Tuberculosis (TB) is a chronic infectious disease caused primarily by Mycobacterium tuberculosis. It affects the lungs most commonly but can involve other organs. The treatment of TB requires prolonged multidrug therapy to ensure complete eradication and prevent resistance. Antitubercular drugs are classified according to their mechanism of action and their role in treatment regimens.
This blog from Pharmacy Freak explains the classification, uses, drug of choice, side effects, and updated treatment protocols as per standard guidelines and pharmacological references.
Table of Contents
What is Antitubercular Drug
Antitubercular drugs are medications used to treat tuberculosis by killing or inhibiting the growth of Mycobacterium tuberculosis. They are used in various combinations to prevent resistance and ensure efficacy.
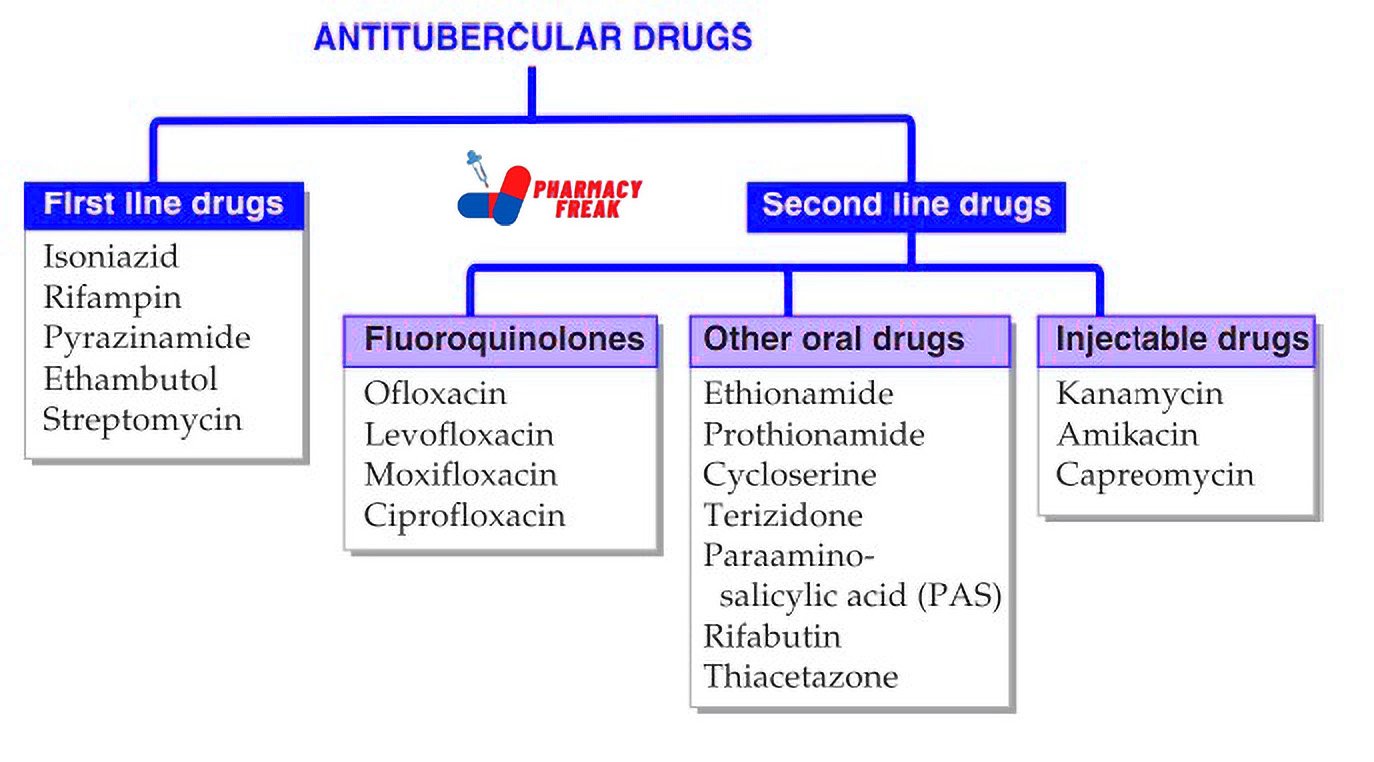
Classification of Antitubercular Drug (KD Tripathi)
- First line drugs: Isoniazid, Rifampin, Pyrazinamide, Ethambutol, Streptomycin
- Second line drugs
– Fluoroquinolones: Ofloxacin, Levofloxacin, Moxifloxacin, Ciprofloxacin
– Other oral drugs: Ethionamide, Prothionamide, Cycloserine, Terizidone, Paraaminosalicylic acid (PAS), Rifabutin, Thiacetazone
– Injectable drugs: Kanamycin, Amikacin, Capreomycin
Classification of Antitubercular Drug (General)
Antitubercular drugs are classified into first-line and second-line agents. They can also be grouped based on their bactericidal or bacteriostatic action and specific role in therapy.
- First-Line Antitubercular Drugs
Isoniazid (INH)
Rifampicin
Pyrazinamide
Ethambutol
Streptomycin
These are the most effective drugs used in the initial phase of treatment - Second-Line Antitubercular Drugs
Fluoroquinolones – Levofloxacin, Moxifloxacin
Injectable agents – Amikacin, Kanamycin, Capreomycin
Other oral agents – Ethionamide, Prothionamide, Cycloserine, Terizidone, Para-aminosalicylic acid (PAS)
Used in drug-resistant or MDR/XDR TB - Newer Drugs for MDR and XDR TB
Bedaquiline
Delamanid
Pretomanid
Used in rifampicin-resistant or extensively drug-resistant TB cases under WHO guidelines - Classification based on Mechanism of Action
a. Inhibitors of mycolic acid synthesis – Isoniazid
b. Inhibitors of RNA synthesis – Rifampicin
c. Inhibitors of cell wall synthesis – Ethambutol, Cycloserine
d. Inhibitors of ATP synthase – Bedaquiline
e. Disruptors of membrane potential – Pyrazinamide
f. Protein synthesis inhibitors – Streptomycin, Amikacin, Kanamycin, Capreomycin, PAS, Linezolid - Classification based on Bactericidal or Bacteriostatic Action
Bactericidal – Isoniazid, Rifampicin, Pyrazinamide, Streptomycin, Bedaquiline
Bacteriostatic – Ethambutol, PAS, Ethionamide, Cycloserine
Uses
- Pulmonary tuberculosis
- Extrapulmonary tuberculosis (e.g., lymph node, spinal, meningitis)
- Latent TB infection (INH monotherapy or INH + Rifapentine)
- MDR-TB and XDR-TB
- Prophylaxis in high-risk contacts
- TB in special populations (HIV, pregnancy, pediatric, renal impairment)
Drug of Choice Highlights
- Pulmonary TB – HRZE regimen (Isoniazid, Rifampicin, Pyrazinamide, Ethambutol)
- Latent TB – Isoniazid for 6–9 months or Rifapentine + Isoniazid weekly for 3 months
- Meningeal TB – HRZE + corticosteroids
- MDR-TB – Based on drug sensitivity test; includes Levofloxacin, Amikacin, Bedaquiline
- TB in pregnancy – Avoid Streptomycin and use HRZE with caution
- TB in HIV – Same drugs; Rifabutin may be used instead of Rifampicin due to drug interactions with ART
Side Effects
- Isoniazid – Hepatotoxicity, peripheral neuropathy (prevented with pyridoxine), lupus-like syndrome
- Rifampicin – Hepatotoxicity, orange discoloration of body fluids, flu-like syndrome
- Pyrazinamide – Hepatotoxicity, hyperuricemia, arthralgia
- Ethambutol – Optic neuritis (reversible if stopped early), color vision loss
- Streptomycin – Ototoxicity, nephrotoxicity
- Fluoroquinolones – Tendonitis, QT prolongation
- Bedaquiline – QT prolongation, hepatotoxicity
- Delamanid – QT prolongation
- Cycloserine – Neurotoxicity, psychosis
- PAS – GI upset, hypersensitivity reactions
Updated Clinical Pearls
- Isoniazid and Rifampicin are the most effective bactericidal agents and form the backbone of all regimens
- Fixed-dose combinations (FDCs) are used to improve compliance and reduce resistance
- Vitamin B6 (pyridoxine) supplementation is essential with INH to prevent peripheral neuropathy
- WHO recommends using shorter regimens with Bedaquiline for MDR-TB where feasible
- Therapeutic drug monitoring is advised in special populations such as renal or hepatic impairment
- Patients on Rifampicin require monitoring for drug interactions, especially with antiretrovirals, oral contraceptives, and anticoagulants
- DOTS (Directly Observed Treatment Short Course) remains the cornerstone of TB control in public health programs
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 867–876
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023.
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 1547–1559
Related Links

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com