Table of Contents
Introduction
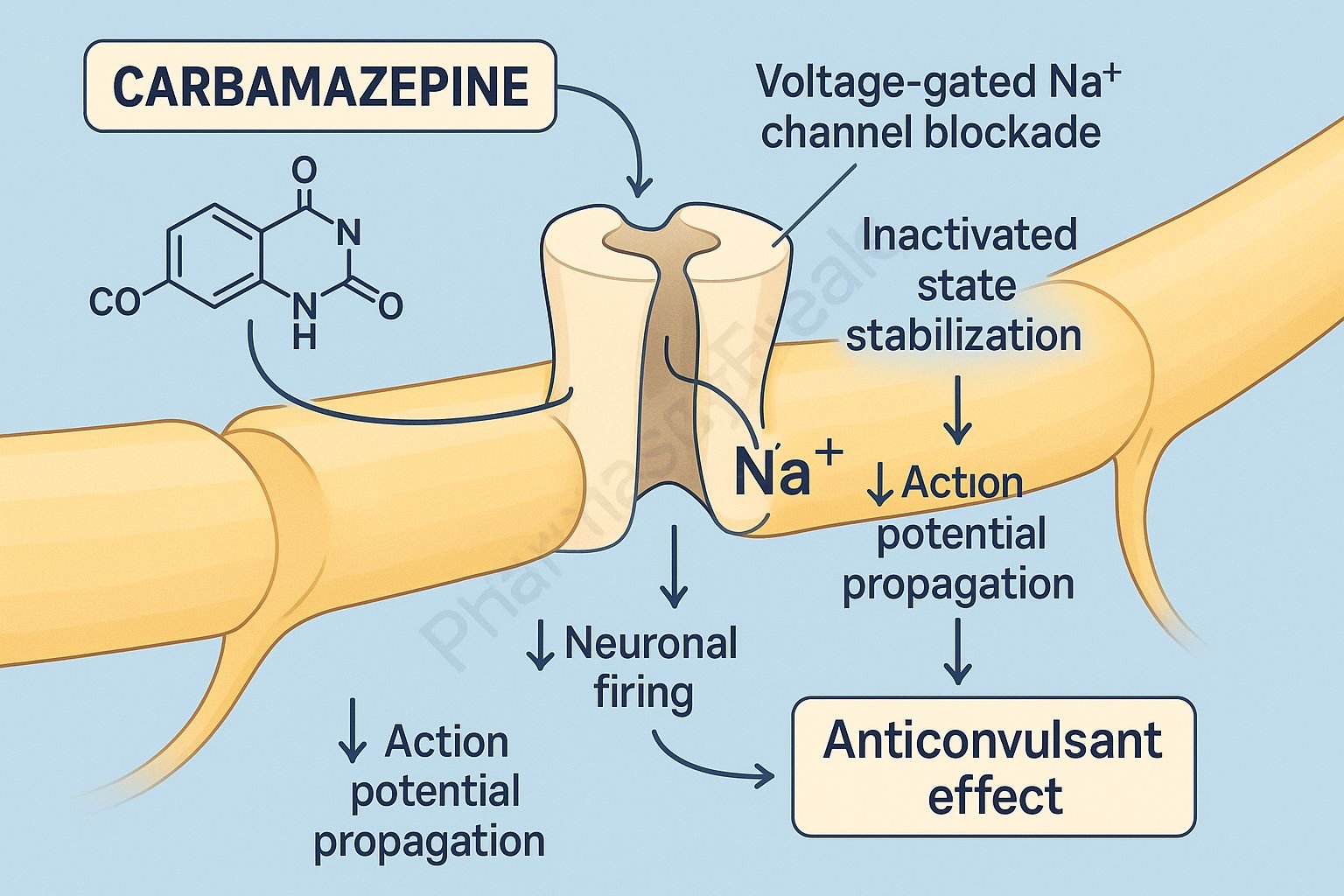
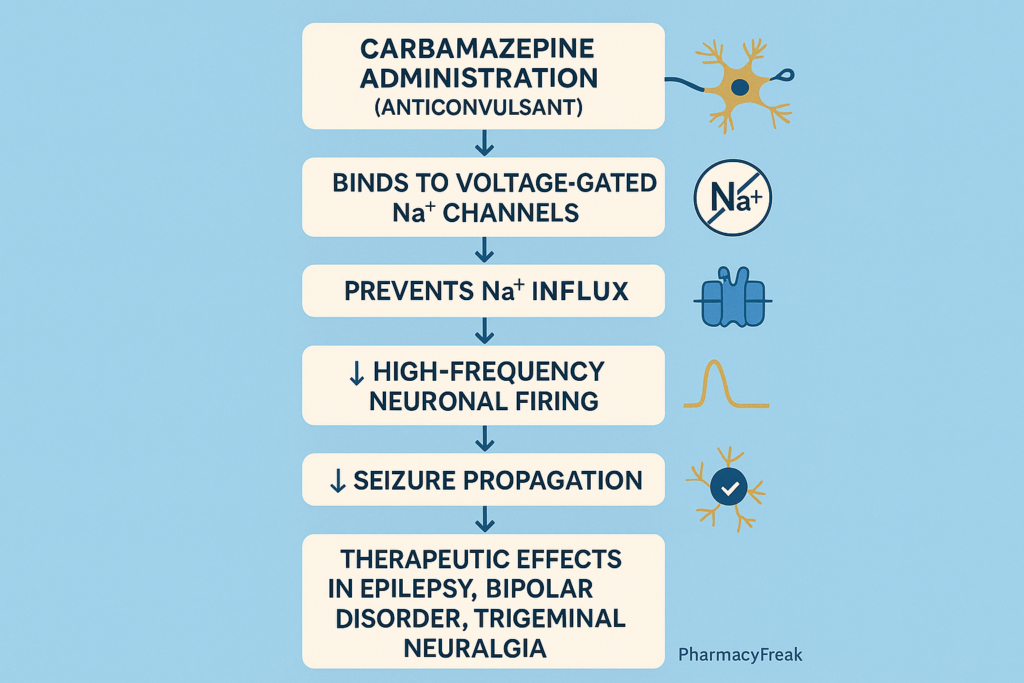
Carbamazepine is a widely used antiepileptic and mood-stabilizing drug effective in the management of partial seizures, generalized tonic–clonic seizures, trigeminal neuralgia, and bipolar disorder. It stabilizes hyperexcitable neuronal membranes and reduces synaptic transmission.
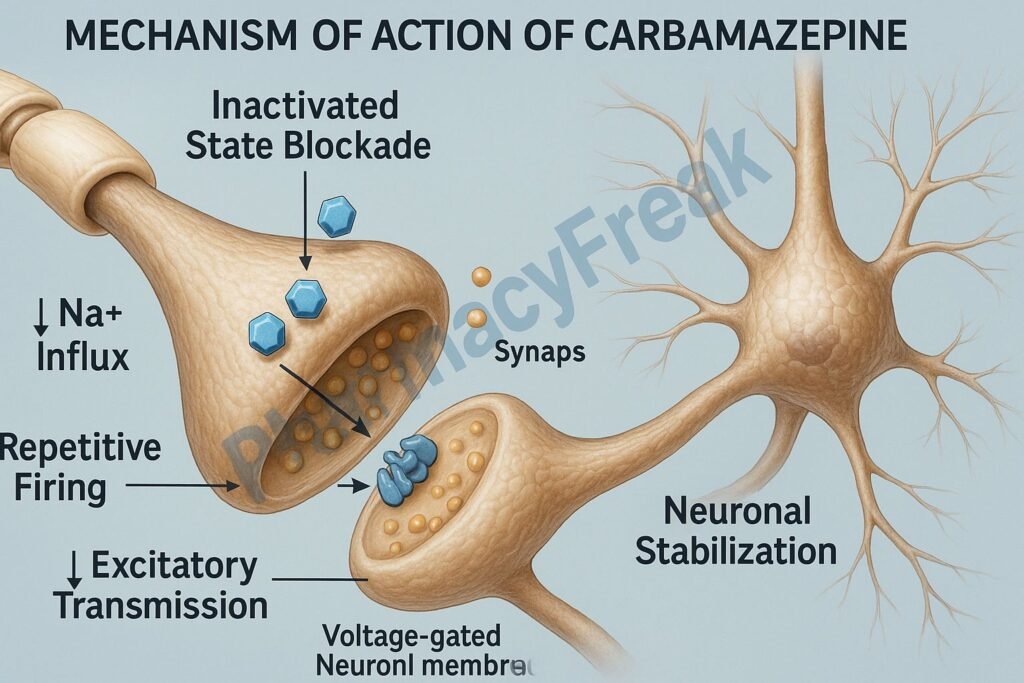
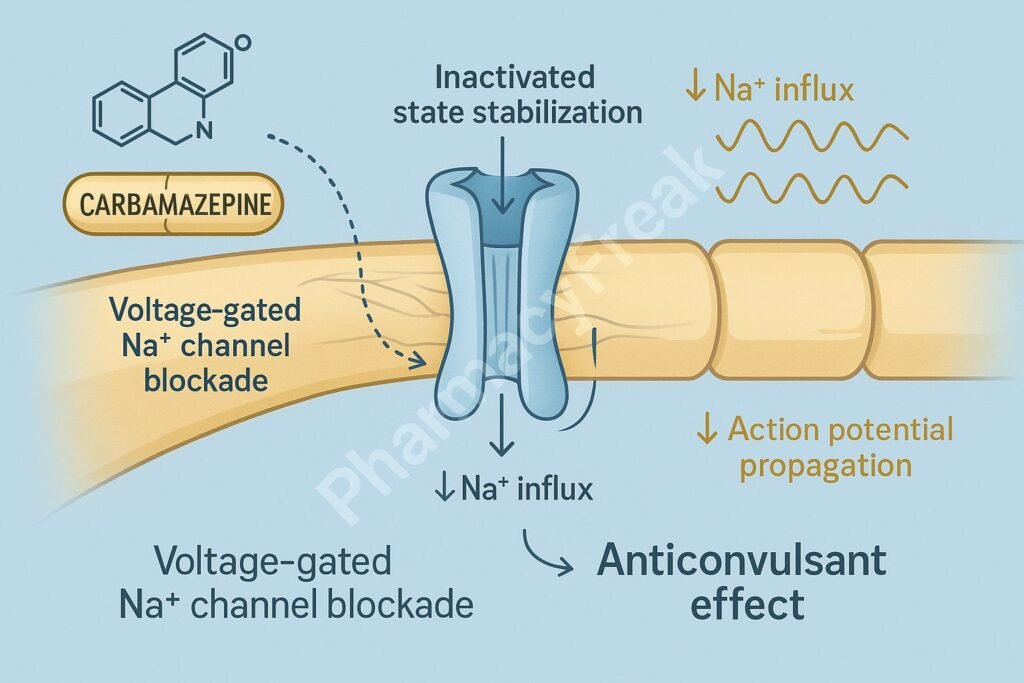
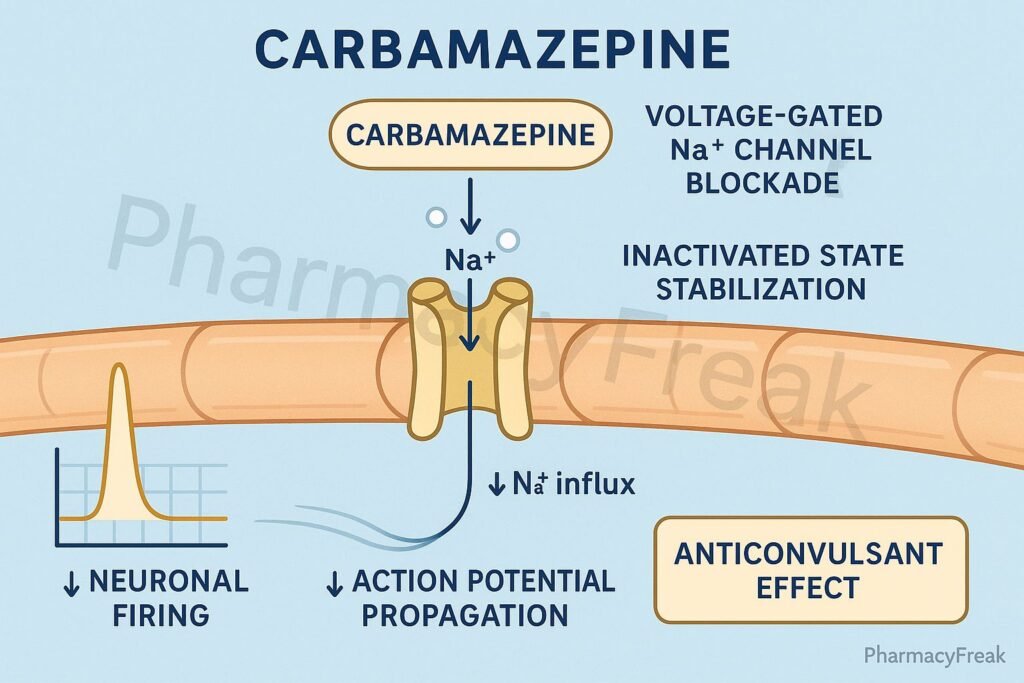
The Mechanism of Action of Carbamazepine is centered on use-dependent blockade of voltage-gated sodium channels, which reduces repetitive neuronal firing and prevents seizure propagation.
Mechanism of Action (Step-wise)
1. Voltage-Gated Sodium Channel Blockade – Primary Mechanism
Carbamazepine binds preferentially to the inactivated state of voltage-gated Na⁺ channels.
Effects:
- ↓ High-frequency repetitive firing
- ↓ Neuronal excitability
- ↓ Seizure propagation
- Stabilization of neuronal membranes
This is the major mechanism for its antiepileptic activity.
2. Use-Dependent Block
Carbamazepine produces greater inhibition in rapidly firing neurons, a feature that:
- Enhances its efficacy in epileptic discharges
- Reduces adverse effects on normal neuronal activity
3. Decreased Excitatory Neurotransmission
By inhibiting sodium channels, it indirectly:
- ↓ Glutamate release
- ↓ Synaptic excitation
This contributes to seizure control and mood stabilization.
4. Potentiation of GABAergic Inhibition (Minor Mechanism)
Carbamazepine may slightly enhance:
- Action of GABA
- Inhibitory neurotransmission
This is not the main mechanism but adds to its anticonvulsant effect.
5. Mood-Stabilizing Effects
Mechanism not fully understood, but involves:
- Sodium channel blockade
- Reduced glutamatergic excitation
- Modulation of monoaminergic pathways
Used in bipolar disorder as an alternative to lithium.
6. Summary of Mechanism
| Mechanism | Effect |
|---|---|
| Na⁺ channel inactivation | ↓ Neuronal firing |
| Use-dependent block | Targeted seizure suppression |
| ↓ Glutamate release | Less excitation |
| Mild GABA enhancement | Supportive inhibition |
| Membrane stabilization | Prevents seizure spread |
Pharmacokinetics
- Absorption: Slow & variable
- Protein binding: 75%
- Metabolism: Extensive hepatic (CYP3A4)
- Active metabolite: Carbamazepine-10,11-epoxide
- Autoinduction: Induces its own metabolism over 2–4 weeks
- Half-life:
- Initial: 25–65 hours
- With autoinduction: 12–17 hours
- Excretion: Renal
Clinical Uses
- Partial seizures
- Generalized tonic–clonic seizures
- Trigeminal neuralgia
- Bipolar disorder (mania)
- Glossopharyngeal neuralgia
- Alcohol withdrawal seizures (adjunct)
Adverse Effects
Common
- Dizziness
- Drowsiness
- Diplopia
- Ataxia
- Nausea/vomiting
Serious
- Agranulocytosis
- Aplastic anemia
- Stevens–Johnson syndrome (SJS)
- Toxic epidermal necrolysis (TEN)
- Hyponatremia (SIADH)
- Hepatotoxicity
HLA-B*1502 allele in Asians increases SJS/TEN risk.
Contraindications
- Bone marrow depression
- Pregnancy (teratogenic—neural tube defects)
- Use with MAO inhibitors
- Hypersensitivity to tricyclic antidepressants
Comparative Analysis
| Feature | Carbamazepine | Phenytoin | Valproate |
|---|---|---|---|
| Mechanism | Na⁺ channel block | Na⁺ channel block | Broad spectrum |
| Autoinduction | Yes | No | No |
| Mood stabilizer | Yes | No | Yes |
| Hyponatremia | High risk | Low | Low |
| SJS risk (HLA-B*1502) | High | Moderate | Low |
MCQs
1. Carbamazepine acts primarily by blocking:
a) Calcium channels
b) GABA receptors
c) Voltage-gated sodium channels
d) Potassium channels
Answer: c) Voltage-gated sodium channels
2. Carbamazepine is particularly effective in:
a) Absence seizures
b) Partial seizures
c) Myoclonic seizures
d) Atonic seizures
Answer: b) Partial seizures
3. A serious adverse effect of carbamazepine is:
a) Hypokalemia
b) Aplastic anemia
c) Hypercalcemia
d) Hypothyroidism
Answer: b) Aplastic anemia
4. Carbamazepine induces its own metabolism by:
a) Inhibiting CYP3A4
b) Autoinduction of CYP3A4
c) Increasing renal excretion
d) Decreasing protein binding
Answer: b) Autoinduction of CYP3A4
5. Genetic testing for which allele is recommended?
a) HLA-B1502
b) HLA-A0201
c) HLA-C0702
d) HLA-DR4
**Answer: a) HLA-B1502**
FAQs
Q1. Why is carbamazepine not used for absence seizures?
It can worsen them due to sodium channel effects.
Q2. Does carbamazepine cause hyponatremia?
Yes—due to SIADH.
Q3. Why does the dose need adjustment over time?
Because carbamazepine induces its own metabolism (autoinduction).
Q4. Is carbamazepine safe during pregnancy?
No—teratogenic risk, especially neural tube defects.
Q5. What monitoring is required?
CBC, liver function tests, and serum sodium.
References
Goodman & Gilman’s Pharmacological Basis of Therapeutics
https://accesspharmacy.mhmedical.com/book.aspx?bookid=2189
Katzung: Basic and Clinical Pharmacology
https://accessmedicine.mhmedical.com/book.aspx?bookid=2464
Tripathi: Essentials of Medical Pharmacology
https://jaypeebrothers.com/
Harrison’s Principles of Internal Medicine
https://accessmedicine.mhmedical.com/book.aspx?bookid=2129

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com