Table of Contents
Introduction
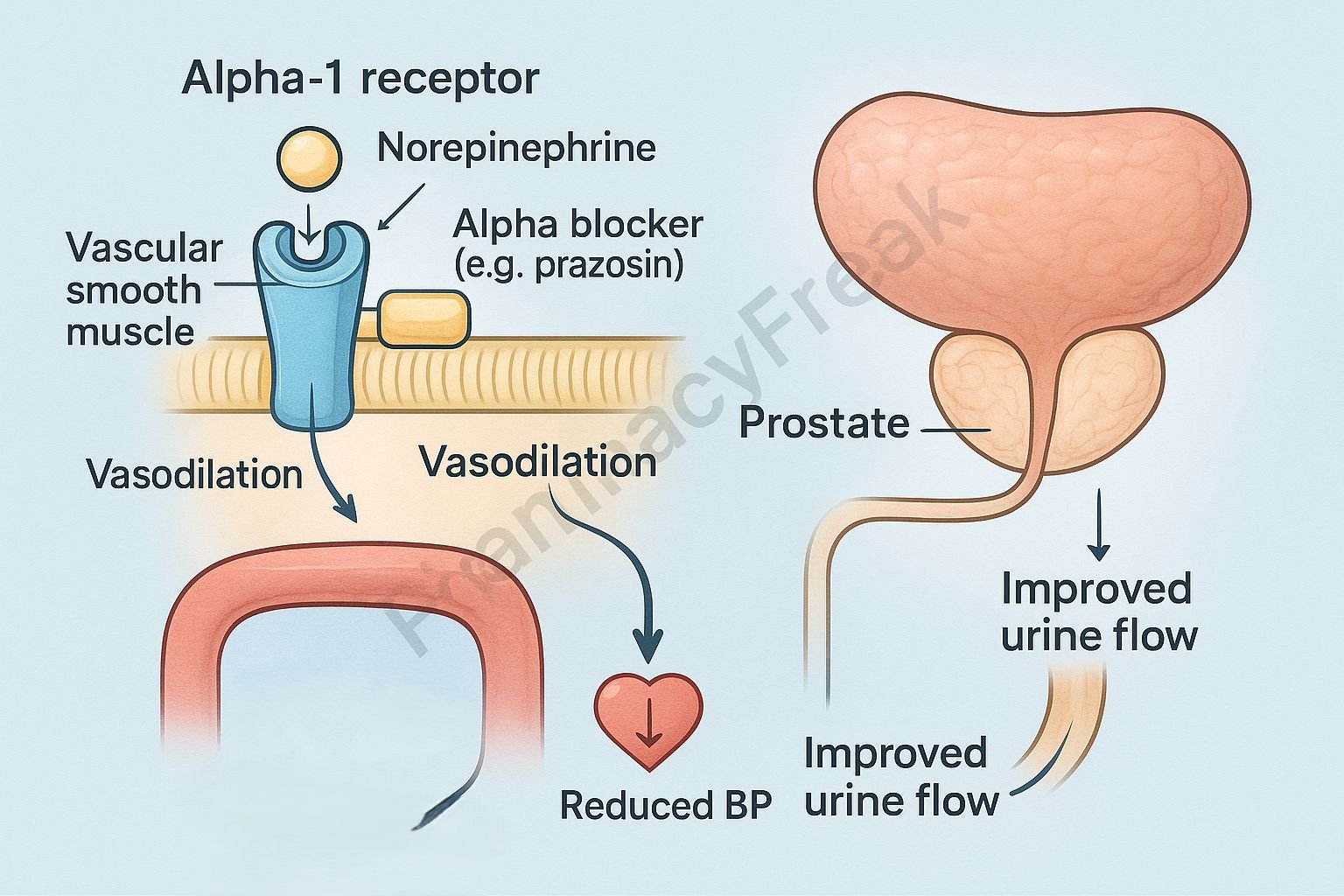
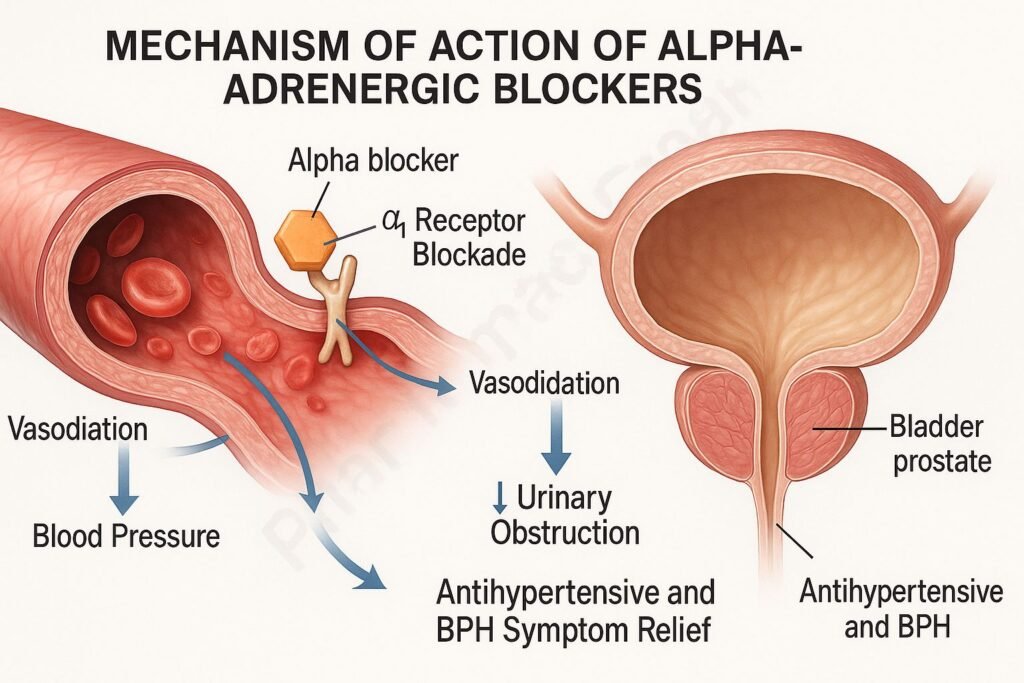
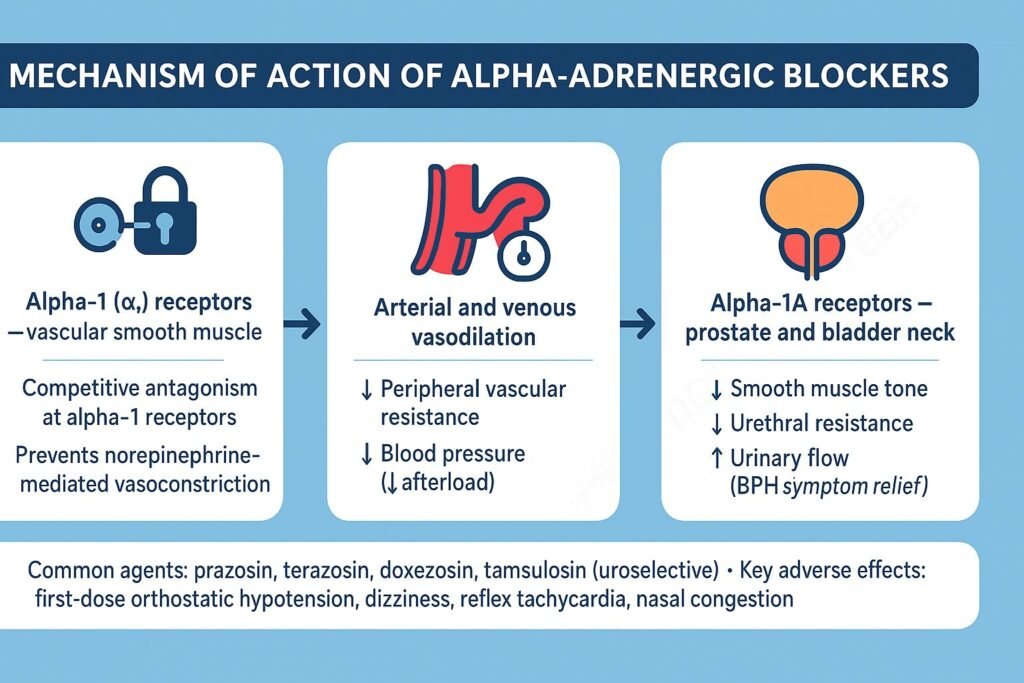
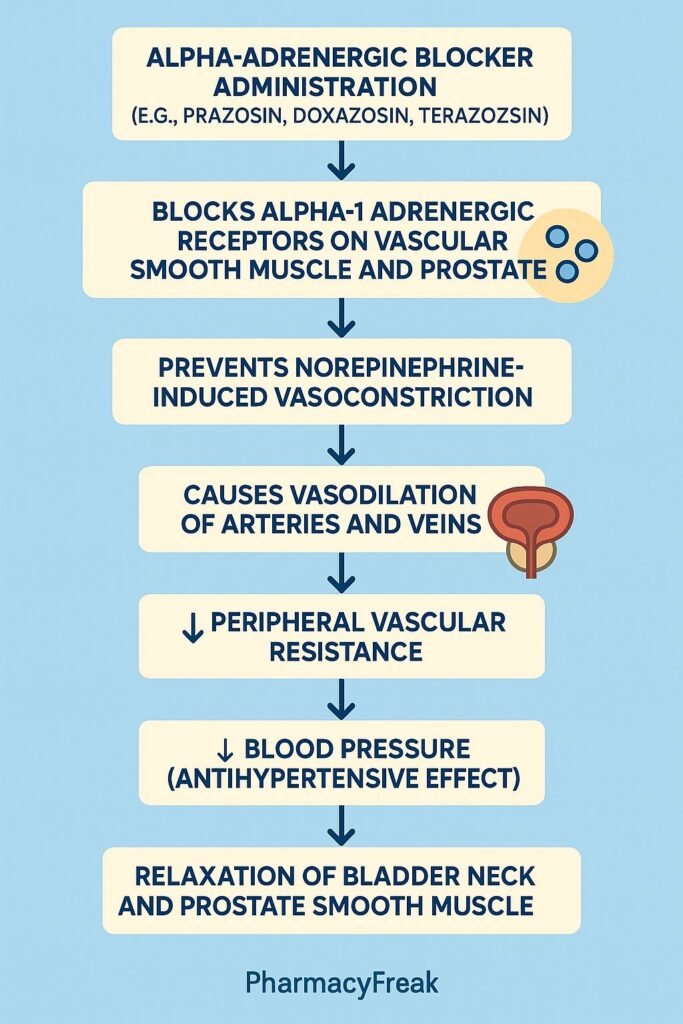
Alpha-adrenergic blockers, also called alpha-blockers, are a class of drugs that antagonize the effects of catecholamines (epinephrine and norepinephrine) at alpha-adrenergic receptors. Mechanism of Action of Alpha-Adrenergic Blockers involves inhibition of alpha-1 and/or alpha-2 receptors, resulting in vasodilation, decreased peripheral vascular resistance, and reduced blood pressure. These drugs are commonly used in the management of hypertension, benign prostatic hyperplasia (BPH), and certain vascular disorders.
Mechanism of Action (Step-wise)
- Blockade of Alpha-Adrenergic Receptors
- Alpha-blockers competitively inhibit the binding of norepinephrine to alpha-adrenergic receptors located on vascular smooth muscle.
- Depending on selectivity, they may block alpha-1, alpha-2, or both receptor types.
- Vascular Effects (Alpha-1 Blockade)
- Alpha-1 receptors mediate vasoconstriction via increased intracellular calcium.
- Blocking these receptors leads to vascular smooth muscle relaxation, resulting in vasodilation and decreased systemic vascular resistance.
- This reduces blood pressure and afterload on the heart.
- Effects on Prostate and Bladder Neck
- In the prostate and bladder neck, alpha-1A receptors mediate smooth muscle tone.
- Alpha-1A blockers (e.g., tamsulosin) relax these muscles, improving urine flow and reducing BPH symptoms.
- Reflex Tachycardia (Alpha-2 Blockade)
- Non-selective alpha blockers (e.g., phentolamine) also block alpha-2 receptors presynaptically, leading to increased norepinephrine release.
- This can cause reflex tachycardia and enhanced cardiac stimulation.
- Overall Effect
- Alpha-1 Selective Blockers: Vasodilation → ↓ Blood Pressure → ↓ Afterload.
- Non-Selective Blockers: Vasodilation + Reflex tachycardia.
- Prostate-Selective Blockers: Relaxation of bladder outlet → Improved urine flow.
Pharmacokinetics
- Absorption: Well absorbed orally; food may delay absorption but reduce first-dose hypotension.
- Distribution: Widely distributed; highly protein bound.
- Metabolism: Mainly hepatic via CYP enzymes.
- Excretion: Renal and biliary routes.
- Half-life: Varies—short (phentolamine) to long (doxazosin).
Clinical Uses
- Hypertension: Doxazosin, Prazosin, Terazosin.
- Benign prostatic hyperplasia (BPH): Tamsulosin, Alfuzosin, Silodosin.
- Pheochromocytoma: Phenoxybenzamine, Phentolamine (pre-operative control of blood pressure).
- Raynaud’s disease and scleroderma-related vasospasm.
Adverse Effects
- Common: Dizziness, postural hypotension, fatigue, nasal congestion.
- Less common: Headache, reflex tachycardia, peripheral edema.
- Serious: Syncope (first-dose phenomenon), priapism (rare), arrhythmias (with non-selective agents).
- Contraindications: Severe hepatic impairment, hypotension, or heart failure (use cautiously).
Comparative Analysis
| Feature | Alpha-1 Blockers (e.g., Prazosin) | Non-Selective Blockers (e.g., Phentolamine) | Alpha-1A Blockers (e.g., Tamsulosin) |
|---|---|---|---|
| Primary action | Vasodilation | Vasodilation + reflex tachycardia | Relaxation of prostate & bladder neck |
| Effect on BP | Decrease | Decrease with reflex ↑ HR | Minimal systemic effect |
| Used for | Hypertension, BPH | Pheochromocytoma | BPH only |
| First-dose hypotension | Common | Moderate | Rare |
| CNS effects | Mild dizziness | Significant | Minimal |
MCQs
1. Alpha-adrenergic blockers act by:
a) Stimulating alpha receptors
b) Blocking alpha receptors
c) Activating beta receptors
d) Inhibiting acetylcholine release
Answer: b) Blocking alpha receptors
2. Which receptor subtype mediates vascular smooth muscle contraction?
a) Alpha-1
b) Alpha-2
c) Beta-1
d) Beta-2
Answer: a) Alpha-1
3. Which of the following is a selective alpha-1 blocker?
a) Phentolamine
b) Phenoxybenzamine
c) Prazosin
d) Yohimbine
Answer: c) Prazosin
4. Tamsulosin acts primarily on:
a) Alpha-1B receptors in arteries
b) Alpha-1A receptors in prostate
c) Alpha-2 receptors in CNS
d) Beta-2 receptors in lungs
Answer: b) Alpha-1A receptors in prostate
5. Which adverse effect is most characteristic of alpha blockers?
a) Hypertension
b) Postural hypotension
c) Bradycardia
d) Bronchospasm
Answer: b) Postural hypotension
6. Reflex tachycardia occurs mainly with:
a) Alpha-1 blockers
b) Alpha-2 blockers
c) Non-selective alpha blockers
d) Beta blockers
Answer: c) Non-selective alpha blockers
7. Phenoxybenzamine differs from phentolamine because it:
a) Is reversible
b) Is irreversible
c) Acts only on alpha-2 receptors
d) Has no effect on BP
Answer: b) Is irreversible
8. Alpha blockers are used in which condition?
a) Asthma
b) Hypertension
c) Hypotension
d) Parkinsonism
Answer: b) Hypertension
9. Which is a long-acting alpha-1 blocker?
a) Doxazosin
b) Prazosin
c) Phentolamine
d) Yohimbine
Answer: a) Doxazosin
10. The “first-dose phenomenon” is seen with:
a) Beta blockers
b) Alpha blockers (especially prazosin)
c) Calcium channel blockers
d) ACE inhibitors
Answer: b) Alpha blockers (especially prazosin)
FAQs
Q1. How do alpha blockers lower blood pressure?
They block alpha-1 receptors in blood vessels, leading to vasodilation and reduced peripheral resistance.
Q2. Why is prazosin given at bedtime initially?
To prevent first-dose postural hypotension and fainting.
Q3. What is the difference between selective and non-selective alpha blockers?
Selective alpha-1 blockers act only on vascular receptors, while non-selective agents block both alpha-1 and alpha-2, causing reflex tachycardia.
Q4. Can alpha blockers be used for prostate enlargement?
Yes, alpha-1A blockers like tamsulosin improve urine flow in benign prostatic hyperplasia.
Q5. Why are alpha blockers used in pheochromocytoma?
They control blood pressure by blocking excessive catecholamine-induced vasoconstriction.
Q6. What causes the “first-dose effect”?
Sudden vasodilation after the first dose leads to transient hypotension and syncope.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- Clinical Hypertension Guidelines (JNC-8, ESC/ESH)
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com