Penicillin are among the earliest discovered and most widely used antibiotics. They belong to the beta-lactam class and are highly effective against various gram-positive and some gram-negative bacteria. Penicillin work by inhibiting bacterial cell wall synthesis and are often used in both clinical and community settings.
This blog from Pharmacy Freak provides a detailed classification, clinical applications, drug of choice highlights, side effects, and practical insights for pharmacy and medical students.
Table of Contents
What is Penicillin
Penicillins are beta-lactam antibiotics derived from Penicillium fungi. They act by inhibiting bacterial cell wall synthesis by binding to penicillin-binding proteins (PBPs), leading to bacterial cell lysis.
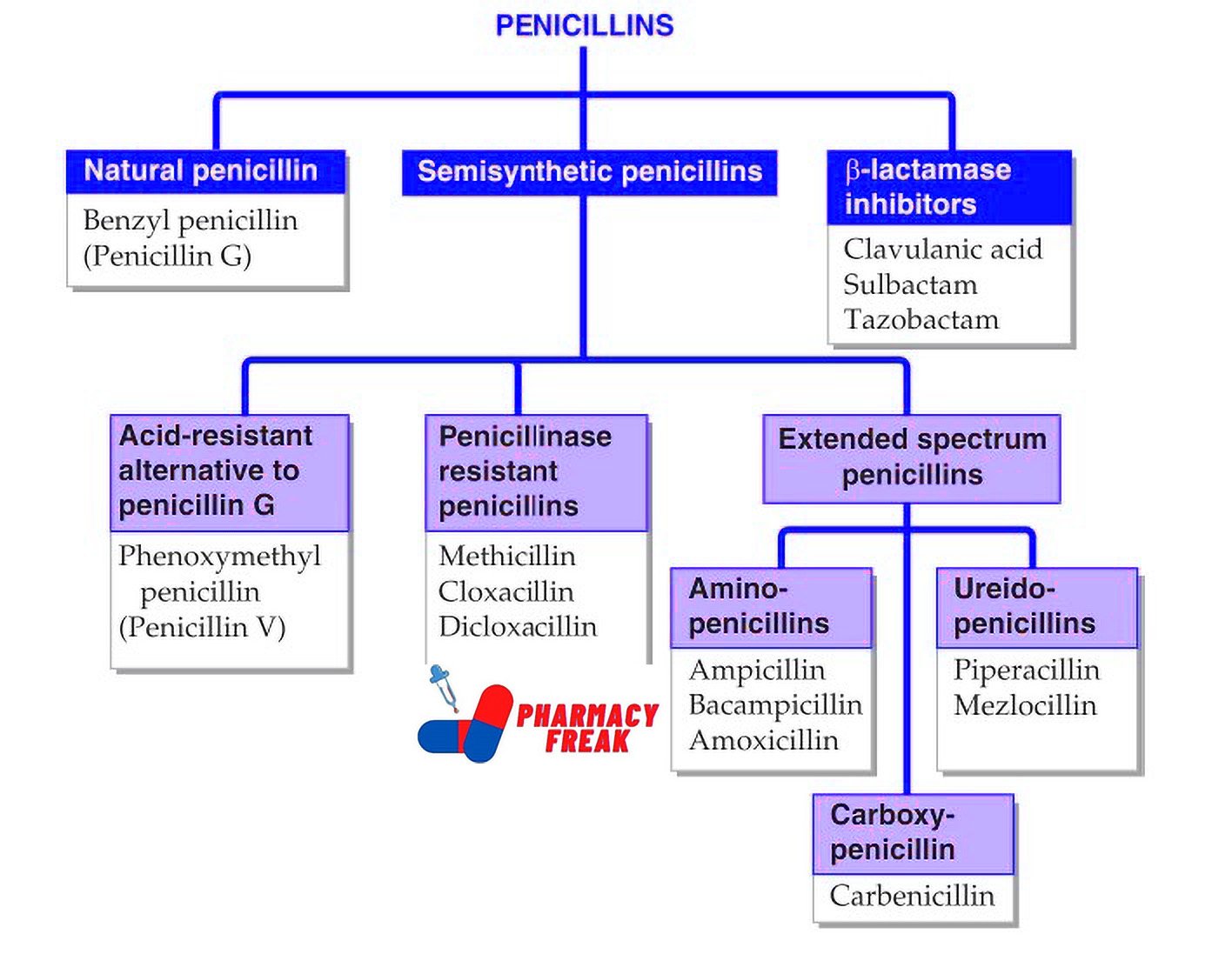
Classification of Penicillins (KD Tripathi)
- Natural penicillin: Benzyl penicillin (Penicillin G)
- Semisynthetic penicillins
- Acid-resistant alternative to penicillin G: Phenoxymethyl penicillin (Penicillin V)
- Penicillinase resistant penicillins: Methicillin, Cloxacillin, Dicloxacillin
- Extended spectrum penicillins –
- Aminopenicillins: Ampicillin, Bacampicillin, Amoxicillin
- Ureidopenicillins: Piperacillin, Mezlocillin
- Carboxypenicillin: Carbenicillin
- β-lactamase inhibitors: Clavulanic acid, Sulbactam, Tazobactam
Classification of Penicillins (General)
Penicillins are classified based on their spectrum of activity and resistance to beta-lactamases.
- Natural Penicillins
Active primarily against gram-positive cocci and some gram-negative cocci
Examples:
- Penicillin G (benzylpenicillin) – IV/IM
- Penicillin V (phenoxymethylpenicillin) – Oral
Use: Streptococcal infections, syphilis, meningococcal infections
- Penicillinase-Resistant Penicillins (Anti-staphylococcal)
Resistant to staphylococcal beta-lactamase
Examples:
- Methicillin (no longer used due to nephrotoxicity)
- Nafcillin, Oxacillin, Cloxacillin, Dicloxacillin
Use: Staphylococcus aureus infections (MSSA)
- Aminopenicillins (Extended-spectrum)
Active against gram-positive bacteria and some gram-negative organisms
Examples:
- Ampicillin (IV, oral)
- Amoxicillin (oral)
Use: Respiratory tract infections, urinary tract infections, enteric infections
- Antipseudomonal Penicillins
Broader gram-negative activity including Pseudomonas aeruginosa
Examples:
- Piperacillin
- Ticarcillin
Use: Hospital-acquired infections, pseudomonal infections
- Beta-lactamase Inhibitor Combinations
Combination of penicillins with beta-lactamase inhibitors to extend spectrum
Examples:
- Ticarcillin + Clavulanic acid
Use: Mixed infections, resistant bacterial strains, polymicrobial infections - Amoxicillin + Clavulanic acid
- Ampicillin + Sulbactam
- Piperacillin + Tazobactam
Uses
Penicillins are used in the treatment of:
- Streptococcal infections (pharyngitis, cellulitis)
- Pneumococcal pneumonia
- Syphilis (Penicillin G)
- Gonorrhea (in penicillin-sensitive strains)
- Dental infections
- Otitis media, sinusitis
- Urinary tract infections
- Endocarditis prophylaxis
- Meningitis (Penicillin G or Ampicillin)
- Staphylococcal infections (Nafcillin, Oxacillin)
- Pseudomonal infections (Piperacillin + Tazobactam)
Drug of Choice Highlights
- Streptococcal pharyngitis – Penicillin V
- Syphilis – Benzathine Penicillin G
- Enterococcal infections – Ampicillin
- Listeria monocytogenes meningitis – Ampicillin
- Staphylococcus aureus (MSSA) – Cloxacillin or Nafcillin
- Pseudomonas – Piperacillin + Tazobactam
- Dog or cat bite infections – Amoxicillin + Clavulanic acid
- H. pylori (part of triple therapy) – Amoxicillin
- Dental abscess – Amoxicillin
Side Effects
- Hypersensitivity reactions (rash, urticaria, anaphylaxis) – most common
- Gastrointestinal upset (diarrhea, nausea)
- Pseudomembranous colitis – especially with ampicillin
- Nephrotoxicity – with methicillin (no longer used)
- Electrolyte disturbances – with large doses of IV penicillins
- Superinfections – such as candidiasis
Updated Clinical Pearls
- Penicillins are time-dependent antibiotics; dosing should aim to maintain plasma levels above the minimum inhibitory concentration (MIC).
- Combination with beta-lactamase inhibitors extends their spectrum to include many beta-lactamase-producing organisms.
- Amoxicillin has better oral bioavailability and causes less diarrhea than ampicillin.
- Methicillin-resistant Staphylococcus aureus (MRSA) is resistant to all beta-lactam antibiotics; alternative agents like vancomycin are used.
- Penicillin allergy should be confirmed before avoidance; many reported allergies are not true IgE-mediated hypersensitivity.
- Penicillin G is still the gold standard treatment for syphilis and neurosyphilis.
Trivia
- Accidental Discovery: Penicillin was discovered accidentally by Sir Alexander Fleming in 1928 when mold (Penicillium notatum) contaminated a petri dish in his lab, leading to one of medicine’s most important breakthroughs.
- First Successful Antibiotic: Penicillin became the first widely used antibiotic, revolutionizing medical treatment and dramatically reducing deaths from bacterial infections during World War II.
- Common Allergy: Penicillins are among the most common causes of drug allergies, affecting up to 10% of people. However, most individuals who believe they’re allergic actually lose their sensitivity over time or were misdiagnosed.
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 720–730
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 318–321
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 1455–1468
Related Links

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com