Angina pectoris is a clinical syndrome characterized by chest pain or discomfort due to transient myocardial ischemia. It occurs when there is an imbalance between myocardial oxygen supply and demand. Antianginal drugs are used to relieve symptoms, improve exercise tolerance, and prevent future ischemic episodes.
This blog from Pharmacy Freak presents the classification, uses, drug of choice, adverse effects, and clinical updates on antianginal drugs as per standard pharmacological sources
Table of Contents
What is Antianginal Drug
Antianginal drugs are medications used to prevent or relieve angina pectoris by improving the balance between oxygen supply and oxygen demand in the myocardium
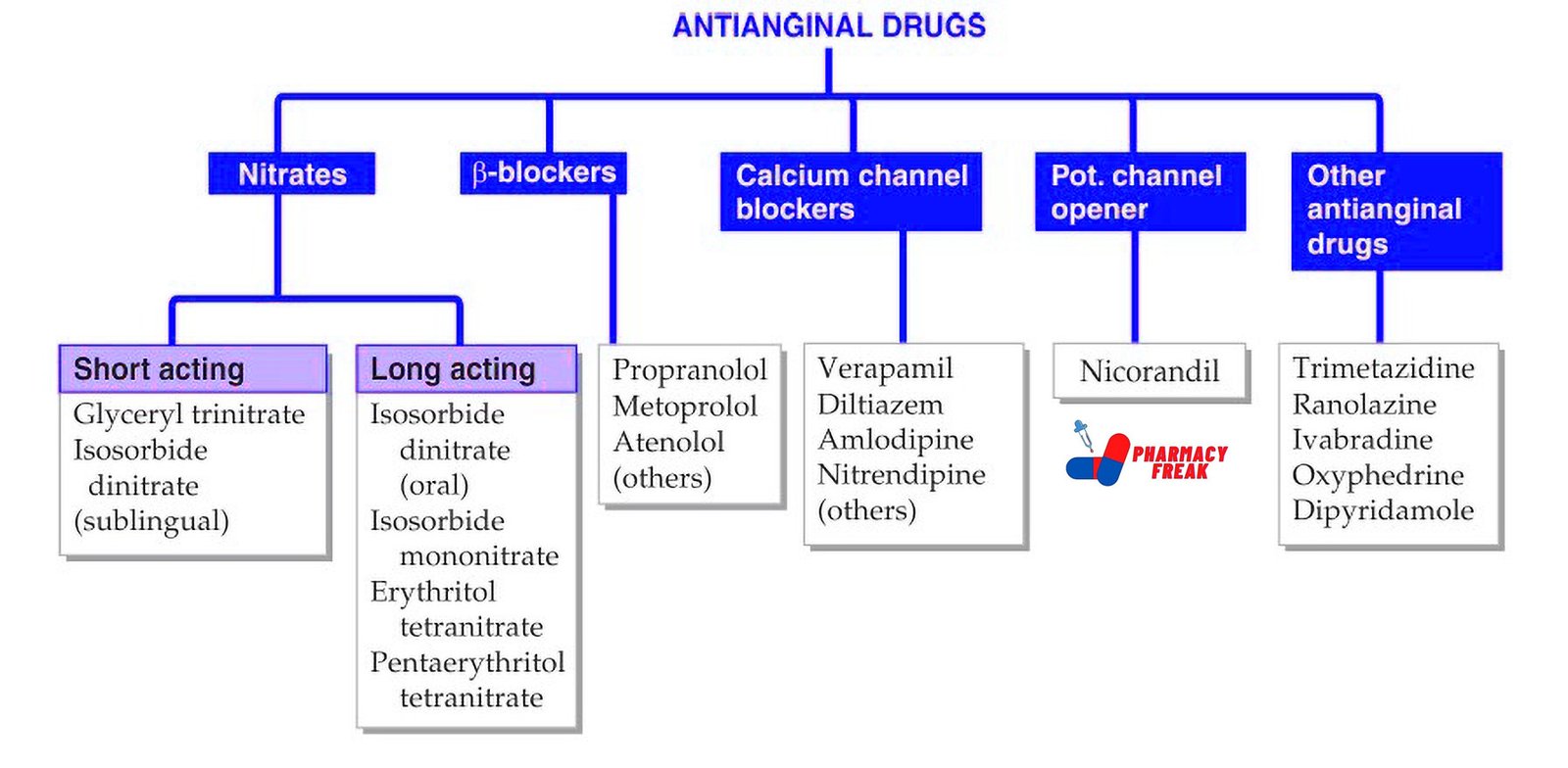
Classification of Antianginal Drug (KD Tripathi)
- Nitrates –
- Short acting: Glyceryl trinitrate, Isosorbide dinitrate (sublingual)
- Long acting: Isosorbide dinitrate (oral), Isosorbide mononitrate, Erythritol tetranitrate, Pentaerythritol tetranitrate
- β–blockers: Propranolol, Metoprolol, Atenolol, others
- Calcium channel blockers: Verapamil, Diltiazem, Amlodipine, Nitrendipine, others
- Potassium channel opener: Nicorandil
- Other antianginal drugs: Trimetazidine, Ranolazine, Ivabradine, Oxyfedrine, Dipyridamole
Classification of Antianginal Drug (General)
Antianginal drugs are classified into the following categories based on their mechanism of action:
- Nitrates
Mechanism: Release nitric oxide → activate guanylate cyclase → increase cGMP → vasodilation
Effect: Dilate veins (↓ preload), arteries (↓ afterload), and coronary vessels (↑ supply)
Examples: Nitroglycerin, Isosorbide dinitrate, Isosorbide mononitrate
Use: Acute and chronic stable angina, variant angina - Beta-Adrenergic Blockers
Mechanism: Block β1 receptors → ↓ heart rate, ↓ contractility, ↓ blood pressure
Effect: Reduce myocardial oxygen demand
Examples: Metoprolol, Atenolol, Propranolol
Use: Chronic stable angina, post-MI angina
Note: Not useful in variant angina; may worsen vasospasm - Calcium Channel Blockers (CCBs)
Mechanism: Inhibit L-type calcium channels → reduce vascular tone and cardiac workload
Subtypes:
a. Dihydropyridines – Amlodipine, Nifedipine (mainly vasodilation)
b. Non-dihydropyridines – Verapamil, Diltiazem (vasodilation + cardiac depression)
Use: Stable and variant angina
Note: Diltiazem and Verapamil also control heart rate - Potassium Channel Openers
Mechanism: Activate ATP-sensitive K⁺ channels → arterial vasodilation
Example: Nicorandil
Use: Chronic stable angina
Note: Dual action (nitrate-like + K⁺ channel opening) - Metabolic Modulators
a. Ranolazine
Mechanism: Inhibits late inward Na⁺ current → ↓ intracellular Ca²⁺ → ↓ myocardial workload
Use: Chronic stable angina unresponsive to other drugs
b. Trimetazidine
Mechanism: Inhibits fatty acid oxidation → shifts metabolism to glucose oxidation (more efficient)
Use: Adjunct in chronic angina
Note: Improves myocardial energy efficiency
- Sinus Node Inhibitors
Mechanism: Selective inhibition of If current → ↓ heart rate without ↓ contractility
Drug: Ivabradine
Use: Stable angina with high heart rate when β-blockers are not tolerated
Note: No effect on BP or myocardial contractility
Uses
Antianginal drugs are used in:
- Stable angina (effort-induced)
- Unstable angina (as part of acute coronary syndrome)
- Variant (Prinzmetal’s) angina
- Silent myocardial ischemia
- Post-myocardial infarction prophylaxis
- Prevention of exercise-induced ischemia
- Pre-operative cardiac optimization
Drug of Choice Highlights
- Stable angina – Nitroglycerin (acute), Beta blockers or CCBs (chronic)
- Variant angina – Calcium channel blockers (especially Dihydropyridines)
- Chronic angina unresponsive to other drugs – Ranolazine
- Acute anginal attack – Sublingual Nitroglycerin
- Angina with high heart rate – Ivabradine
- Angina with hypertension – Beta blockers or Non-DHP CCBs
- Post-MI angina – Beta blockers (especially cardioselective)
- Angina in heart failure – Nitrates, Beta blockers, Ivabradine (if HR >70 bpm)
Side Effects
- Nitrates – Headache, flushing, hypotension, tolerance (nitrate-free interval needed)
- Beta blockers – Bradycardia, fatigue, bronchospasm, sexual dysfunction
- CCBs – Ankle edema, hypotension (DHPs), bradycardia, AV block (Non-DHPs)
- Ranolazine – Dizziness, constipation, QT prolongation
- Ivabradine – Visual disturbances (phosphenes), bradycardia
- Nicorandil – Headache, mouth ulcers
- Trimetazidine – GI upset, extrapyramidal symptoms (rare)
Updated Clinical Pearls
- Nitrates provide immediate relief in acute angina but tolerance develops on chronic use; a daily nitrate-free interval is essential.
- Beta blockers reduce mortality after myocardial infarction and are a mainstay in chronic stable angina.
- Non-dihydropyridine CCBs should be avoided with beta blockers due to risk of bradycardia and AV block.
- Ranolazine is particularly useful in patients who cannot tolerate hemodynamic effects of traditional drugs.
- Ivabradine selectively lowers heart rate without affecting blood pressure, making it suitable in normotensive patients with tachycardia.
- Trimetazidine is used as an add-on therapy when conventional drugs are not fully effective.
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 578–584
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 240–243
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 673–682
Related Links

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com