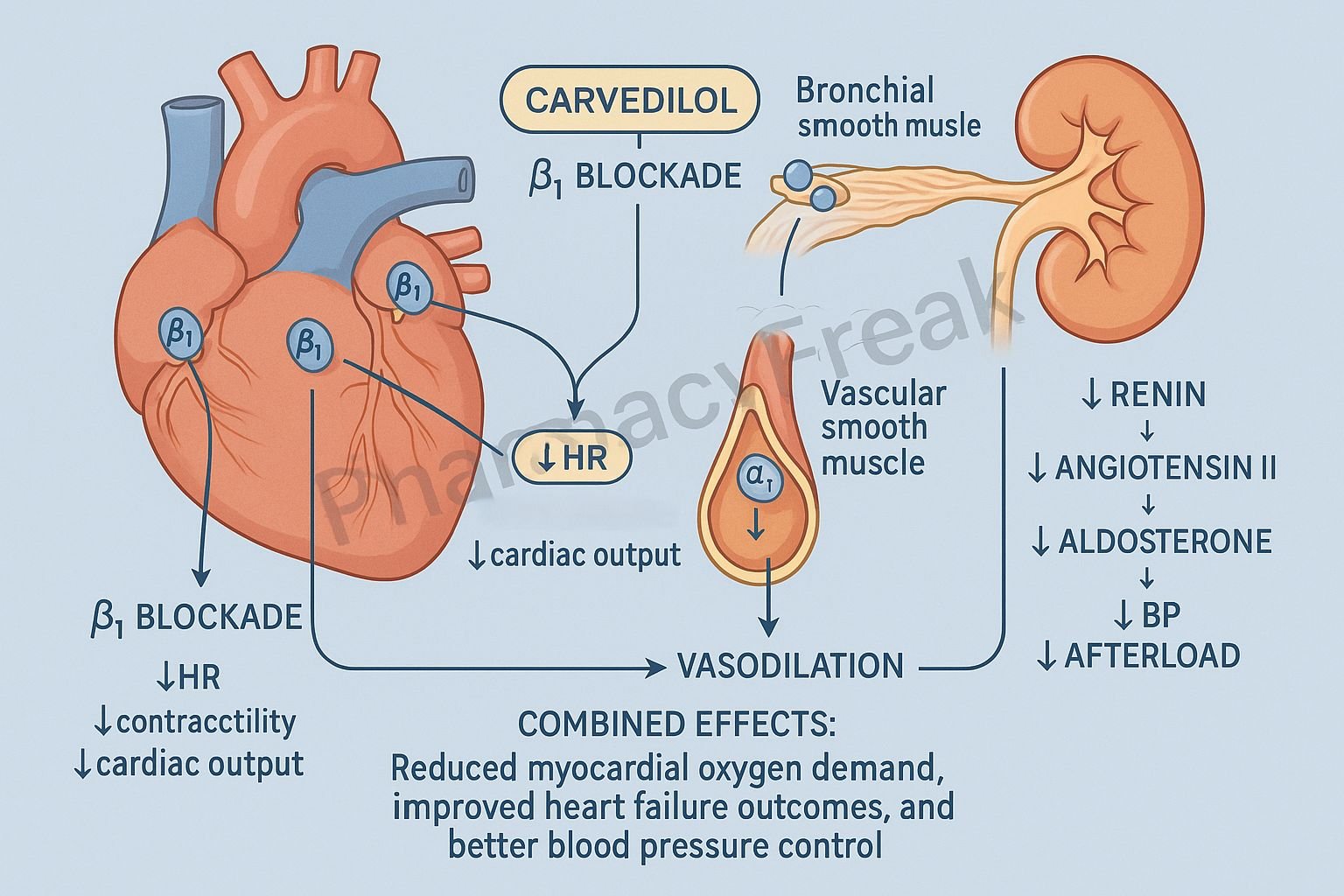
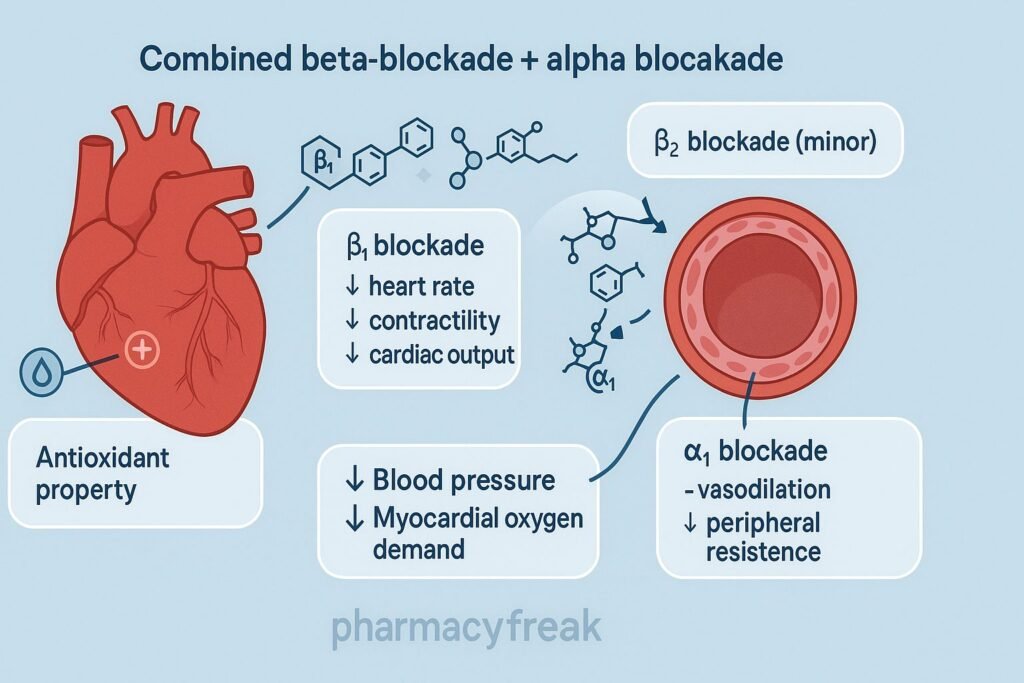
Carvedilol is a nonselective beta-blocker with additional alpha-1 blocking activity. It is widely used in heart failure, hypertension, ischemic heart disease, and for reducing mortality post-myocardial infarction. Unlike traditional beta-blockers, carvedilol provides combined beta-blockade, alpha-blockade, antioxidant properties, and anti-remodeling effects, making it a cornerstone therapy in chronic heart failure.
The Mechanism of Action of Carvedilol involves blocking β1, β2, and α1 receptors, reducing heart rate and contractility, decreasing systemic vascular resistance, and preventing harmful cardiac remodeling.
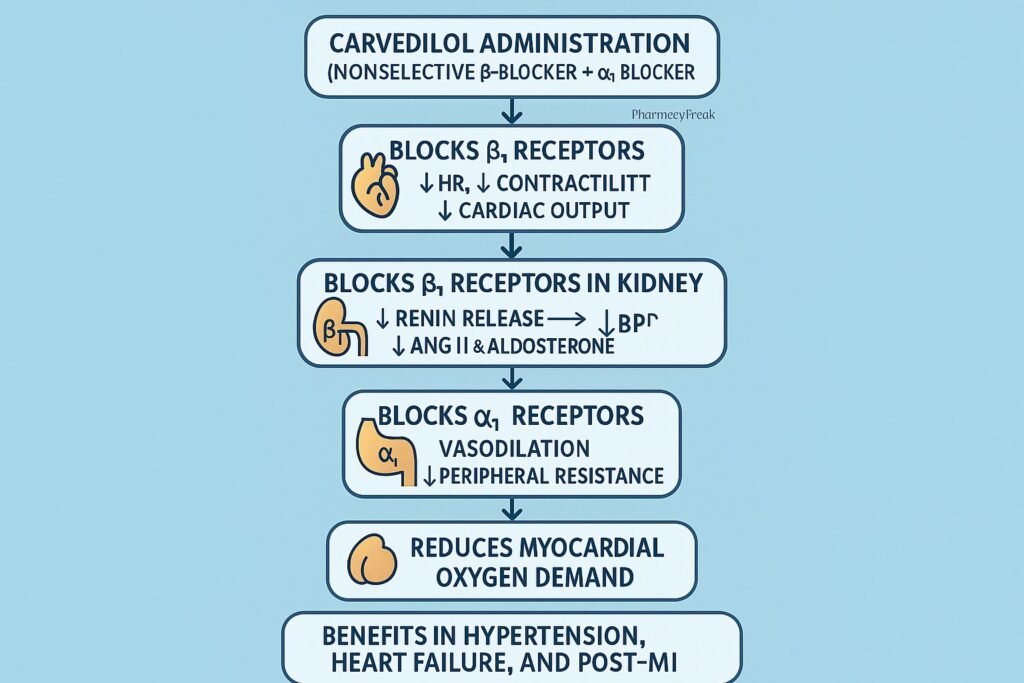
Mechanism of Action (Step-wise)
1. Nonselective Beta Blockade (β1 + β2 Blockade) – Primary Mechanism
Carvedilol inhibits both β1 and β2 adrenergic receptors.
β1 Blockade Effects:
- ↓ Heart rate (negative chronotropy)
- ↓ Cardiac contractility (negative inotropy)
- ↓ Cardiac output
- ↓ Conductivity through AV node (negative dromotropy)
These decrease myocardial oxygen demand.
β2 Blockade Effects:
- Mild bronchoconstriction (important in asthma)
- ↓ Peripheral vasodilation
- ↓ Glycogenolysis (caution in diabetics)
2. Alpha-1 Blockade – Vasodilation
Carvedilol blocks α1 receptors on vascular smooth muscle.
Effects:
- Peripheral vasodilation
- ↓ Systemic vascular resistance
- ↓ Afterload
- Improved cardiac output in heart failure
This vasodilatory effect distinguishes carvedilol from most beta-blockers.
3. Antioxidant Properties
Carvedilol reduces oxidative stress through:
- Scavenging free radicals
- Inhibition of lipid peroxidation
Effect: Protection against myocardial damage and remodeling.
4. Anti-Remodeling Effects
Chronic sympathetic activation promotes cardiac hypertrophy and dilation.
Carvedilol:
- ↓ Catecholamine toxicity
- ↓ Myocyte apoptosis
- ↓ Ventricular hypertrophy
- ↓ Myocardial fibrosis
Outcome: Improved survival in heart failure.
5. Inhibition of RAAS Activation
β1 blockade in the kidneys leads to:
- ↓ Renin release
- ↓ Angiotensin II
- ↓ Aldosterone
This reduces volume overload and vascular resistance.
6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| β1 blockade | ↓ HR, ↓ contractility |
| β2 blockade | Mild bronchoconstriction |
| α1 blockade | Vasodilation, ↓ afterload |
| ↓ Renin release | ↓ RAAS activation |
| Antioxidant effects | ↓ Remodeling and cell death |
| Antiarrhythmic action | Slows AV conduction |
Pharmacokinetics
- Bioavailability: ~25% (first-pass metabolism)
- Protein binding: >95%
- Metabolism: Hepatic (CYP2D6, CYP2C9)
- Half-life: 7–10 hours
- Elimination: Fecal
Clinical Uses
- Chronic heart failure (reduces mortality)
- Hypertension
- Post-myocardial infarction
- Angina pectoris
- Atrial fibrillation (rate control)
- Cardiomyopathy
Adverse Effects
- Bradycardia
- Hypotension
- Fatigue
- Dizziness
- Bronchospasm (caution in asthma/COPD)
- Orthostatic hypotension (due to α1 block)
- Worsening heart failure initially (start low dose)
- Masked hypoglycemia in diabetics
Contraindications
- Asthma or severe COPD
- Severe bradycardia
- Heart block (second or third degree)
- Cardiogenic shock
- Severe hepatic impairment
- Hypotension
Comparative Analysis
| Feature | Carvedilol | Metoprolol | Propranolol |
|---|---|---|---|
| Receptor action | β1, β2, α1 | β1 selective | β1, β2 |
| Vasodilation | Yes | No | No |
| Heart failure mortality benefit | High | Moderate | Limited |
| Bronchospasm risk | Moderate | Low | High |
MCQs
1. Carvedilol lowers blood pressure mainly by:
a) β1 blockade only
b) α1 blockade causing vasodilation
c) β2 stimulation
d) Dopamine receptor blockade
Answer: b) α1 blockade causing vasodilation
2. Carvedilol reduces cardiac remodeling due to:
a) Its diuretic effect
b) Its antioxidant properties
c) Calcium channel blockade
d) Increased heart rate
Answer: b) Its antioxidant properties
3. Carvedilol decreases renin release by blocking:
a) α1 receptors
b) β1 receptors in the kidney
c) β2 receptors
d) Angiotensin receptors
Answer: b) β1 receptors in the kidney
4. A patient with asthma should avoid carvedilol because of:
a) α1 blockade
b) β2 blockade
c) Dopamine antagonism
d) Increased renin activity
Answer: b) β2 blockade
5. Carvedilol is useful in heart failure because it:
a) Increases heart rate
b) Causes vasoconstriction
c) Reduces afterload and inhibits remodeling
d) Increases oxygen consumption
Answer: c) Reduces afterload and inhibits remodeling
FAQs
Q1. Does carvedilol improve survival in heart failure?
Yes—it significantly reduces mortality and hospitalizations.
Q2. Can carvedilol be used in atrial fibrillation?
Yes—it helps with rate control.
Q3. Why start carvedilol at a low dose in heart failure?
To avoid initial worsening of symptoms due to negative inotropy.
Q4. Does carvedilol cause bronchospasm?
Yes—because it blocks β2 receptors.
Q5. Is carvedilol better than metoprolol for heart failure?
Often yes—due to its α1-blocking and antioxidant benefits.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com