Table of Contents
Introduction
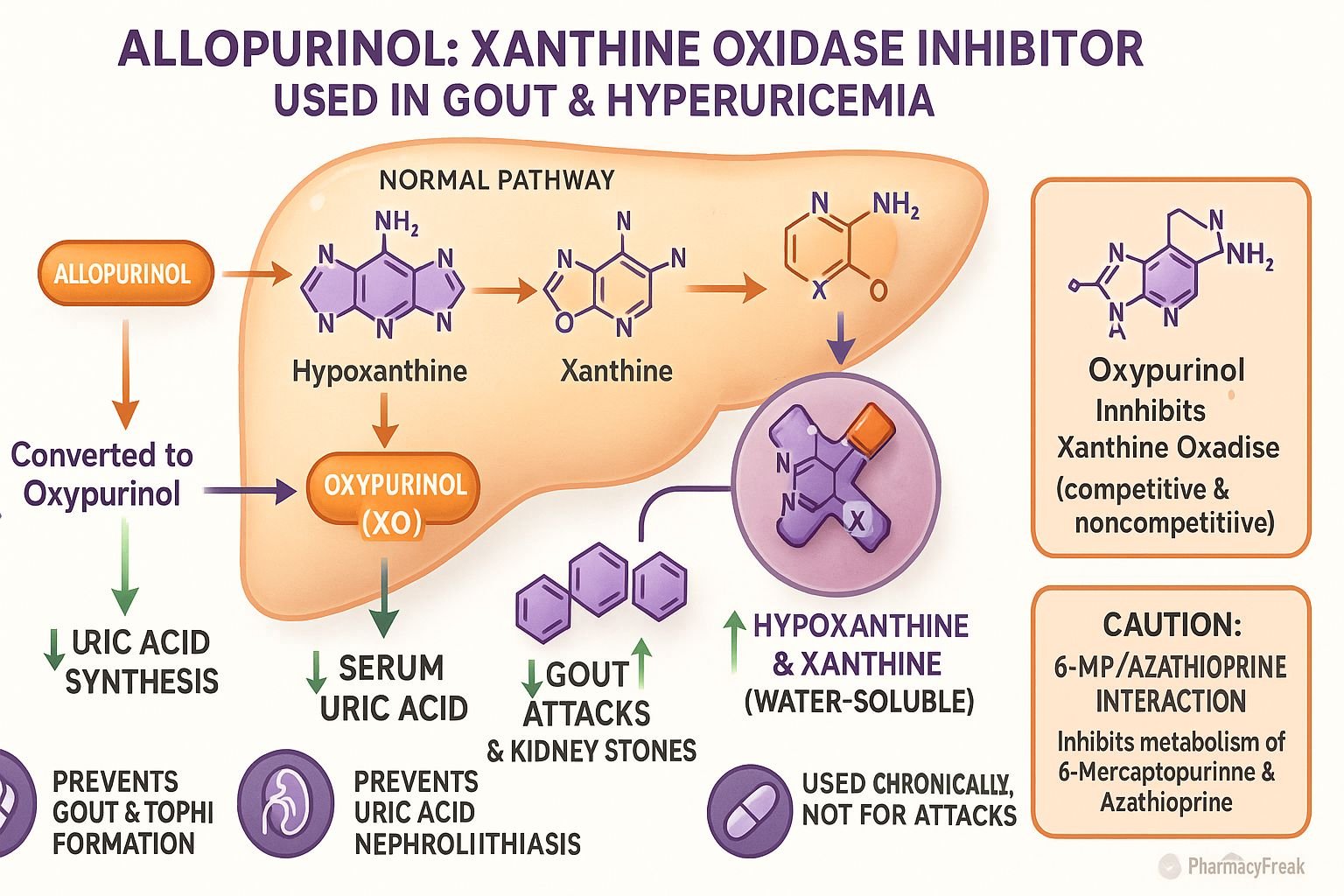
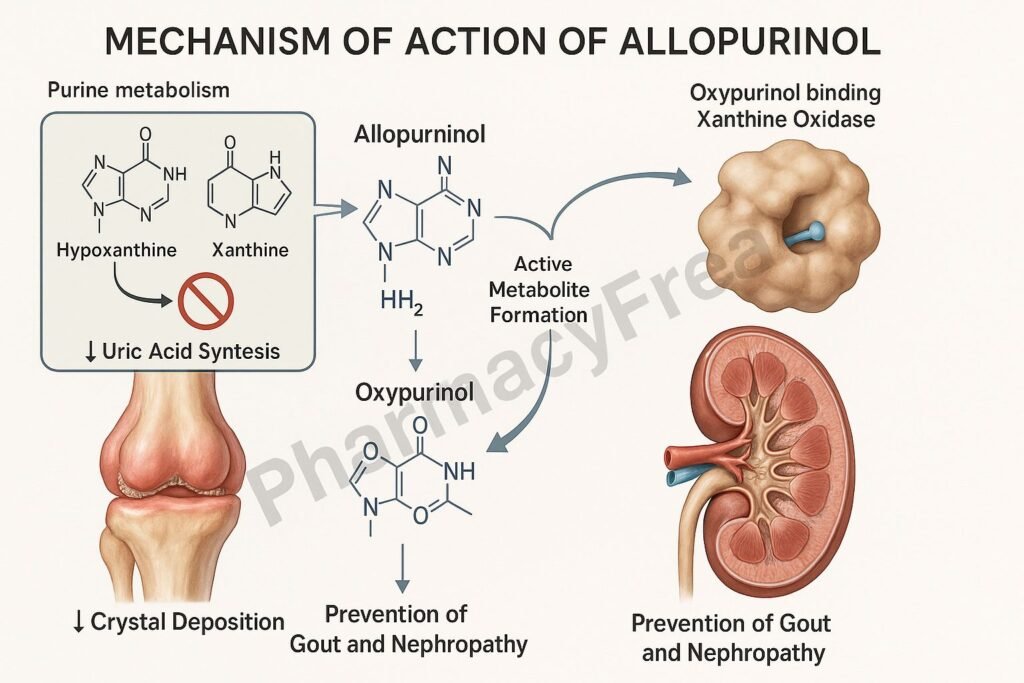
Allopurinol is a xanthine oxidase inhibitor used primarily in the management of gout and hyperuricemia associated with malignancy or chemotherapy. Mechanism of Action of Allopurinol involves inhibition of uric acid production by blocking the enzyme xanthine oxidase, thereby reducing serum uric acid levels and preventing crystal deposition in joints and tissues. It is a cornerstone drug in chronic gout therapy and in preventing tumor lysis–related uric acid nephropathy.
Mechanism of Action (Step-wise)
- Normal Uric Acid Production Pathway
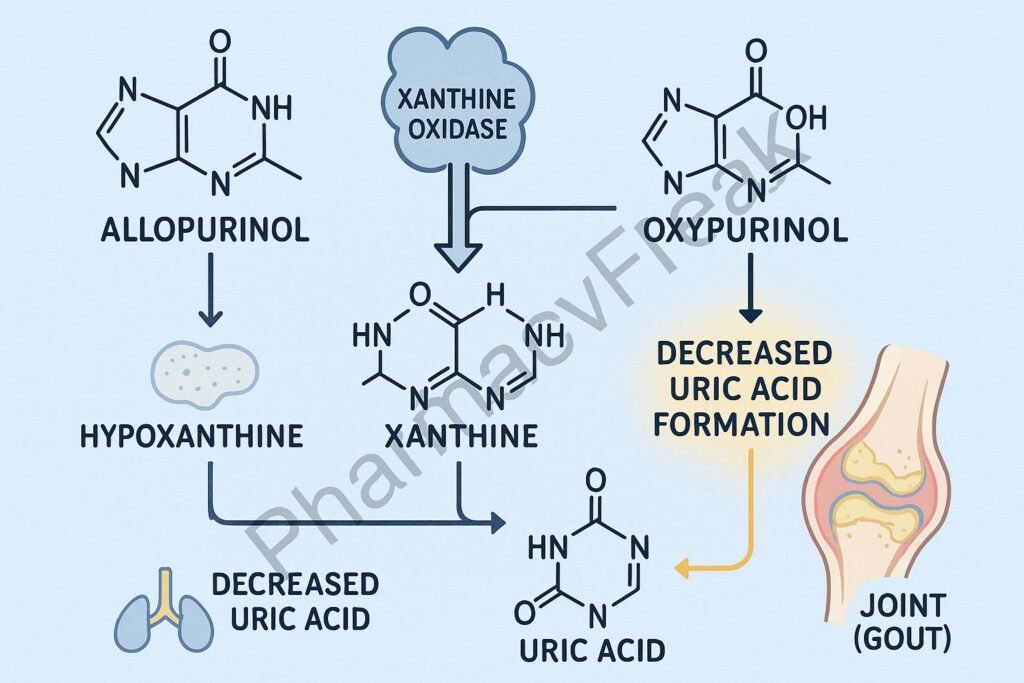
- Purine metabolism produces hypoxanthine and xanthine.
- The enzyme xanthine oxidase converts hypoxanthine → xanthine → uric acid.
- Excess uric acid can crystallize and deposit in joints, kidneys, and soft tissues, causing gout.
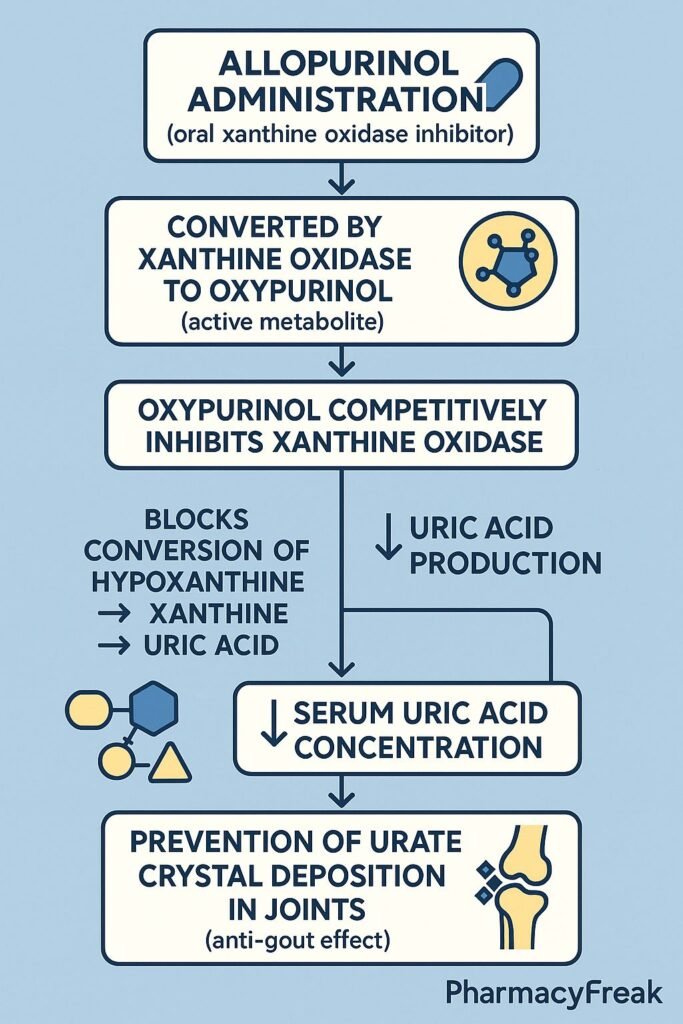
- Allopurinol Conversion to Oxypurinol
- Allopurinol is a structural analog of hypoxanthine.
- After administration, it is metabolized by xanthine oxidase to oxypurinol (alloxanthine), which is an active metabolite with a long half-life.
- Inhibition of Xanthine Oxidase
- Both allopurinol and oxypurinol inhibit xanthine oxidase competitively.
- This blocks the conversion of hypoxanthine and xanthine to uric acid.
- Reduction of Uric Acid Levels
- Decreased uric acid formation prevents new crystal formation and promotes dissolution of existing urate crystals.
- Increased levels of hypoxanthine and xanthine are more soluble and easily excreted in urine.
- Overall Effect
- Decreases serum uric acid concentration.
- Prevents gout attacks and uric acid nephropathy.
- Does not relieve acute pain but prevents recurrence with long-term use.
Pharmacokinetics
- Absorption: Rapid and complete after oral administration.
- Distribution: Widely distributed, including in extracellular fluids.
- Metabolism: Converted in the liver to oxypurinol, the active metabolite.
- Excretion: Renal (mainly as oxypurinol).
- Half-life: Allopurinol ~2 hours; Oxypurinol ~18–30 hours.
Clinical Uses
- Chronic gout (not for acute attacks).
- Hyperuricemia due to chemotherapy (tumor lysis syndrome).
- Recurrent uric acid kidney stones.
- Lesch–Nyhan syndrome (excess purine production).
- Adjuvant therapy with azathioprine or 6-mercaptopurine (dose adjustment required).
Adverse Effects
- Common: Rash, nausea, diarrhea, drowsiness.
- Less common: Hepatotoxicity, leukopenia, pruritus.
- Serious: Stevens–Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), hypersensitivity reactions.
- Drug Interactions: Inhibits metabolism of azathioprine and 6-mercaptopurine, requiring dose reduction to 25%.
- Contraindications: Known hypersensitivity, caution in renal impairment.
Comparative Analysis
| Feature | Allopurinol | Febuxostat | Colchicine |
|---|---|---|---|
| Mechanism | Xanthine oxidase inhibition | Xanthine oxidase inhibition | Microtubule inhibition |
| Primary use | Chronic gout, hyperuricemia | Chronic gout, hyperuricemia | Acute gout attack management |
| Onset of action | Slow (days to weeks) | Slow (days to weeks) | Rapid (within hours) |
| Metabolism | Hepatic → oxypurinol | Hepatic (non-purine selective) | Hepatic |
| Hypersensitivity risk | Moderate (SJS/TEN possible) | Lower | Minimal |
MCQs
1. Allopurinol acts by inhibiting which enzyme?
a) Adenosine deaminase
b) Xanthine oxidase
c) Guanylate cyclase
d) Phosphodiesterase
Answer: b) Xanthine oxidase
2. The active metabolite of allopurinol is:
a) Alloxanthine (oxypurinol)
b) Hypoxanthine
c) Xanthine
d) Uric acid
Answer: a) Alloxanthine (oxypurinol)
3. Allopurinol reduces plasma uric acid levels by:
a) Increasing renal excretion of uric acid
b) Inhibiting uric acid synthesis
c) Enhancing purine degradation
d) Increasing uricase activity
Answer: b) Inhibiting uric acid synthesis
4. Allopurinol is contraindicated in:
a) Hypertension
b) Hypersensitivity to xanthine oxidase inhibitors
c) Diabetes
d) Dyslipidemia
Answer: b) Hypersensitivity to xanthine oxidase inhibitors
5. Which of the following drugs requires dose reduction when used with allopurinol?
a) Colchicine
b) Azathioprine
c) Indomethacin
d) Probenecid
Answer: b) Azathioprine
6. Allopurinol should not be started during:
a) Intercritical gout period
b) Acute gout attack
c) Tumor lysis syndrome
d) Asymptomatic hyperuricemia
Answer: b) Acute gout attack
7. Which is a serious adverse effect of allopurinol?
a) SJS/TEN
b) Bradycardia
c) Hypotension
d) Tremor
Answer: a) SJS/TEN
8. The onset of allopurinol’s urate-lowering effect occurs in:
a) 6–12 hours
b) 2–3 days
c) 1–2 weeks
d) 1–2 months
Answer: c) 1–2 weeks
9. Allopurinol decreases formation of which metabolite?
a) Hypoxanthine
b) Xanthine
c) Uric acid
d) Adenine
Answer: c) Uric acid
10. In Lesch–Nyhan syndrome, allopurinol helps by:
a) Inhibiting uric acid synthesis
b) Stimulating HGPRT activity
c) Blocking dopamine receptors
d) Increasing purine breakdown
Answer: a) Inhibiting uric acid synthesis
FAQs
Q1. Can allopurinol be used during an acute gout attack?
No, it may worsen symptoms; it should be started after the acute phase resolves.
Q2. What is the starting dose of allopurinol in gout?
Usually 100 mg/day, gradually increased to maintain serum uric acid below 6 mg/dL.
Q3. Why must azathioprine dose be reduced with allopurinol?
Allopurinol inhibits xanthine oxidase, which metabolizes azathioprine; failure to adjust the dose can cause severe toxicity.
Q4. Is febuxostat better than allopurinol?
Febuxostat is more selective and safer in mild renal impairment but more expensive.
Q5. What should be monitored during therapy?
Serum uric acid, liver function tests, renal function, and signs of hypersensitivity.
Q6. Can allopurinol cause rash?
Yes, rash is a common early sign of hypersensitivity; discontinue immediately if severe.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- British National Formulary (BNF) – Allopurinol Monograph
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com