Table of Contents
Introduction
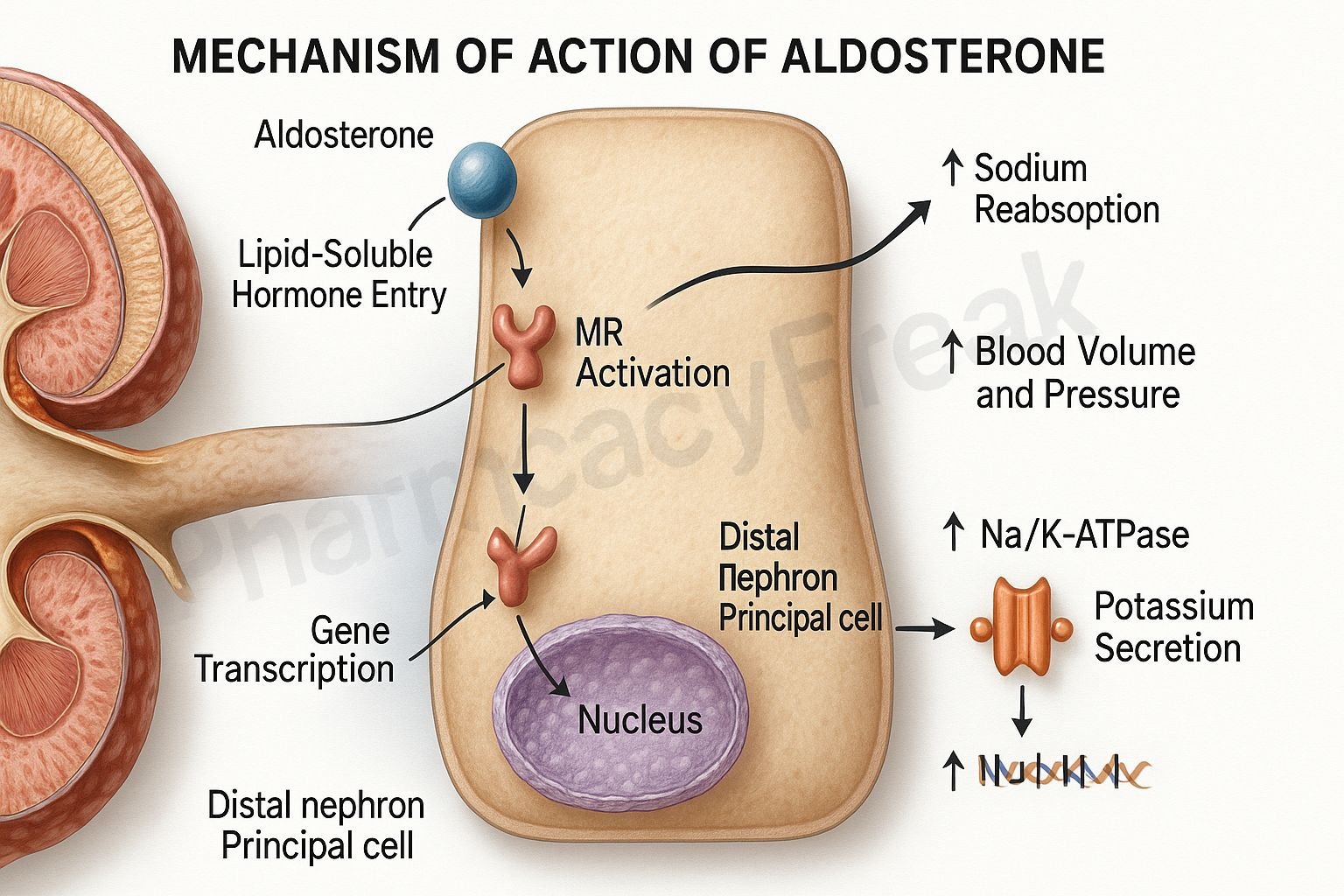
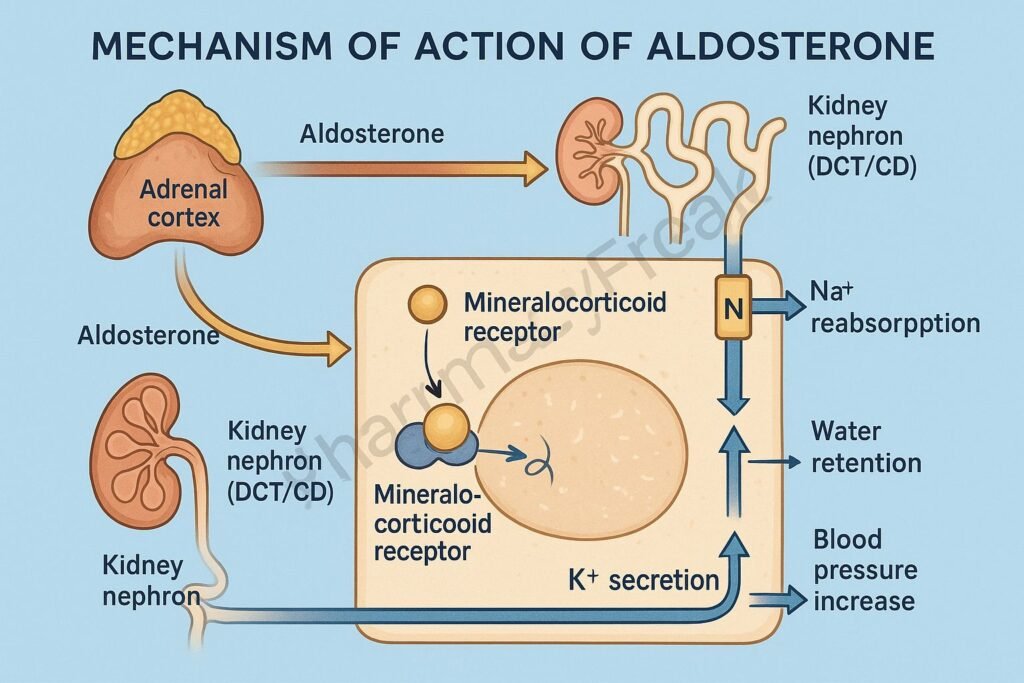
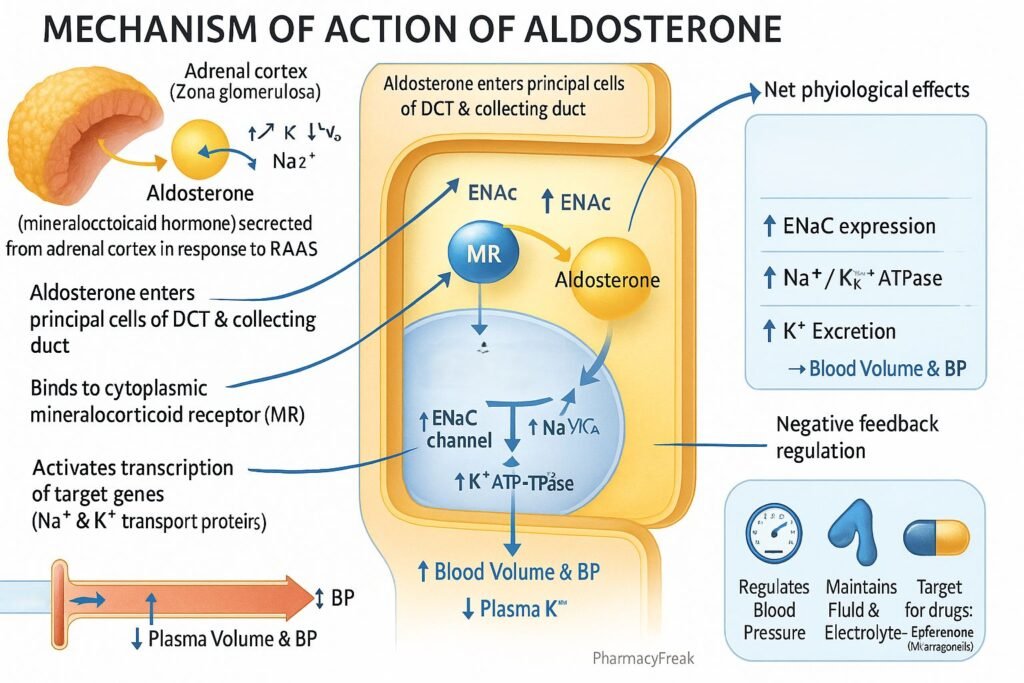
Aldosterone is a mineralocorticoid hormone synthesized in the zona glomerulosa of the adrenal cortex. It plays a vital role in maintaining electrolyte balance, blood volume, and blood pressure through regulation of sodium and potassium homeostasis. Mechanism of Action of Aldosterone involves binding to intracellular mineralocorticoid receptors (MR) in epithelial cells of the distal nephron, leading to increased sodium reabsorption and potassium secretion. Its effects are critical in the renin–angiotensin–aldosterone system (RAAS) and are essential for fluid balance and cardiovascular stability.
Mechanism of Action (Step-wise)
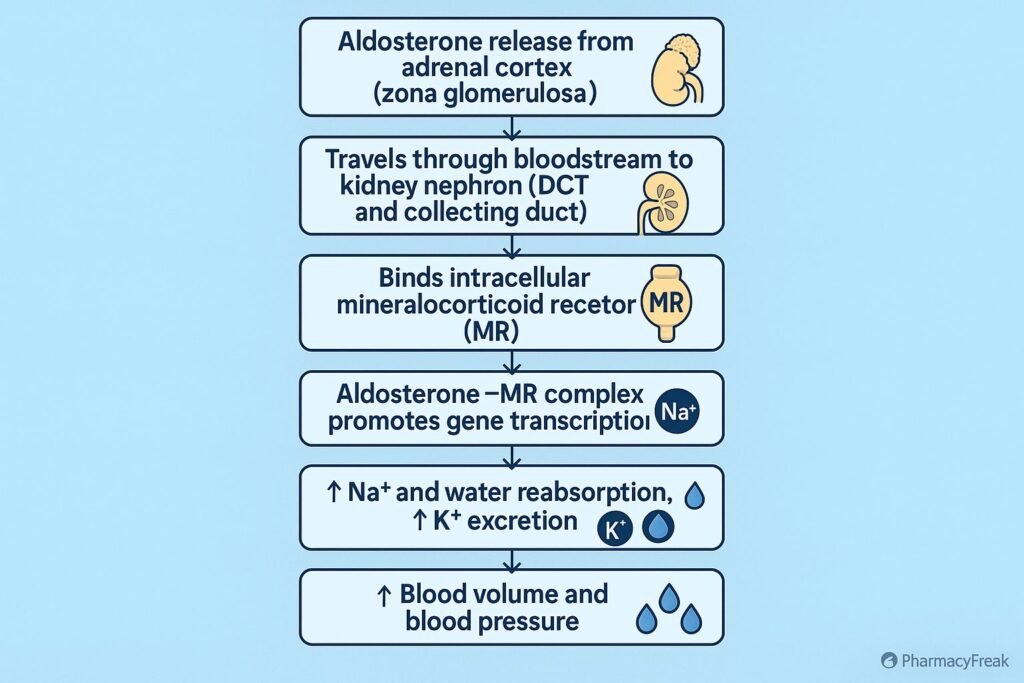
- Hormone Release and Circulation
- Aldosterone secretion is stimulated by angiotensin II, elevated plasma potassium, and adrenocorticotropic hormone (ACTH).
- It travels through the bloodstream bound to plasma proteins such as albumin and corticosteroid-binding globulin.
- Receptor Binding
- In the distal convoluted tubule and collecting duct of the nephron, aldosterone diffuses through the cell membrane and binds to intracellular mineralocorticoid receptors (MR) in the cytoplasm.
- Gene Transcription Activation
- The aldosterone–receptor complex translocates to the nucleus, where it binds to specific DNA response elements.
- This triggers transcription of genes encoding epithelial sodium channels (ENaC) and Na⁺/K⁺-ATPase pumps.
- Protein Synthesis and Cellular Changes
- Newly synthesized ENaC channels are inserted into the luminal membrane.
- Na⁺/K⁺-ATPase pumps are upregulated on the basolateral side of tubular cells.
- Physiological Effects
- Increased sodium reabsorption from tubular fluid into the bloodstream.
- Increased potassium excretion into the urine.
- Water retention secondary to sodium reabsorption, leading to increased extracellular fluid volume and blood pressure.
- Overall Effect
- Conserves sodium and water.
- Promotes potassium excretion.
- Maintains intravascular volume and arterial pressure.
Pharmacokinetics
- Source: Endogenously secreted steroid hormone.
- Half-life: Approximately 15–20 minutes in plasma.
- Metabolism: Rapid hepatic metabolism to tetrahydroaldosterone and conjugates.
- Excretion: Metabolites eliminated via urine.
- Receptor type: Nuclear/cytosolic receptor (acts via gene transcription).
Clinical Importance
- Physiological role: Electrolyte and fluid balance via the RAAS pathway.
- Deficiency: Seen in Addison’s disease (adrenal insufficiency) — results in hyponatremia, hyperkalemia, and hypotension.
- Excess: Seen in primary hyperaldosteronism (Conn’s syndrome) — causes hypertension, hypokalemia, and metabolic alkalosis.
- Therapeutic modulation:
- Agonists: Fludrocortisone (synthetic mineralocorticoid).
- Antagonists: Spironolactone, Eplerenone — used in heart failure, hypertension, and hyperaldosteronism.
Adverse Effects of Excess Aldosterone
- Hypertension due to sodium and water retention.
- Hypokalemia → muscle weakness, arrhythmias.
- Metabolic alkalosis.
- Cardiac remodeling and fibrosis in chronic cases.
Comparative Analysis
| Feature | Aldosterone | Cortisol | Spironolactone (Antagonist) |
|---|---|---|---|
| Source | Zona glomerulosa (adrenal cortex) | Zona fasciculata | Synthetic drug |
| Primary receptor | Mineralocorticoid receptor (MR) | Glucocorticoid receptor (GR) | Mineralocorticoid receptor antagonist |
| Main action | Na⁺ retention, K⁺ excretion | Glucose metabolism, stress response | K⁺ retention, Na⁺ loss |
| Effect on BP | Increases | Mild increase | Decreases |
| Clinical correlation | RAAS control, BP regulation | Stress and metabolism | Treatment of hyperaldosteronism |
MCQs
1. Aldosterone is secreted from which part of the adrenal gland?
a) Zona fasciculata
b) Zona glomerulosa
c) Zona reticularis
d) Medulla
Answer: b) Zona glomerulosa
2. Aldosterone acts on which part of the nephron?
a) Proximal tubule
b) Loop of Henle
c) Distal convoluted tubule and collecting duct
d) Glomerulus
Answer: c) Distal convoluted tubule and collecting duct
3. The main effect of aldosterone is:
a) Sodium excretion and potassium retention
b) Sodium retention and potassium excretion
c) Both sodium and potassium retention
d) Sodium excretion only
Answer: b) Sodium retention and potassium excretion
4. The receptor for aldosterone is located in the:
a) Cell membrane
b) Cytoplasm/nucleus
c) Synaptic cleft
d) Extracellular matrix
Answer: b) Cytoplasm/nucleus
5. Aldosterone increases expression of which transport protein?
a) Na⁺/K⁺-ATPase
b) Ca²⁺ channels
c) H⁺/K⁺-ATPase
d) Glucose transporter
Answer: a) Na⁺/K⁺-ATPase
6. Which of the following stimulates aldosterone secretion?
a) Low potassium
b) High sodium
c) Angiotensin II
d) Low ACTH
Answer: c) Angiotensin II
7. The main mechanism of hypertension in hyperaldosteronism is:
a) Increased cardiac output
b) Increased sodium and water reabsorption
c) Decreased peripheral resistance
d) Increased renin release
Answer: b) Increased sodium and water reabsorption
8. Which drug blocks aldosterone receptors?
a) Spironolactone
b) Furosemide
c) Hydrochlorothiazide
d) Metoprolol
Answer: a) Spironolactone
9. The half-life of aldosterone is approximately:
a) 5 minutes
b) 15–20 minutes
c) 1 hour
d) 12 hours
Answer: b) 15–20 minutes
10. Which condition is associated with aldosterone deficiency?
a) Addison’s disease
b) Cushing’s syndrome
c) Diabetes insipidus
d) Pheochromocytoma
Answer: a) Addison’s disease
FAQs
Q1. How does aldosterone increase blood pressure?
It promotes sodium and water reabsorption, increasing blood volume and consequently blood pressure.
Q2. What stimulates aldosterone secretion?
Mainly angiotensin II, elevated plasma potassium, and to a lesser extent, ACTH.
Q3. How does aldosterone differ from cortisol?
Aldosterone primarily regulates electrolytes, while cortisol regulates metabolism and stress responses.
Q4. What happens in hyperaldosteronism?
Excess aldosterone leads to hypertension, hypokalemia, and metabolic alkalosis.
Q5. What drugs inhibit aldosterone action?
Spironolactone and eplerenone — both are mineralocorticoid receptor antagonists.
Q6. Can aldosterone deficiency cause dehydration?
Yes, due to excessive sodium and water loss in urine.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung’s Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- Guyton & Hall Textbook of Medical Physiology
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com