Table of Contents
Introduction
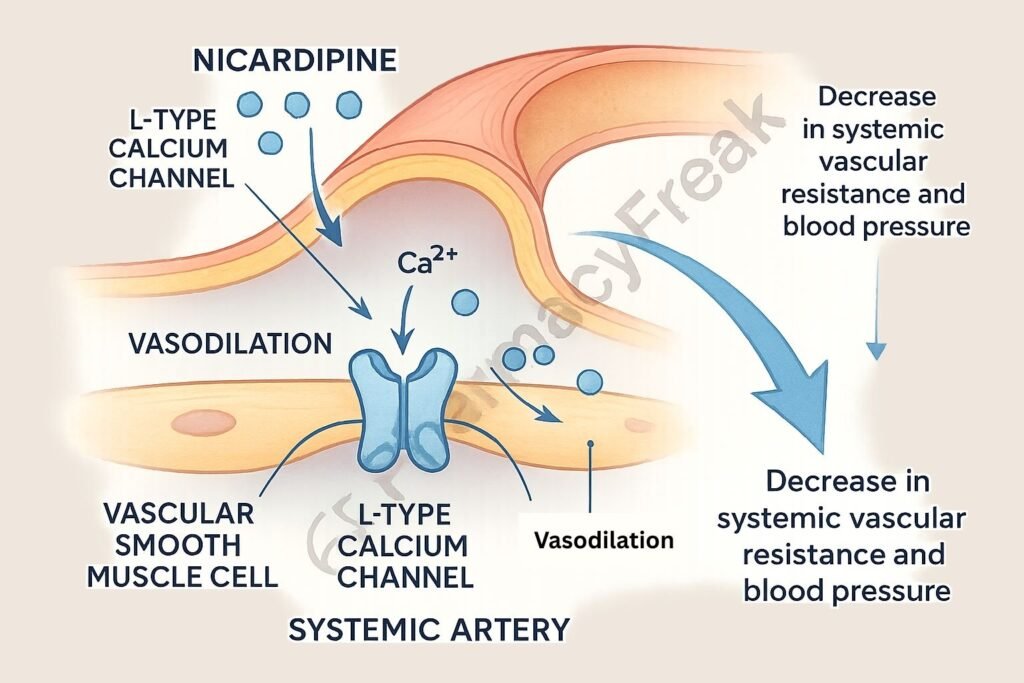
Nicardipine is a dihydropyridine calcium channel blocker primarily used for the management of hypertension and angina. It selectively acts on vascular smooth muscle to induce vasodilation, resulting in decreased systemic vascular resistance. Its rapid onset and favorable hemodynamic profile make it especially useful in hypertensive emergencies and perioperative blood pressure control.
Mechanism of Action (Step-wise)
1. Inhibition of L-type Calcium Channels
Nicardipine selectively blocks L-type voltage-gated calcium channels located in the smooth muscle of arterial vessels.
2. Decreased Calcium Influx
Blocking these channels reduces intracellular calcium concentration, which is essential for vascular smooth muscle contraction.
3. Vascular Smooth Muscle Relaxation
Reduced calcium availability leads to relaxation of arteriolar smooth muscle, causing vasodilation.
4. Decreased Systemic Vascular Resistance (SVR)
Vasodilation lowers SVR and arterial blood pressure.
5. Coronary Artery Dilation
Nicardipine also dilates coronary arteries, enhancing myocardial oxygen supply, beneficial in angina.
Pharmacokinetics
- Route of Administration: Oral and intravenous
- Bioavailability (oral): ~35% (due to first-pass metabolism)
- Onset of Action: 5–15 minutes (IV), 45 minutes (oral)
- Half-Life: 2–4 hours (IV), up to 8 hours (oral)
- Metabolism: Hepatic (CYP3A4)
- Excretion: Urine and feces
Clinical Uses
- Hypertensive emergencies (IV form)
- Chronic hypertension (oral form)
- Angina pectoris
- Perioperative blood pressure control
- Subarachnoid hemorrhage-associated vasospasm (off-label)
Adverse Effects
- Headache
- Flushing
- Tachycardia (reflex)
- Peripheral edema
- Hypotension
- Nausea and dizziness
- Contraindications: Aortic stenosis, advanced heart block (without pacemaker), severe hypotension
Comparative Analysis
| Parameter | Nicardipine | Amlodipine |
|---|---|---|
| Drug Class | Dihydropyridine CCB | Dihydropyridine CCB |
| Onset of Action (IV) | Rapid (5–15 min) | Not used IV |
| Duration of Action | Short (IV), moderate (oral) | Long (oral, ~24–36 hours) |
| Tachycardia | Common | Less common |
| Indications | Hypertensive emergency, angina | Chronic hypertension |
Multiple Choice Questions (MCQs)
1. Nicardipine primarily blocks which type of calcium channel?
a) N-type
b) L-type
c) P/Q-type
d) T-type
Answer: b) L-type
2. The therapeutic effect of nicardipine is mainly due to:
a) Increased cardiac output
b) Vasodilation of arteries
c) Increased preload
d) Decreased myocardial contractility
Answer: b) Vasodilation of arteries
3. A common reflex side effect of nicardipine is:
a) Bradycardia
b) Constipation
c) Tachycardia
d) Dry mouth
Answer: c) Tachycardia
4. Nicardipine is contraindicated in which condition?
a) Angina pectoris
b) Hypertensive crisis
c) Severe aortic stenosis
d) Diabetes mellitus
Answer: c) Severe aortic stenosis
5. What is the onset of action for IV nicardipine?
a) 1 hour
b) 30 minutes
c) 5–15 minutes
d) Immediate
Answer: c) 5–15 minutes
FAQs
Q1. Can nicardipine be used in pregnancy?
It is generally avoided unless the benefit outweighs the risk.
Q2. How is nicardipine administered during hypertensive emergencies?
It is given as a continuous intravenous infusion.
Q3. Does nicardipine cause bradycardia?
No, reflex tachycardia is more common due to vasodilation.
Q4. Is nicardipine used for arrhythmias?
No, it has no significant effects on cardiac conduction.
Q5. How does nicardipine differ from verapamil?
Nicardipine is a vascular-selective dihydropyridine, while verapamil affects the heart more directly.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 12th Edition
- KD Tripathi, Essentials of Medical Pharmacology, 7th Edition
- Nicardipine Prescribing Information
- Guidelines for Hypertensive Emergencies
Related Internal Links

I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com