Table of Contents
Introduction
Cyclizine is a first-generation antihistamine belonging to the piperazine class, primarily used as an antiemetic and antivertigo agent. It is commonly prescribed for the prevention and treatment of motion sickness, postoperative nausea and vomiting, and vestibular disorders. Cyclizine is frequently tested in pharmacology, ENT, anesthesia, and nursing examinations because of its central anticholinergic and antihistaminic actions.
Mechanism of Action (Step-wise)
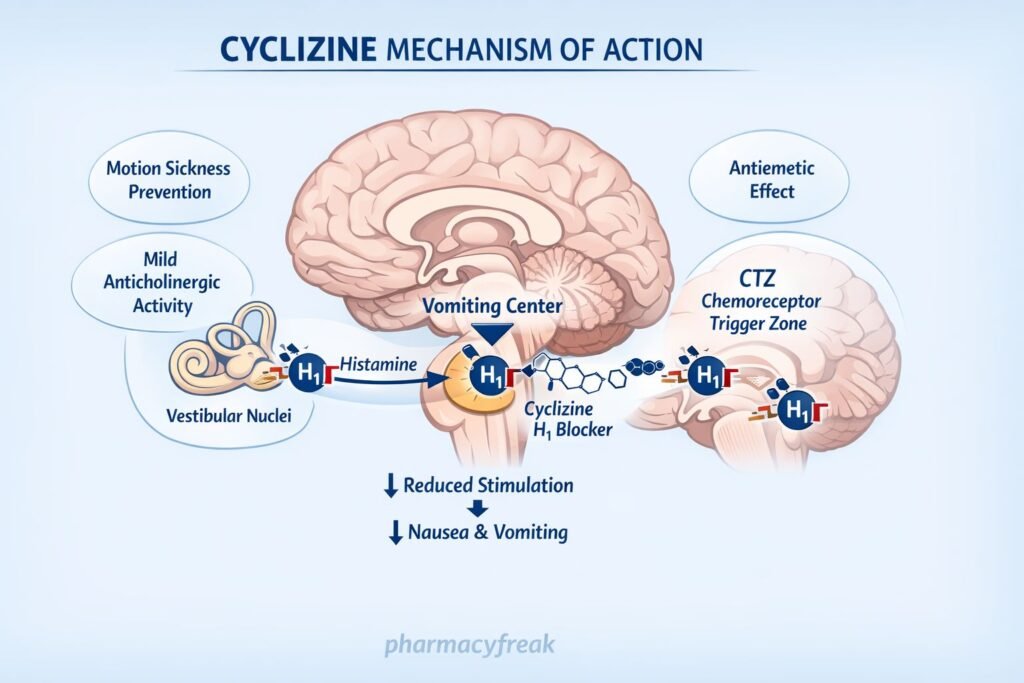
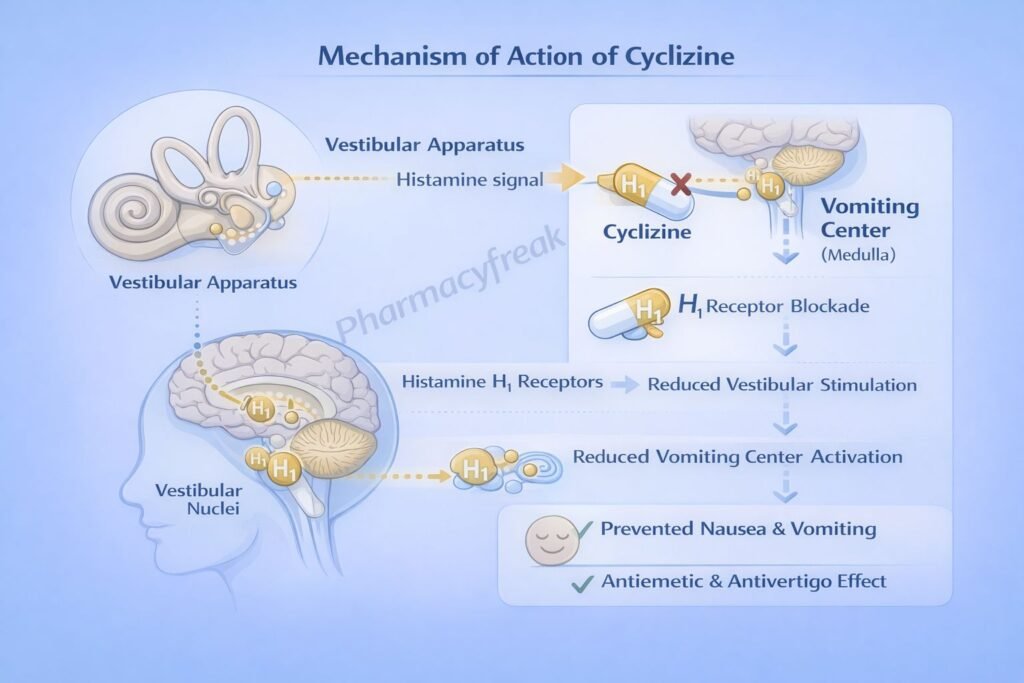
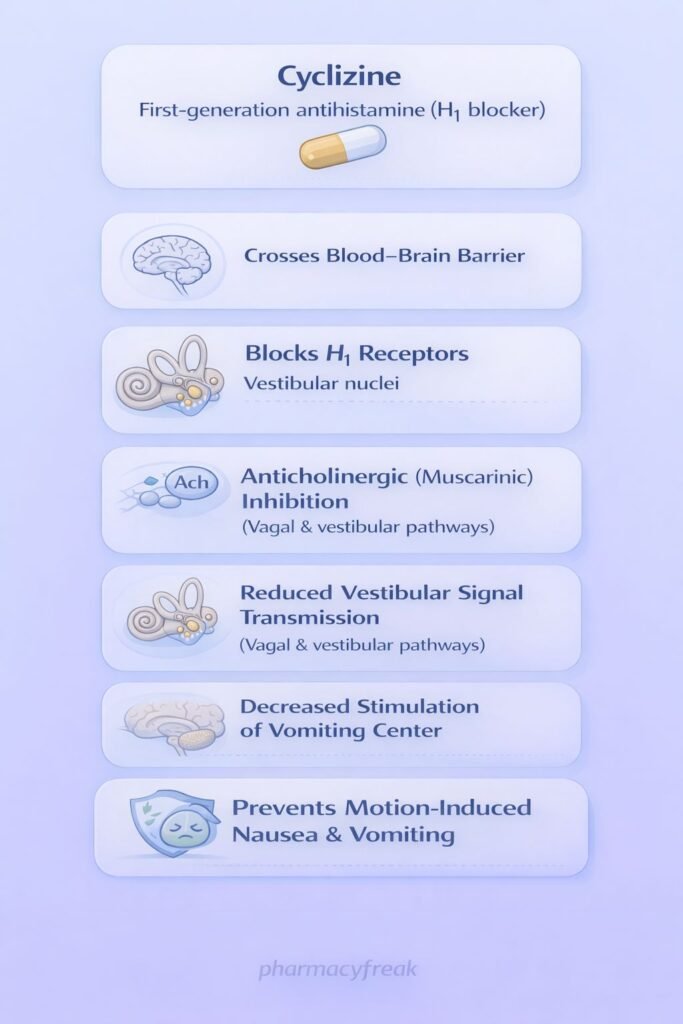
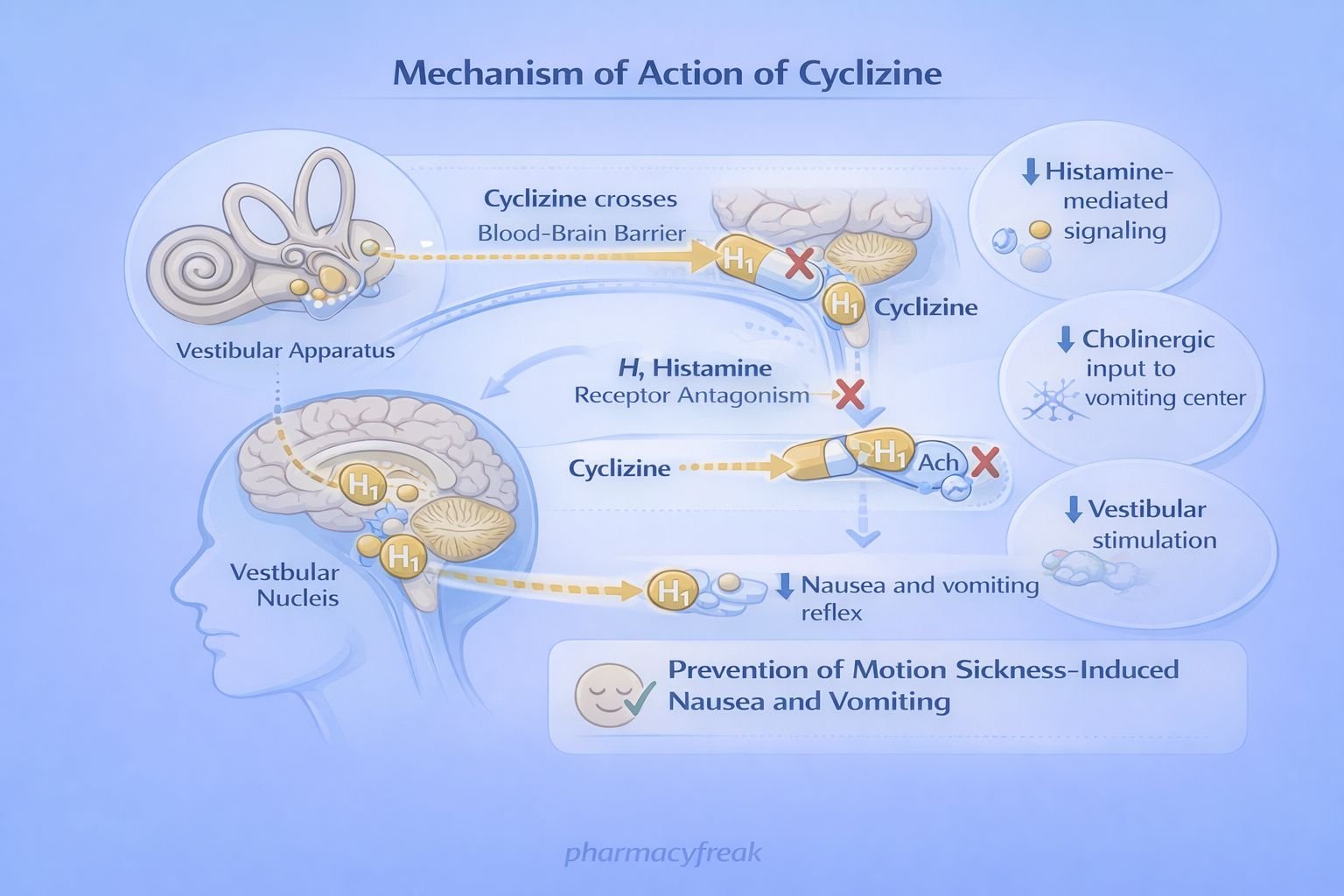
Cyclizine produces its antiemetic and antivertigo effects through central histamine and muscarinic receptor blockade.
Step-wise mechanism:
- Histamine-Mediated Vestibular Stimulation
Motion and vestibular disturbances activate histaminergic pathways projecting from the vestibular nuclei to the vomiting center in the medulla. - H₁ Receptor Blockade
Cyclizine competitively antagonizes histamine H₁ receptors in the vestibular apparatus and vomiting center. - Suppression of Vestibular Input
Blocking H₁ receptors reduces excitatory signals from the vestibular system to the chemoreceptor trigger zone (CTZ). - Anticholinergic (Antimuscarinic) Action
Cyclizine also exhibits central antimuscarinic effects, further inhibiting vestibular stimulation of the vomiting center. - Reduced Neuronal Firing in Vomiting Center
Combined H₁ and muscarinic blockade suppresses neuronal activity in the medullary vomiting center. - Antiemetic and Antivertigo Effect
The net effect is prevention of nausea, vomiting, and vertigo, particularly motion-induced symptoms.
Pharmacokinetics
- Absorption: Well absorbed orally
- Onset of action: 30–60 minutes
- Distribution: Widely distributed; crosses the blood–brain barrier
- Metabolism: Hepatic metabolism
- Elimination: Renal excretion of metabolites
- Half-life: Approximately 14–20 hours
- Duration of action: Long-lasting, suitable for motion sickness prophylaxis
Clinical Uses
Cyclizine is primarily used for disorders related to vestibular dysfunction and nausea:
- Motion sickness prophylaxis and treatment
- Vertigo (including Ménière’s disease)
- Postoperative nausea and vomiting
- Drug-induced nausea
- Pregnancy-associated nausea (selected cases, with caution)
It is less effective for chemotherapy-induced nausea compared to 5-HT₃ antagonists.
Adverse Effects
Adverse effects are typical of first-generation antihistamines and anticholinergics:
- Central nervous system:
- Drowsiness
- Sedation
- Dizziness
- Anticholinergic effects:
- Dry mouth
- Blurred vision
- Urinary retention
- Constipation
- Others:
- Headache
- Paradoxical excitation (rare, especially in children)
Caution is required in elderly patients and those with glaucoma or prostatic hypertrophy.
Comparative Analysis (must include a table + explanation)
Comparison of Antiemetic Antihistamines
| Feature | Cyclizine | Dimethindene | Meclizine |
|---|---|---|---|
| Drug class | H₁ antihistamine | H₁ antihistamine | H₁ antihistamine |
| Anticholinergic action | Moderate | Mild | Mild |
| Sedation | Moderate | Moderate | Low |
| Duration of action | Long | Moderate | Long |
| Primary use | Motion sickness, vertigo | Allergy, motion sickness | Motion sickness |
Explanation:
Cyclizine is particularly effective for vestibular-related nausea due to its balanced antihistaminic and anticholinergic activity. Compared to meclizine, cyclizine may cause slightly more sedation but provides strong antiemetic efficacy.
MCQs (10–15)
- Cyclizine primarily blocks which receptor?
a) H₂ receptor
b) H₁ receptor
c) 5-HT₃ receptor
d) Dopamine D₂ receptor
Answer: b) H₁ receptor
- Cyclizine is most effective in preventing:
a) Chemotherapy-induced vomiting
b) Pregnancy hyperemesis
c) Motion sickness
d) Opioid-induced nausea
Answer: c) Motion sickness
- Cyclizine exerts antiemetic action by acting mainly on the:
a) Cerebral cortex
b) Hypothalamus
c) Vestibular system
d) Spinal cord
Answer: c) Vestibular system
- Cyclizine belongs to which drug class?
a) Phenothiazine
b) Benzamide
c) Piperazine antihistamine
d) Butyrophenone
Answer: c) Piperazine antihistamine
- Which additional pharmacologic action contributes to cyclizine’s efficacy?
a) Dopamine antagonism
b) Serotonin antagonism
c) Anticholinergic effect
d) GABA agonism
Answer: c) Anticholinergic effect
- A common adverse effect of cyclizine is:
a) Diarrhea
b) Sedation
c) Hypertension
d) Bradycardia
Answer: b) Sedation
- Cyclizine crosses the blood–brain barrier because it is:
a) Water soluble
b) Lipophilic
c) Ionized
d) Protein bound
Answer: b) Lipophilic
- Cyclizine should be used cautiously in patients with:
a) Asthma
b) Glaucoma
c) Peptic ulcer
d) Diabetes
Answer: b) Glaucoma
- Cyclizine prevents vomiting by suppressing signals to the:
a) Cerebellum
b) CTZ and vomiting center
c) Limbic system
d) Reticular formation
Answer: b) CTZ and vomiting center
- Compared to first-generation antihistamines, cyclizine causes:
a) No sedation
b) Severe EPS
c) Moderate sedation
d) QT prolongation
Answer: c) Moderate sedation
FAQs (minimum 5)
- What is the primary mechanism of cyclizine?
Blockade of histamine H₁ receptors in the vestibular system and vomiting center. - Why is cyclizine effective in motion sickness?
It suppresses vestibular input to the vomiting center. - Does cyclizine have anticholinergic effects?
Yes, contributing to its antiemetic action. - Is cyclizine useful for chemotherapy-induced nausea?
No, it is less effective than 5-HT₃ antagonists. - Can cyclizine cause drowsiness?
Yes, due to central H₁ receptor blockade. - Is cyclizine safe in elderly patients?
Use cautiously due to anticholinergic and sedative effects.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
https://accessmedicine.mhmedical.com - Katzung BG. Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com - Tripathi KD. Essentials of Medical Pharmacology
https://www.jaypeebrothers.com - Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com