Any appreciable harmful or unpleasant reaction resulting from an intervention related to the use of a medicinal product, which predicts hazard from future administration and warrants prevention or specific treatment, or alteration of the dosage regimen or withdrawal of the product is known as an Adverse Drug Reaction (ADR). Both toxic effects and side effects differ from each other.
Toxic effects result from higher doses, are harmful, and occur via the same mechanism as the therapeutic effects. Side effects are not associated with dose, may or may not be harmful, and occur via separate mechanisms. The terms adverse drug reaction and adverse drug effect can be used interchangeably as the only difference between them is that an adverse reaction is related to the change in the patient. In contrast, an adverse effect is related to the drug effect.
However, the term adverse event should be considered separate from the other terms, because it is an adverse outcome that occurs when a patient is receiving a drug but for which causality has not been determined, and it may or may not be related to the drug being administered.
Table of Contents
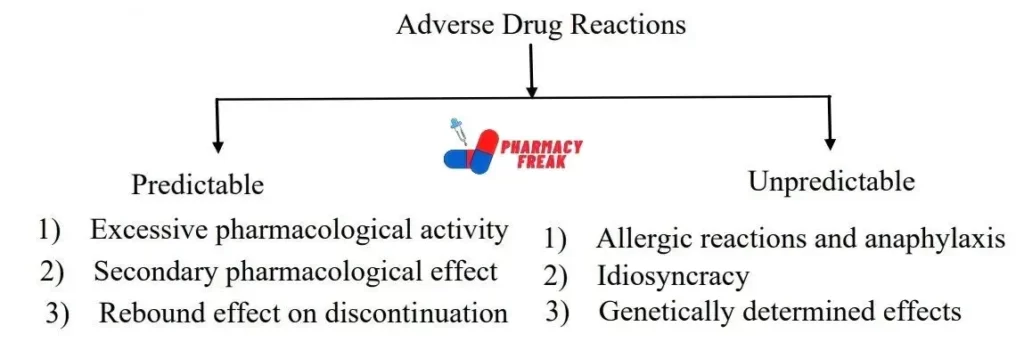
CLASSIFICATION Of ADVERSE DRUG REACTIONS
Excessive Pharmacological Effects
The excessive pharmacological effects a drug may produce lead to the most common adverse drug reactions. CNS depressants, hypoglycaemics, cardioactive agents, and hypotensive agents can give rise to such reactions. These reactions develop in all patients when any drug is given in excessive dosage. However, these reactions may also occur at normal doses in neonates, and geriatrics, in patients suffering from more than 70% kidney dysfunction, and in patients with lower albumin levels due to liver or kidney damage. Some examples of excessive pharmacological effects are:
- Bradycardia in patients administering digoxin in excessive dosage.
- Respiratory depression if patients having severe bronchitis are administered with morphine or benzodiazepine hypnotics.
Secondary Pharmacological Effects
Dose-related reactions include secondary pharmacological effects, iatrogenic effects, hyper-susceptibility, and overdose. Along with therapeutic effects, a drug also produces adverse or beneficial secondary effects. For example, morphine is an analgesic that can cause two adverse secondary effects, i.e., constipation and respiratory depression. Diphenhydramine is an antihistamine that produces sedation as a secondary effect and thus is used for inducing sleep.
There are many drugs that at average doses give rise to multiple pharmacological effects. Still, these drugs are prescribed for any one of these many actions. For example, antihistamines are prescribed either for allergic skin reactions or for their anti-nausea effects. In hospitalized patients, antihistamines cause drowsiness; but in travelers, they may produce secondary adverse pharmacological effects involving CNS depression that may be dangerous if the individuals are consuming hypnotics, tranquilizers, or OTC drugs. Hence, excessive as well as secondary pharmacological effects give rise to a wide range of undesired drug effects in different patients.
Toxicity Following Sudden Withdrawal of Drugs
When an individual suddenly stops taking a drug that he/she has been taking for a long – term, a withdrawal or abstinence syndrome occurs. Acute withdrawal gives rise to variable symptoms, like sweating, tremors, anxiety, seizures, hallucinations, and delirium. Irritability and discomfort develop when the drug is stopped, and this stimulates many users to resume the intake of that drug. Such use of drugs acts as a self-medication to treat the unpleasant symptoms developed by not using those drugs. As a result, a vicious and escalating cycle is generated. For CNS depressants (e.g., alcohol, barbiturates, and benzodiazepines), a rebound effect of hyper-excitability may occur when their effects wear off after a drinking episode ends. This withdrawal reaction occurs markedly with higher use levels. Withdrawal symptoms start occurring from 12-24 hours after stopping the drug and last for several days; however, this depends on the drug. The medical treatment for alcohol withdrawal involves sedating the hyper-excitability of the nervous system by using another drug of the same class of depressants, benzodiazepines, and vitamins. Barbiturates have also been used but they are associated with the risk of cross-tolerance (tolerance to one drug generalizes to other drugs in the same category), thus are less preferred. If alcoholic patients are given barbiturates to reduce withdrawal symptoms, they may quickly adapt due to cross-tolerance and fail to benefit. Thus, newer drugs such as clonidine and β-adrenergic blockers are used. With the reduction in withdrawal symptoms, the medical treatment is progressively decreased. Naltrexone is an alcohol antagonist, which has been used for treating alcohol withdrawal symptoms. Naloxone is a heroin antagonist that competes with it to bind on the opiate receptors, therefore, has been used for treating heroin withdrawal symptoms.
Allergic Drug Reactions
Drug allergy (or hypersensitivity) is a type B adverse drug reaction. A drug allergy is often difficult to diagnose as there are no consistent laboratory tests for identifying the related drug (for which the allergic reaction has occurred). In some cases, the symptoms imitate that of the infectious disease. Diagnosis of an allergic reaction becomes easier if the administered drug is known to produce such a reaction ( e.g., penicillin); however the situation is difficult if the drug is hardly ever reported to produce any allergy. Some drugs can produce pseudoallergic reactions which resemble allergic reactions but have no immunological basis. These reactions occur due to mast cell degranulation and consequent histamine release. These reactions also resemble type I hypersensitivity reactions. Histamine release on administration of opiates (e.g., morphine), vancomycin, and radiocontrast media is an example of a pseudoallergic reaction.
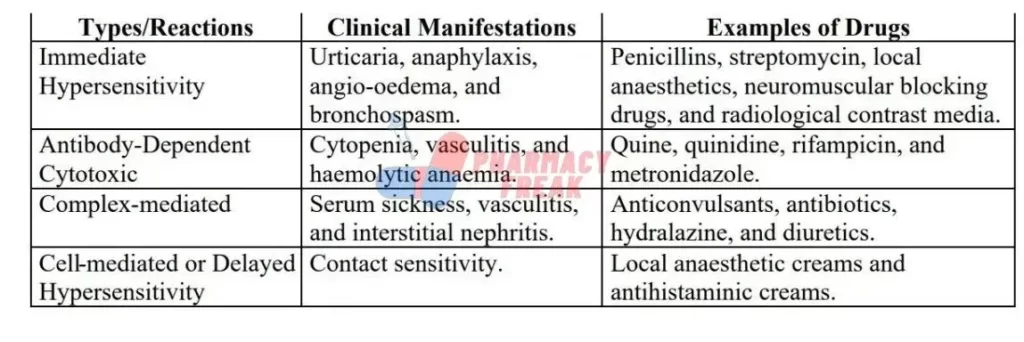
Allergic reactions to drugs follow the type I -IV classification.
Idiosyncrasy
Idiosyncratic adverse reactions are less common than pharmacological adverse reactions, but sometimes they may become serious and lead to many deaths. The drug-metabolizing system of the body is involved in the pathogenesis of several idiosyncratic reactions. Metabolism of the drug (divided into phases I and II) serves as a defense mechanism as it triggers the excretion of the parent drug and its metabolites, thereby preventing their accumulation in the body that might cause dose-dependent toxicity. Drug metabolism also inhibits the accumulation of some drugs within particular cells or cellular compartments to prevent toxicity. For example, perhexiline ne (an anti-anginal agent) caused hepatotoxicity and peripheral neuropathy in indi viduals lacking the CYP2D6 (debrisoquine hydroxylase) isoform of cytochrome P-450. Enzymes involved in drug metabolism, mainly the phase I cytochrome P-450 enzymes, may form chemically reactive and toxic metabolites by the bioactivation process. In many individuals, the formation of such metabolites is counter-balanced by bioinactivation (a detoxification mechanism). However, the balance between bioactivation and bioinactivation in vulnerable individuals is disturbed by either genetic or host factors such as age, enzyme induction, and disease. These factors prevent the detoxification of toxic metabolites, thus allowing them to bind covalently to various cellular macromolecules and cause toxicity. With most of the drugs, the factors causing this imbalance are unknown, which is why such reactions continue to occur. In some cases, chemically reactive metabolites are formed regardless of the dose. At therapeutic doses, the formed toxic metabolite is detoxified by cellular defense mechanisms. On the other hand, in case of overdoses, an imbalance occurs between bioactivation and bioinactivation. This leads to the formation of excessive chemically reactive metabolites that overcome the cellular detoxification capacity and cause cell damage.
The term idiosyncrasy is used for uncommon and unexpected drug effects. It also includes drug-induced fetal abnormalities, for example, phocomelia in the progeny of mothers taking thalidomide. This drug is a potential teratogen, but its mechanism is unidentified. If mothers take this drug in the initial period of gestation when the limb buds are forming, the newborn will have sealed limbs. One more idiosyncratic reaction is drug-induced cancer. A long induction period exists between the exposure to the drugs and the development of tumors, thus very little is known about the drug factors involved in cancer etiology.
Genetically Determined Toxicity
Patients with special genotypes or genetic makeup have an increased risk of drug toxicity. Some examples of such reactions are:
- Patients with a hereditary deficiency of pseudocholinesterase cannot metabolize succinylcholine (muscle relaxant), thus its use results in prolonged paralysis and apnoea.
- Glucose-6-phosphate dehydrogenase enzyme causes glucose degradation. Individuals deficient in this enzyme can develop hemolytic anemia after taking primaquine, quinidine, aminoquinolines, sulphonamides, and nitrofurantoin.
- Isoniazid, hydralazine, and procainamide are metabolized in the liver by N -acetyl transferase enzyme. Some individuals are slow and some are fast acetylators. The slow acetylators of isoniazid suffer from peripheral neuropathy; while the slow acetylators of hydralazine and procainamide suffer from drug -induced lupus syndrome.

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com
