Table of Contents
Introduction
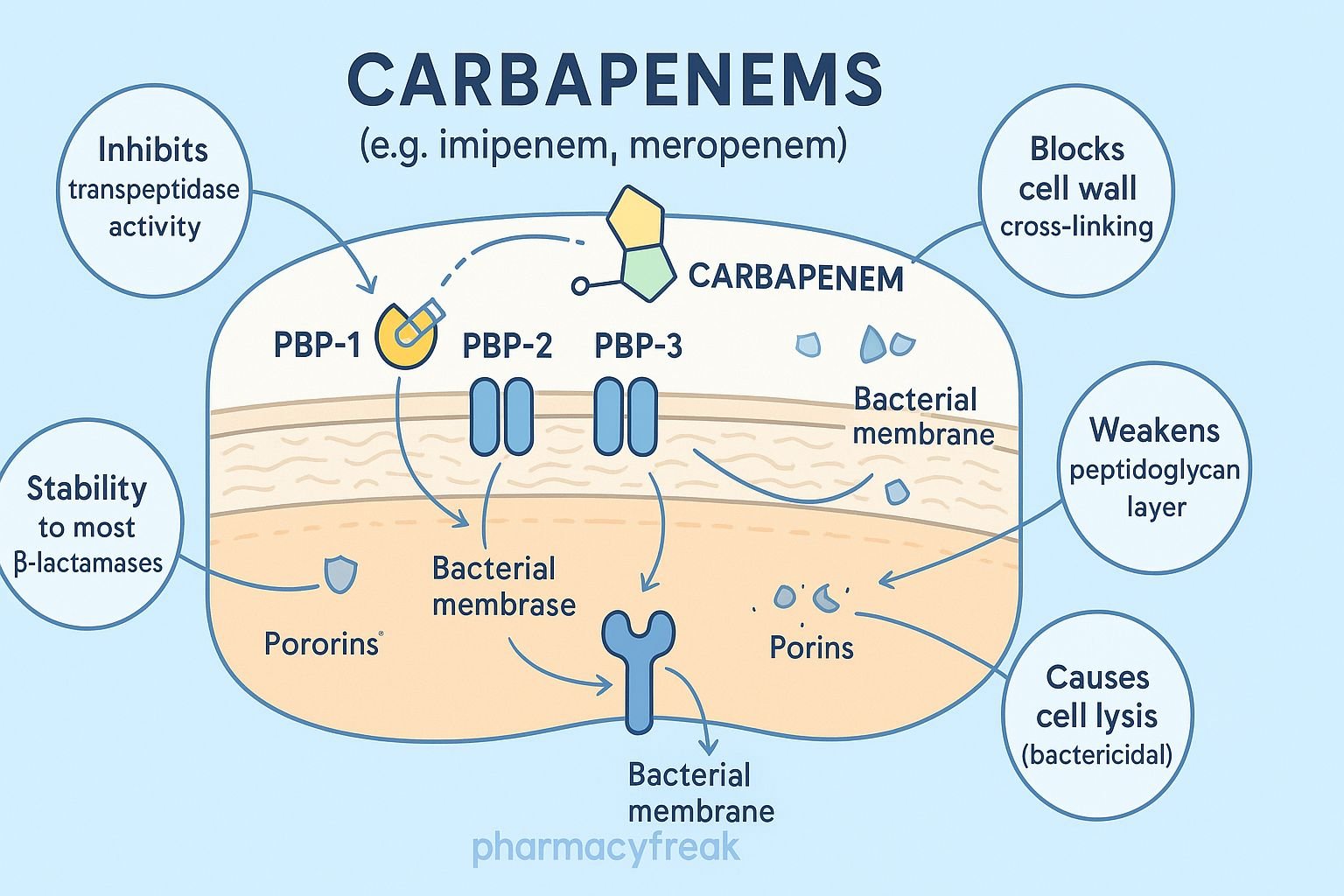
Carbapenems are a powerful class of beta-lactam antibiotics known for their broad-spectrum activity against gram-positive, gram-negative, and anaerobic bacteria. Common agents include imipenem, meropenem, ertapenem, and doripenem. They are often reserved for severe, hospital-acquired, or multidrug-resistant infections due to their potent activity and stability against most beta-lactamases.
The Mechanism of Action of Carbapenems involves inhibition of bacterial cell wall synthesis by binding to penicillin-binding proteins (PBPs), leading to rapid bactericidal activity.


Mechanism of Action (Step-wise)
1. Inhibition of Penicillin-Binding Proteins (PBPs) – Primary Mechanism
Carbapenems bind irreversibly to multiple PBPs, especially:
- PBP-2
- PBP-3
This prevents transpeptidation, the final step in peptidoglycan cross-linking.
Effects:
- Weakening of cell wall structure
- Loss of osmotic stability
- Bacterial cell lysis and death
2. High Affinity for PBPs
Compared to other beta-lactams, carbapenems exhibit:
- Stronger binding
- Broader PBP affinity
- More rapid bactericidal action
This contributes to their exceptional potency.
3. Resistance to Most Beta-Lactamases
Carbapenems are highly resistant to:
- Many serine beta-lactamases
- ESBLs (extended-spectrum beta-lactamases)
However, they are susceptible to:
- Carbapenemases (KPC, NDM, OXA types)
4. Enhanced Permeation Through Gram-Negative Outer Membrane
Carbapenems efficiently penetrate gram-negative bacteria due to:
- Small molecular size
- High stability in periplasm
- Ability to use multiple porin channels
This increases activity against Enterobacterales and Pseudomonas (except ertapenem).
5. Inhibition of Autolysin Inhibitors
Carbapenems activate autolytic enzymes by inhibiting their natural inhibitors.
Effects:
- Enhanced bacterial lysis
- Faster bactericidal action
6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| PBP binding | Inhibits cell wall synthesis |
| Blocks transpeptidation | Weakens peptidoglycan |
| Beta-lactamase resistance | Broad-spectrum activity |
| Porin penetration | Gram-negative coverage |
| Autolysin activation | Rapid cell lysis |
Pharmacokinetics
- Route: IV (all carbapenems)
- Distribution: Wide tissue penetration, including CNS (meropenem > imipenem)
- Metabolism:
- Imipenem is degraded by renal dehydropeptidase → requires cilastatin
- Others (meropenem, ertapenem, doripenem) resist degradation
- Excretion: Renal
- Half-life: 1–4 hours
Clinical Uses
- Severe hospital-acquired infections
- Complicated urinary tract infections
- Intra-abdominal infections
- Sepsis and septic shock
- Multidrug-resistant Gram-negative infections
- Pseudomonas infections (except ertapenem)
- ESBL-producing bacteria infections
Adverse Effects
- Nausea, vomiting
- Diarrhea
- Skin rash
- Seizures (especially imipenem)
- Eosinophilia
- Thrombocytopenia
- Drug fever
Imipenem has the highest seizure risk, particularly in renal impairment.
Contraindications
- Severe beta-lactam allergy
- History of seizures (caution with imipenem)
- Renal impairment (dose adjustments required)
Comparative Analysis
| Feature | Imipenem | Meropenem | Ertapenem | Doripenem |
|---|---|---|---|---|
| Seizure risk | High | Low | Low | Low |
| Pseudomonas activity | Yes | Yes | No | Yes |
| Dosing | 3–4 times/day | 3 times/day | Once daily | 3 times/day |
| Dehydropeptidase degradation | Yes | No | No | No |
MCQs
1. Carbapenems exert their action by inhibiting:
a) DNA gyrase
b) PBPs involved in cell wall synthesis
c) Protein synthesis at 50S subunit
d) RNA polymerase
Answer: b) PBPs involved in cell wall synthesis
2. Imipenem must be given with cilastatin because:
a) It prevents allergic reactions
b) It inhibits renal dehydropeptidase
c) Enhances bactericidal effect
d) Prevents seizures
Answer: b) It inhibits renal dehydropeptidase
3. Which carbapenem does NOT cover Pseudomonas?
a) Meropenem
b) Imipenem
c) Ertapenem
d) Doripenem
Answer: c) Ertapenem
4. Carbapenems are resistant to most:
a) Carbapenemases
b) ESBLs
c) Metallo-beta-lactamases
d) Polymyxins
Answer: b) ESBLs
5. A major adverse effect of imipenem is:
a) Nephrotoxicity
b) Seizures
c) Ototoxicity
d) Hepatotoxicity
Answer: b) Seizures
FAQs
Q1. Why are carbapenems considered broad-spectrum antibiotics?
Because they inhibit multiple PBPs and resist most beta-lactamases.
Q2. Which carbapenem is safest for CNS infections?
Meropenem—lowest seizure risk and good CSF penetration.
Q3. Are carbapenems oral drugs?
No—all are IV only.
Q4. Why is ertapenem once daily?
It has a longer half-life.
Q5. Do carbapenems treat ESBL infections?
Yes—they are first-line for ESBL-producing organisms.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com