Table of Contents
Introduction
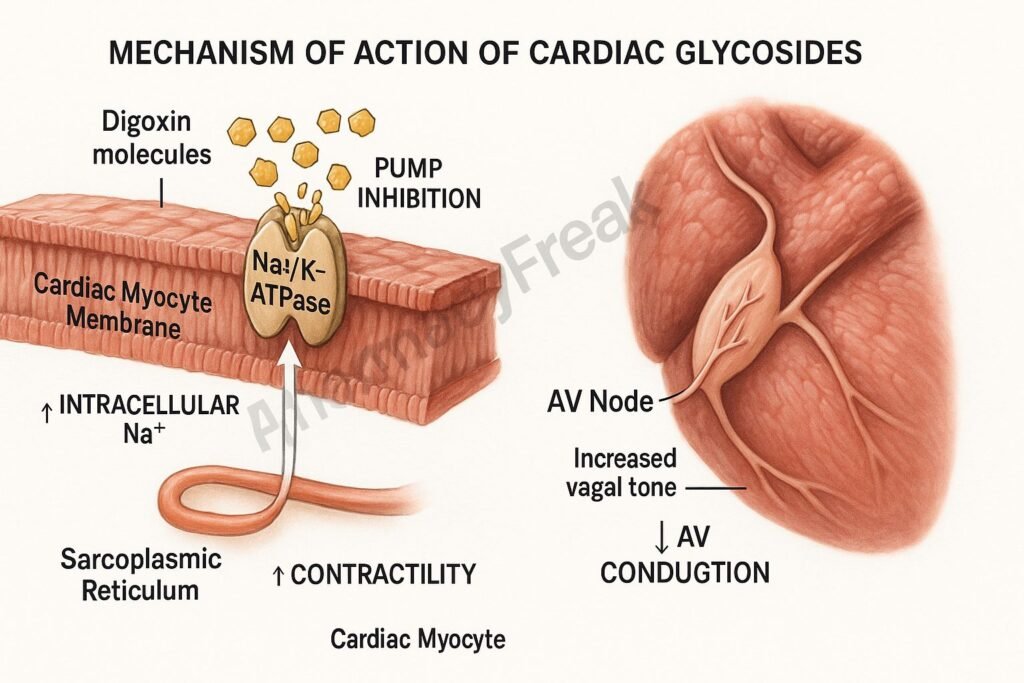
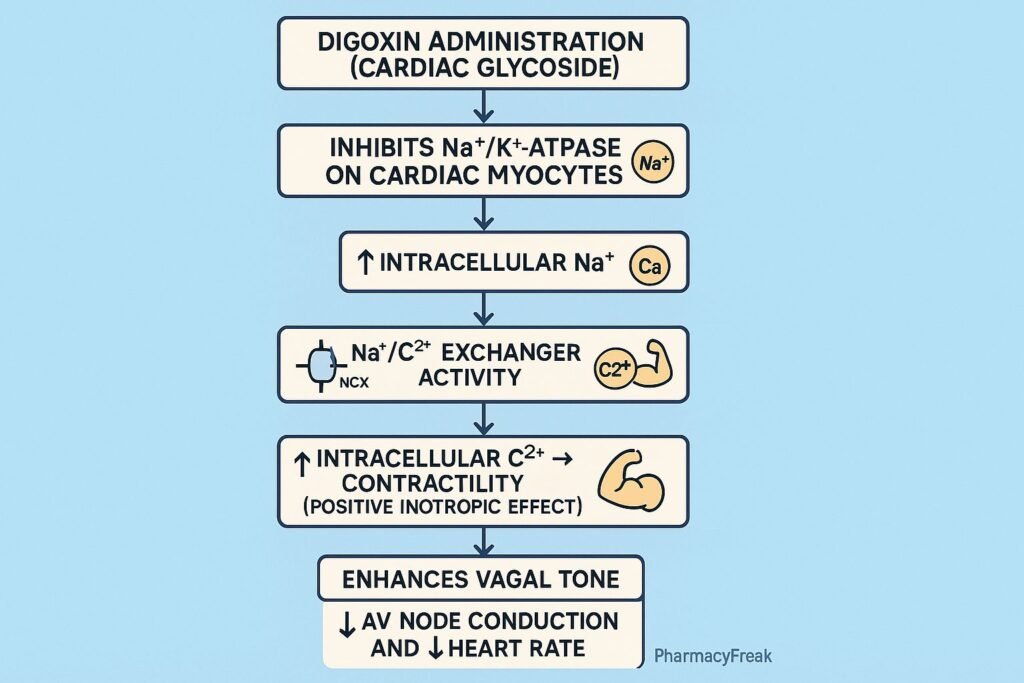
Cardiac glycosides, primarily digoxin, are potent drugs used in the management of heart failure and supraventricular arrhythmias. These compounds increase cardiac contractility (positive inotropy) and modulate conduction through the atrioventricular (AV) node.
The Mechanism of Action of Cardiac Glycosides centers on inhibition of the Na⁺/K⁺-ATPase pump, leading to increased intracellular calcium and enhanced myocardial contraction, along with parasympathetic stimulation that slows AV nodal conduction.
Mechanism of Action (Step-wise)
1. Inhibition of Na⁺/K⁺-ATPase – Primary Mechanism
Cardiac glycosides bind to and inhibit the sodium–potassium pump on cardiac myocytes.
Normal pump function:
- Pumps 3 Na⁺ out
- Pumps 2 K⁺ in
When inhibited:
- ↑ Intracellular Na⁺
- ↓ Na⁺ gradient across cell membrane
This initiates downstream effects.
2. Reduced Activity of Na⁺/Ca²⁺ Exchanger (NCX)
The NCX normally uses the Na⁺ gradient to extrude Ca²⁺.
When intracellular Na⁺ rises:
- NCX activity decreases
- Less Ca²⁺ is pumped out
- Intracellular Ca²⁺ increases
3. Increased Calcium in Sarcoplasmic Reticulum
Excess intracellular Ca²⁺ is stored in the sarcoplasmic reticulum.
Effect:
- Larger calcium release during each action potential
- Stronger myocardial contraction (positive inotropic effect)
This is beneficial in heart failure by improving cardiac output.
4. Increased Vagal Tone (Parasympathetic Activity)
Cardiac glycosides stimulate the vagus nerve.
Effects:
- ↓ SA node firing
- ↓ AV node conduction
- ↑ AV nodal refractoriness
This is useful in:
- Atrial fibrillation
- Atrial flutter
- Paroxysmal supraventricular tachycardia (PSVT)
5. Negative Chronotropic and Dromotropic Effects
Due to vagal stimulation:
- Negative chronotropy: Slows heart rate
- Negative dromotropy: Slows AV nodal conduction
This prevents rapid ventricular response in AF/AFl.
6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| Na⁺/K⁺-ATPase inhibition | ↑ Intracellular Ca²⁺ |
| ↓ Na⁺/Ca²⁺ exchanger | ↑ Contractility |
| ↑ SR Ca²⁺ stores | Stronger systole |
| ↑ Vagal tone | Slower AV conduction |
| ↓ Heart rate | Antiarrhythmic effect |
Pharmacokinetics
- Absorption: Good oral absorption
- Distribution: Large volume; binds to tissues
- Half-life: ~36–48 hours (longer in renal disease)
- Metabolism: Minimal hepatic
- Excretion: Renal (dose adjustment needed)
Clinical Uses
- Congestive heart failure (improves symptoms, not mortality)
- Atrial fibrillation (rate control)
- Atrial flutter
- PSVT (rare use)
Adverse Effects
Cardiac
- Arrhythmias (PVCs, AV block, ventricular tachycardia)
- Bradycardia
GI
- Nausea, vomiting
- Anorexia
CNS
- Confusion
- Visual disturbances (yellow/green vision – xanthopsia)
Electrolyte effects
- Hypokalemia increases toxicity
- Hyperkalemia seen in severe overdose
Contraindications
- Ventricular fibrillation
- Heart block
- Hypokalemia
- Severe renal impairment (caution)
- Concomitant use with drugs that increase digoxin levels (verapamil, amiodarone, macrolides)
Comparative Analysis
| Feature | Digoxin | Digitoxin | Ouabain |
|---|---|---|---|
| Solubility | Hydrophilic | Lipophilic | Poor oral absorption |
| Half-life | 36–48 h | 7 days | Very short |
| Elimination | Renal | Hepatic | Renal |
| Clinical use | Common | Rare | Experimental |
MCQs
1. Cardiac glycosides increase intracellular Ca²⁺ by inhibiting:
a) Ca²⁺ channels
b) Na⁺/K⁺-ATPase
c) Na⁺ channels
d) K⁺ channels
Answer: b) Na⁺/K⁺-ATPase
2. Digoxin’s positive inotropy is due to:
a) Increased catecholamines
b) Increased sarcoplasmic calcium stores
c) Increased Na⁺/K⁺-ATPase activity
d) Decreased vagal tone
Answer: b) Increased sarcoplasmic calcium stores
3. The arrhythmogenic risk of digoxin increases with:
a) Hyperkalemia
b) Hypokalemia
c) Hypernatremia
d) Hypermagnesemia
Answer: b) Hypokalemia
4. Digoxin’s action on the AV node causes:
a) Increased conduction
b) Decreased conduction
c) Widened QRS
d) Tachycardia
Answer: b) Decreased conduction
5. Classic visual disturbance in digoxin toxicity:
a) Blue vision
b) Red vision
c) Yellow-green vision
d) Tunnel vision
Answer: c) Yellow-green vision
FAQs
Q1. Why is digoxin useful in atrial fibrillation?
Because it slows AV nodal conduction via vagal stimulation.
Q2. Does digoxin improve survival in heart failure?
No—it improves symptoms but does not reduce mortality.
Q3. What electrolyte increases digoxin toxicity?
Hypokalemia, which increases digoxin binding to Na⁺/K⁺-ATPase.
Q4. How is digoxin toxicity treated?
With digoxin-specific antibody fragments (Digibind).
Q5. Can renal failure cause digoxin toxicity?
Yes—digoxin clearance is reduced.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com
