Antiplatelet drugs are essential in the prevention and management of thromboembolic diseases. They inhibit platelet aggregation and reduce the formation of arterial thrombi, which are responsible for conditions such as myocardial infarction, stroke, and peripheral vascular disease. These drugs form a crucial component of antithrombotic therapy.
This blog from Pharmacy Freak outlines the classification, clinical applications, drug of choice, side effects, and current clinical pearls of antiplatelet drugs for students and healthcare professionals.
Table of Contents
What is Antiplatelet Drugs
Antiplatelet drugs are agents that interfere with platelet function and prevent platelet aggregation, thereby reducing the formation of thrombi in arteries. They are most effective in preventing arterial thrombosis.
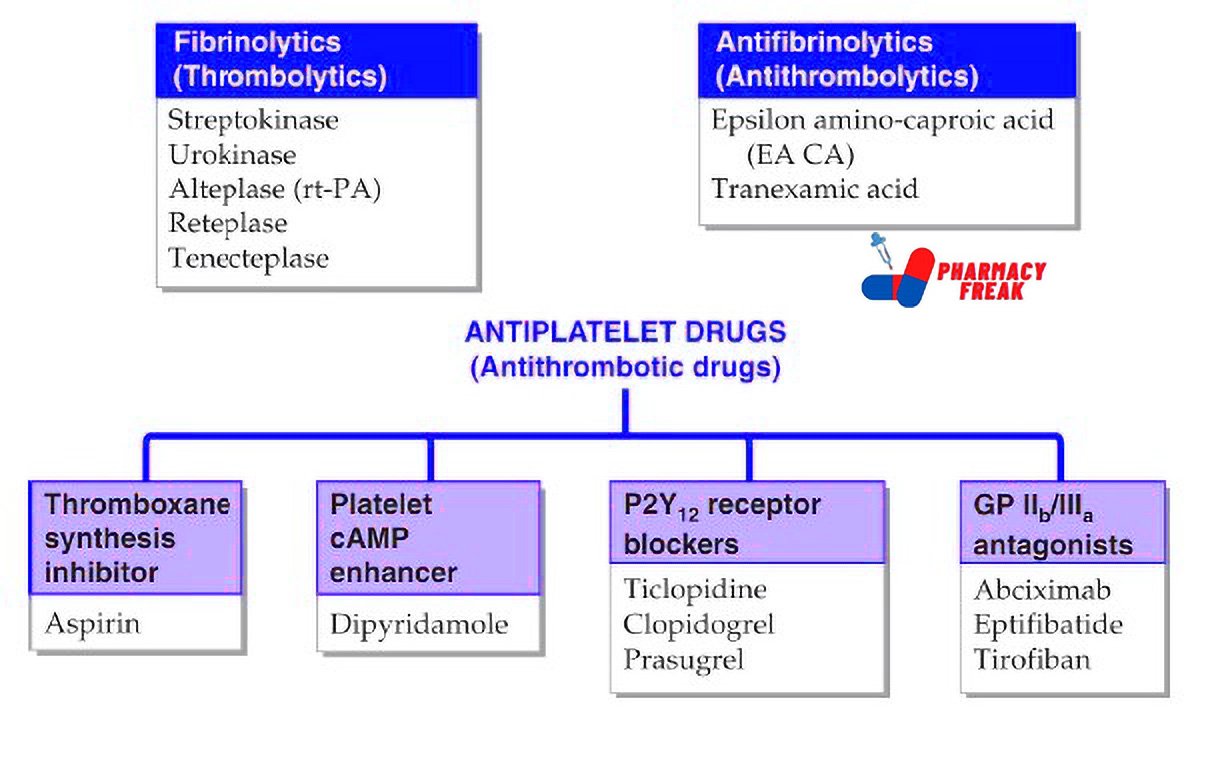
Classification of Antiplatelet Drugs (KD Tripathi)
- Fibrinolytics (Thrombolytics):
Streptokinase, Urokinase, Alteplase (rt-PA), Reteplase, Tenecteplase - Antifibrinolytics (Antithrombolytics):
Epsilon amino-caproic acid (EA CA), Tranexamic acid - ANTIPLATELET DRUGS (Antithrombotic Drugs):
- Thromboxane synthesis inhibitor: Aspirin
- Platelet cAMP enhancer: Dipyridamole
- P2Y₁₂ receptor blockers: Ticlopidine, Clopidogrel, Prasugrel
- GP IIb/IIIa antagonists: Abciximab, Eptifibatide, Tirofiban
Classification of Antiplatelet Drugs (General)
Antiplatelet drugs are classified based on their mechanism of action:
- Cyclooxygenase (COX) Inhibitors
Mechanism: Inhibit cyclooxygenase-1 (COX-1) in platelets, reducing thromboxane A2 synthesis
Examples:
- Aspirin
Use: Primary and secondary prevention of myocardial infarction and stroke
Note: Irreversible inhibition; effect lasts for the life of the platelet (7–10 days)
- ADP Receptor (P2Y12) Inhibitors
Mechanism: Block P2Y12 receptors on platelets, preventing ADP-mediated aggregation
Examples:
- Clopidogrel
- Prasugrel
- Ticagrelor
- Ticlopidine
Use: Acute coronary syndrome, post-PCI stent placement
Note: Clopidogrel is a prodrug; Ticagrelor is reversible and more potent
- Glycoprotein IIb/IIIa Inhibitors
Mechanism: Inhibit final common pathway of platelet aggregation
Examples:
- Abciximab
- Eptifibatide
- Tirofiban
Use: Intravenous agents used during angioplasty or acute coronary syndrome
Note: Most potent class but used only in hospital setting
- Phosphodiesterase (PDE) Inhibitors
Mechanism: Increase cAMP in platelets, inhibiting platelet aggregation
Examples:
- Dipyridamole
- Cilostazol
Use: - Dipyridamole: Combined with aspirin in stroke prevention
- Cilostazol: Used in intermittent claudication (peripheral arterial disease)
- Protease-Activated Receptor-1 (PAR-1) Antagonists
Mechanism: Block thrombin-induced platelet aggregation
Example:
- Vorapaxar
Use: Secondary prevention in patients with prior MI or PAD
Note: Used as add-on therapy; high bleeding risk
Uses
Antiplatelet drugs are used in:
- Acute coronary syndrome (NSTEMI, STEMI)
- Secondary prevention after myocardial infarction
- Post-percutaneous coronary intervention (PCI) with stent placement
- Ischemic stroke and transient ischemic attack (TIA)
- Peripheral arterial disease
- Prevention of thromboembolism in atrial fibrillation (when anticoagulants are contraindicated)
- Graft or shunt thrombosis prevention
- Prevention of clotting in hemodialysis machines or during procedures
Drug of Choice Highlights
- Primary prevention of cardiovascular events – Low-dose Aspirin
- Acute coronary syndrome – Dual antiplatelet therapy (Aspirin + Clopidogrel or Ticagrelor)
- Post-stenting (PCI) – Aspirin + P2Y12 inhibitor (e.g., Clopidogrel for at least 1 year)
- Secondary stroke prevention – Aspirin or Aspirin + Dipyridamole
- Peripheral artery disease with claudication – Cilostazol
- Aspirin intolerance – Clopidogrel
- High-risk percutaneous interventions – Abciximab (IV)
Side Effects
- Aspirin – Gastric irritation, peptic ulcers, bleeding, hypersensitivity
- Clopidogrel – Diarrhea, rash, thrombotic thrombocytopenic purpura (rare)
- Ticagrelor – Dyspnea, bleeding, bradycardia
- Prasugrel – Higher bleeding risk, contraindicated in stroke or elderly patients
- Glycoprotein IIb/IIIa inhibitors – Bleeding, thrombocytopenia
- Dipyridamole – Headache, dizziness, hypotension
- Cilostazol – Palpitations, headache, contraindicated in heart failure
- Vorapaxar – Serious bleeding, not for use in patients with stroke or TIA history
Updated Clinical Pearls
- Aspirin is still the most widely used and cost-effective antiplatelet agent for both primary and secondary prevention.
- Dual antiplatelet therapy (DAPT) with aspirin and a P2Y12 inhibitor is standard for 12 months post-stent placement.
- Ticagrelor and Prasugrel are more potent than Clopidogrel but carry a higher bleeding risk.
- Cilostazol improves walking distance in patients with intermittent claudication and has antiplatelet properties.
- Vorapaxar is a novel agent reserved for high-risk patients and is not routinely used due to bleeding concerns.
- Genetic testing may be considered in poor responders to Clopidogrel due to CYP2C19 polymorphisms.
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 540–547
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 224–226
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 933–940
Related Links

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com