Table of Contents
Introduction
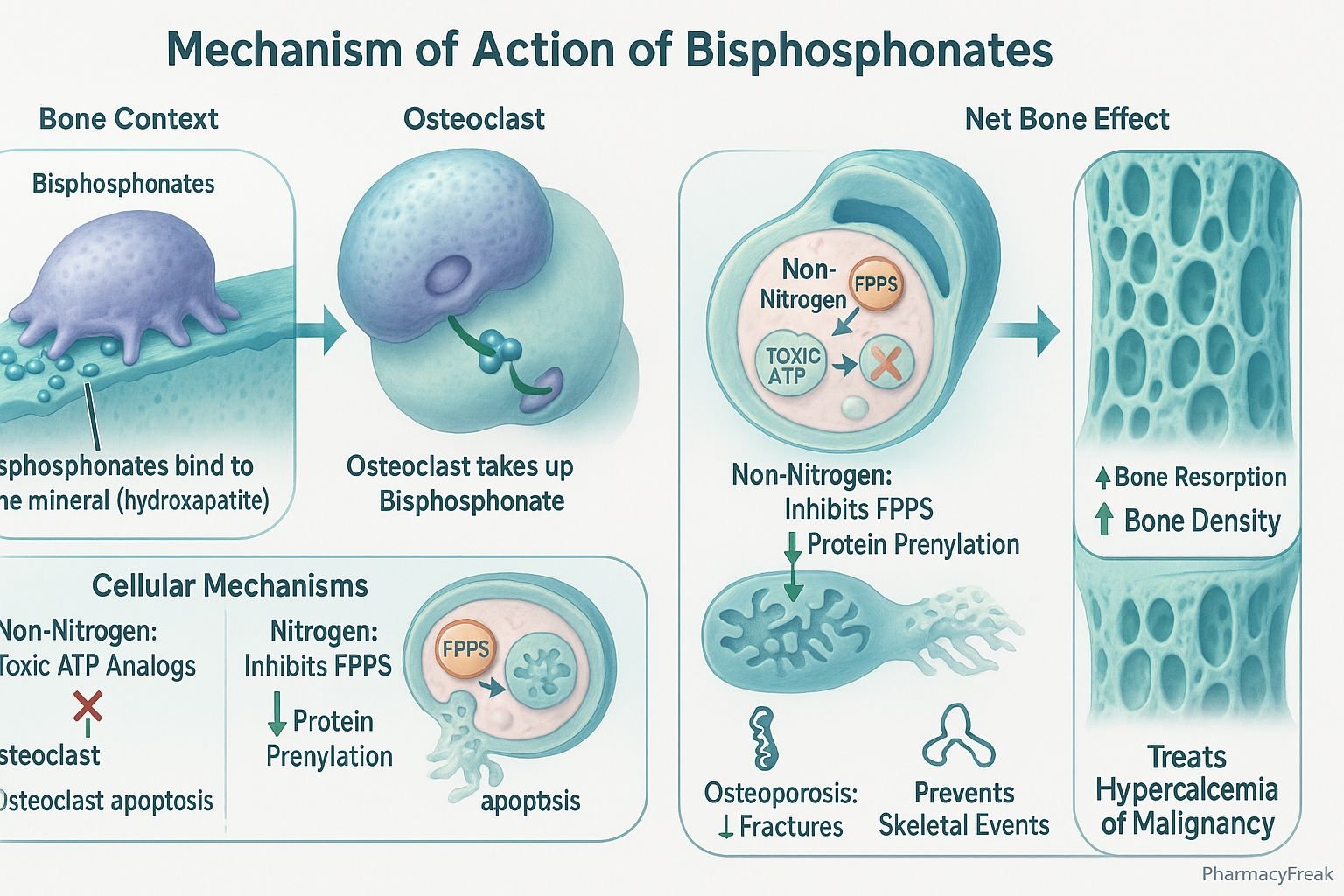
Bisphosphonates are a major class of drugs used to prevent and treat bone resorption disorders. Mechanism of Action of Bisphosphonates revolves around their ability to inhibit osteoclast-mediated bone breakdown, thereby preserving bone density. They are widely used in conditions such as osteoporosis, Paget’s disease of bone, multiple myeloma, and bone metastases. Their unique affinity for bone tissue makes them highly effective in targeting skeletal pathology.
Mechanism of Action (Step-wise)
- Bone Affinity
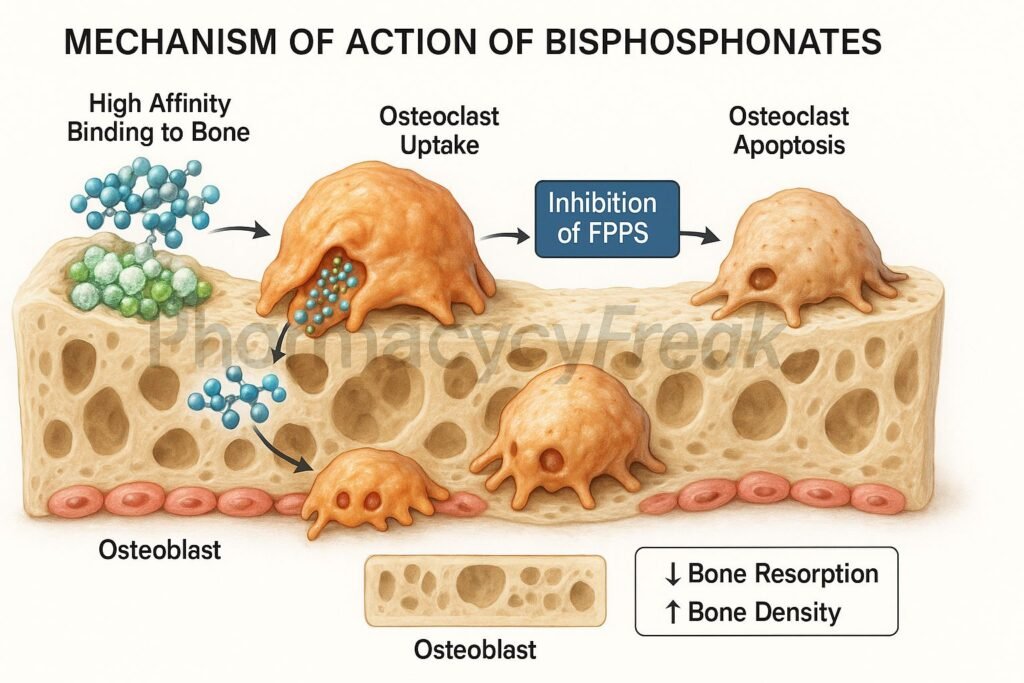
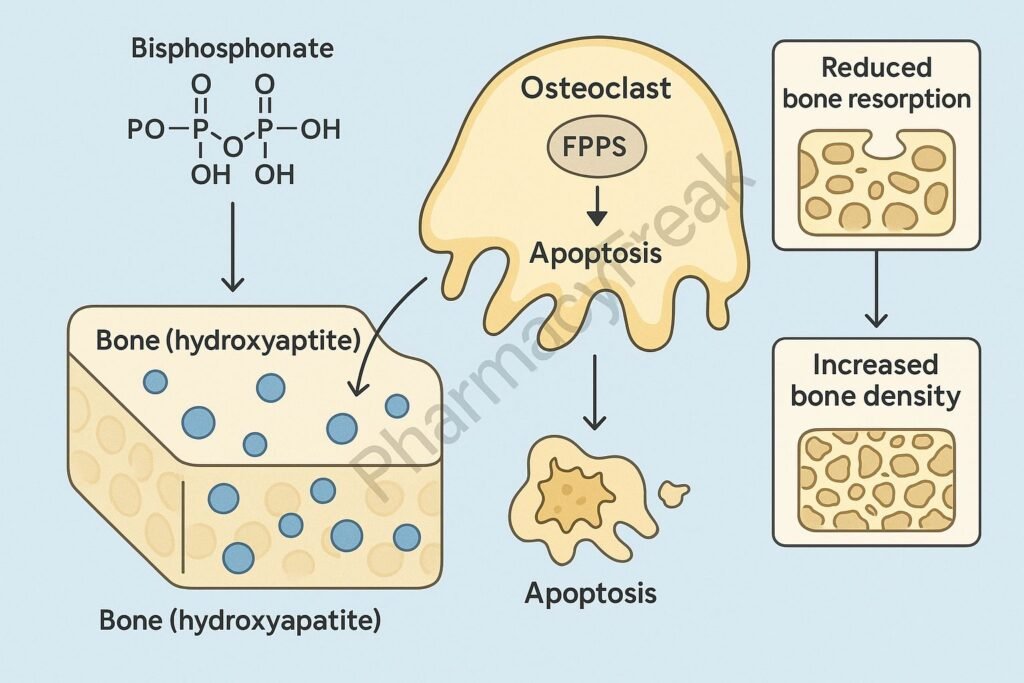
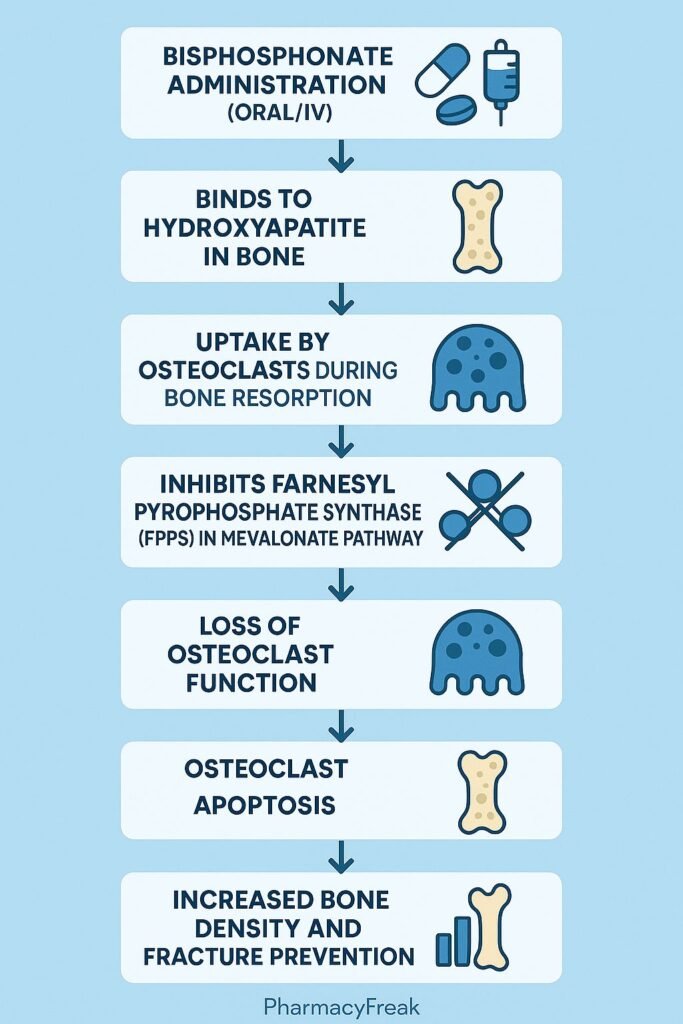
- Bisphosphonates have a strong affinity for hydroxyapatite crystals in bone.
- They bind selectively to sites of active bone resorption.
- Osteoclast Uptake
- During bone remodeling, osteoclasts ingest bisphosphonates from resorption surfaces.
- This delivers the drug directly to the cells responsible for bone breakdown.
- Intracellular Action
- Non-nitrogen bisphosphonates (e.g., etidronate): Incorporate into ATP analogs, causing osteoclast apoptosis.
- Nitrogen-containing bisphosphonates (e.g., alendronate, zoledronic acid): Inhibit farnesyl pyrophosphate synthase (FPPS) in the mevalonate pathway.
- This prevents prenylation of GTP-binding proteins necessary for osteoclast function.
- Inhibition of Osteoclast Function
- Osteoclasts lose the ability to form ruffled borders, adhere to bone, and resorb mineralized tissue.
- Apoptosis of osteoclasts is induced.
- Overall Effect
- Decreased bone resorption.
- Increased bone mineral density and skeletal strength.
Pharmacokinetics
- Absorption: Poor oral absorption (<1% bioavailability); must be taken fasting with water.
- Distribution: Rapidly binds to bone; minimal plasma protein binding.
- Metabolism: Not metabolized.
- Excretion: Excreted unchanged via the kidneys.
- Half-life: Very long skeletal half-life (years), due to deposition in bone.
Clinical Uses
- Osteoporosis (postmenopausal, male, and glucocorticoid-induced).
- Paget’s disease of bone.
- Bone metastases and hypercalcemia of malignancy.
- Multiple myeloma-related bone lesions.
- Osteogenesis imperfecta (off-label).
Adverse Effects
- Common: Gastrointestinal irritation, esophagitis (oral forms).
- Less common: Hypocalcemia, flu-like symptoms (IV administration).
- Serious: Osteonecrosis of the jaw (ONJ), atypical femoral fractures, renal toxicity (IV high dose).
Comparative Analysis
| Feature | Nitrogen Bisphosphonates (e.g., Alendronate) | Non-Nitrogen Bisphosphonates (e.g., Etidronate) |
|---|---|---|
| Main target | FPPS in mevalonate pathway | ATP analog formation |
| Potency | Higher | Lower |
| Apoptosis induction | Via disrupted protein prenylation | Via toxic ATP analogs |
| Clinical use | Osteoporosis, cancer-related bone disease | Rarely used today |
| Half-life in bone | Long | Long |
MCQs
1. What is the main action of bisphosphonates?
a) Stimulating osteoblasts
b) Inhibiting osteoclast-mediated bone resorption
c) Increasing vitamin D activation
d) Increasing calcium absorption from intestine
Answer: b) Inhibiting osteoclast-mediated bone resorption
2. Nitrogen-containing bisphosphonates inhibit which enzyme?
a) Cyclooxygenase
b) Farnesyl pyrophosphate synthase
c) Carbonic anhydrase
d) Na+/K+ ATPase
Answer: b) Farnesyl pyrophosphate synthase
3. Which condition is a serious complication of bisphosphonate therapy?
a) Osteonecrosis of the jaw
b) Glaucoma
c) Hypertension
d) Hepatotoxicity
Answer: a) Osteonecrosis of the jaw
4. Which bisphosphonate has the highest potency?
a) Etidronate
b) Zoledronic acid
c) Tiludronate
d) Clodronate
Answer: b) Zoledronic acid
5. Bisphosphonates are contraindicated in:
a) Hypertension
b) Renal impairment
c) Osteoporosis
d) Paget’s disease
Answer: b) Renal impairment
6. Which bisphosphonate is given intravenously?
a) Risedronate
b) Zoledronic acid
c) Alendronate
d) Tiludronate
Answer: b) Zoledronic acid
7. Oral bisphosphonates should be taken:
a) With meals
b) With milk
c) On an empty stomach with water
d) With fruit juice
Answer: c) On an empty stomach with water
8. How long is the skeletal half-life of bisphosphonates?
a) Hours
b) Days
c) Weeks
d) Years
Answer: d) Years
9. The ruffled border in osteoclasts is disrupted by:
a) Bisphosphonates
b) Calcitonin
c) Denosumab
d) Teriparatide
Answer: a) Bisphosphonates
10. Bisphosphonates belong to which pharmacological group?
a) Anti-resorptive drugs
b) Anabolic bone drugs
c) Anti-inflammatory drugs
d) Calcium-sensing receptor agonists
Answer: a) Anti-resorptive drugs
FAQs
Q1. How do bisphosphonates prevent bone loss?
By binding to bone and inhibiting osteoclast-mediated resorption.
Q2. Do bisphosphonates increase calcium absorption?
No, they primarily reduce bone resorption, indirectly stabilizing calcium levels.
Q3. How should oral bisphosphonates be taken?
On an empty stomach with water, sitting upright for at least 30 minutes.
Q4. Can bisphosphonates be used long-term?
Yes, but drug holidays are often recommended after 3–5 years to reduce risks.
Q5. What is the difference between nitrogen and non-nitrogen bisphosphonates?
Nitrogen-containing drugs inhibit the mevalonate pathway, while non-nitrogen types form toxic ATP analogs.
Q6. What rare side effect is associated with IV bisphosphonates?
Osteonecrosis of the jaw, especially after dental surgery.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics
- Katzung Basic and Clinical Pharmacology
- Harrison’s Principles of Internal Medicine
- Clinical practice guidelines on osteoporosis management
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com