Amoebiasis is a parasitic infection caused by Entamoeba histolytica. It may present as asymptomatic cyst passage, intestinal amoebiasis (dysentery), or extraintestinal manifestations like liver abscess. Treatment depends on the severity, site of infection, and form of the parasite involved. Antiamoebic drugs are categorized based on the tissue site where they act.
This blog from Pharmacy Freak discusses the classification of Antiamoebic Drugs, clinical uses, preferred drugs, side effects, and updated treatment pearls essential for pharmacology exam preparation and practice.
Table of Contents
What is Antiamoebic Drugs
Antiamoebic drugs are agents used to treat infections caused by Entamoeba histolytica. These drugs act on the parasite in its trophozoite and cystic stages, either in the intestinal lumen, intestinal wall, or extraintestinal tissues.
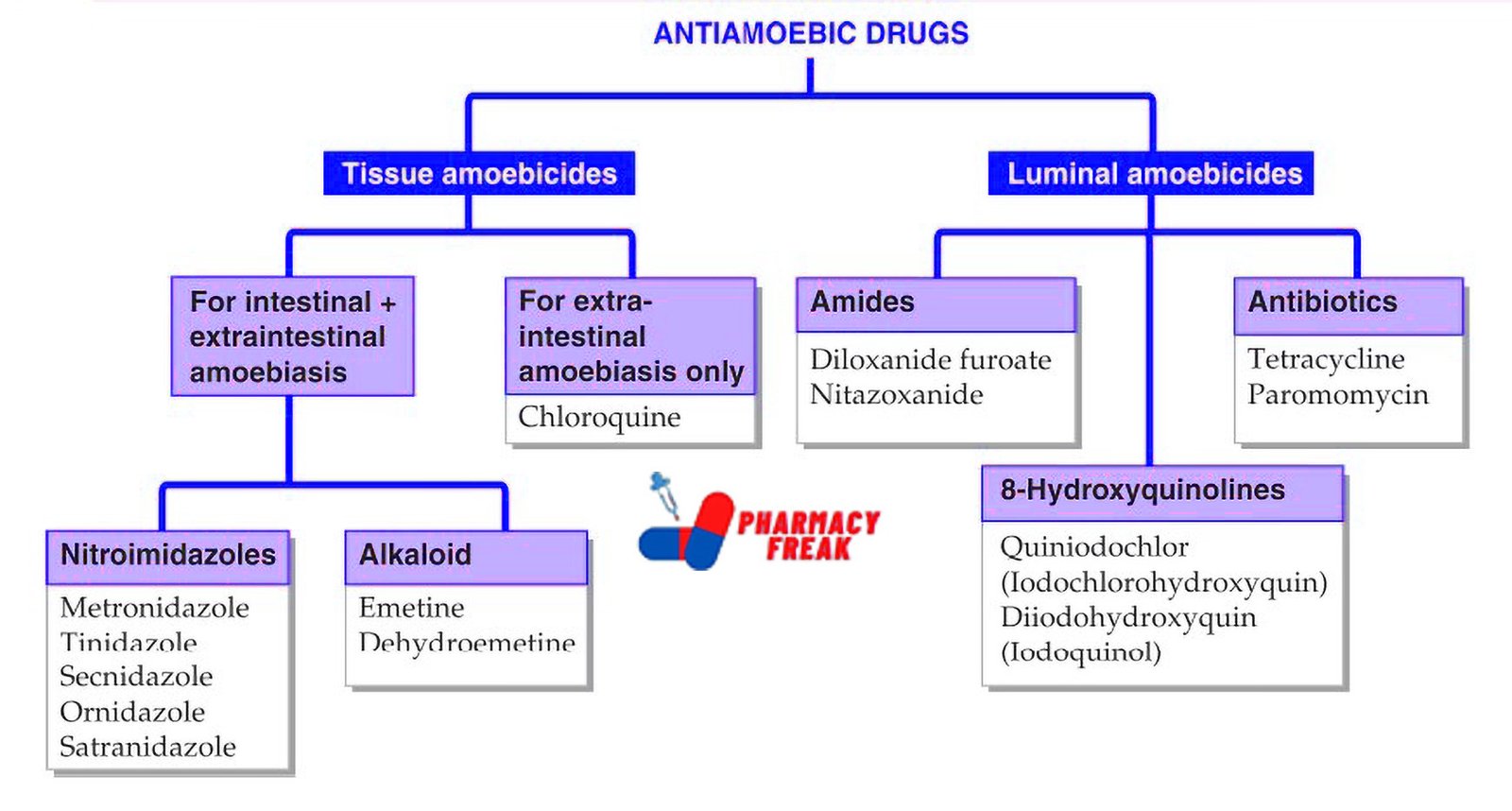
Classification of Antiamoebic Drugs (KD Tripathi)
- Tissue amoebicides –
- Fo intestinal + extraintestinal amoebiasis:
- Nitroimidazoles: Metronidazole, Tinidazole, Secnidazole, Ornidazole, Satranidazole
- Alkaloid: Emetine, Dehydroemetine
- For extraintestinal amoebiasis only: Chloroquine
- Luminal amoebicides –
- Amides: Diloxanide furoate, Nitazoxanide
- Antibiotics: Tetracycline, Paromomycin
- 8–Hydroxyquinolines: Quiniodochlor (Iodochlorohydroxyquin), Diiodohydroxyquin (Iodoquinol)
Classification of Penicillin (General)
Antiamoebic drugs are classified according to their site of action into three main groups:
- Luminal Amoebicides
Act only in the intestinal lumen on cysts and non-invasive trophozoites
Examples:
- Diloxanide furoate
- Paromomycin
- Iodoquinol
- Tetracycline (as adjunct)
Use: Asymptomatic carriers, to eradicate cysts after treatment of invasive disease
- Tissue Amoebicides
Act on the trophozoites in the intestinal wall and extraintestinal tissues
Examples:
- Metronidazole
- Tinidazole
- Ornidazole
- Secnidazole
Use: Intestinal amoebiasis (dysentery), liver abscess, and other extraintestinal forms
- Mixed Amoebicides
Act in both the intestinal lumen and tissues
Examples:
- Metronidazole (partial luminal activity)
- Tinidazole
- Ornidazole
Use: Most commonly used drugs in clinical practice due to dual action
- Adjunctive Agents
Used in combination to treat severe or complicated infections
Examples:
- Chloroquine – Used for hepatic amoebiasis (reaches liver abscess cavity)
- Emetine and Dehydroemetine – Potent but toxic; rarely used today
Uses
Antiamoebic drugs are used for:
- Asymptomatic intestinal cyst carriers
- Amoebic dysentery (intestinal amoebiasis)
- Amoebic liver abscess and other extraintestinal infections
- Mixed bacterial and amoebic diarrhoea
- Pre- and post-operative management of intestinal amoebiasis
- Prophylaxis in high-risk populations (not routinely recommended)
Drug of Choice Highlights
- Asymptomatic cyst carriers – Diloxanide furoate or Paromomycin
- Intestinal amoebiasis – Metronidazole followed by a luminal agent
- Liver abscess – Metronidazole or Tinidazole + Chloroquine (if needed)
- Severe amoebic dysentery – Metronidazole + Diloxanide furoate
- Mixed infections (e.g., with Giardia) – Metronidazole
- Pregnancy – Paromomycin (category B, non-absorbable)
Side Effects
- Metronidazole – Metallic taste, nausea, headache, disulfiram-like reaction with alcohol, neurotoxicity (rare)
- Tinidazole – Similar to metronidazole but better tolerated and longer acting
- Diloxanide furoate – Flatulence, GI upset
- Paromomycin – Nausea, abdominal pain; may cause ototoxicity or nephrotoxicity with systemic absorption
- Chloroquine – GI disturbances, visual disturbances, pruritus
- Emetine – Cardiotoxicity, muscle weakness; use limited to resistant or severe cases only
Updated Clinical Pearls
- Metronidazole is the most commonly used drug for amoebiasis and provides rapid relief in intestinal and hepatic infections.
- It does not completely eradicate luminal cysts; hence, it must be followed by a luminal amoebicide to prevent relapse or carrier state.
- Tinidazole has a longer half-life and better compliance due to once-daily dosing.
- Chloroquine is effective in amoebic liver abscesses but does not act in the intestine and must be combined with a luminal agent.
- Emetine and Dehydroemetine are now rarely used due to high toxicity.
- Paromomycin is preferred in pregnancy due to its poor absorption and safety profile.
- Combination therapy with metronidazole and diloxanide is the standard of care in most invasive amoebic diseases.
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 888–892
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 304–306
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 1561–1565
Related Links

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com