Table of Contents
Introduction
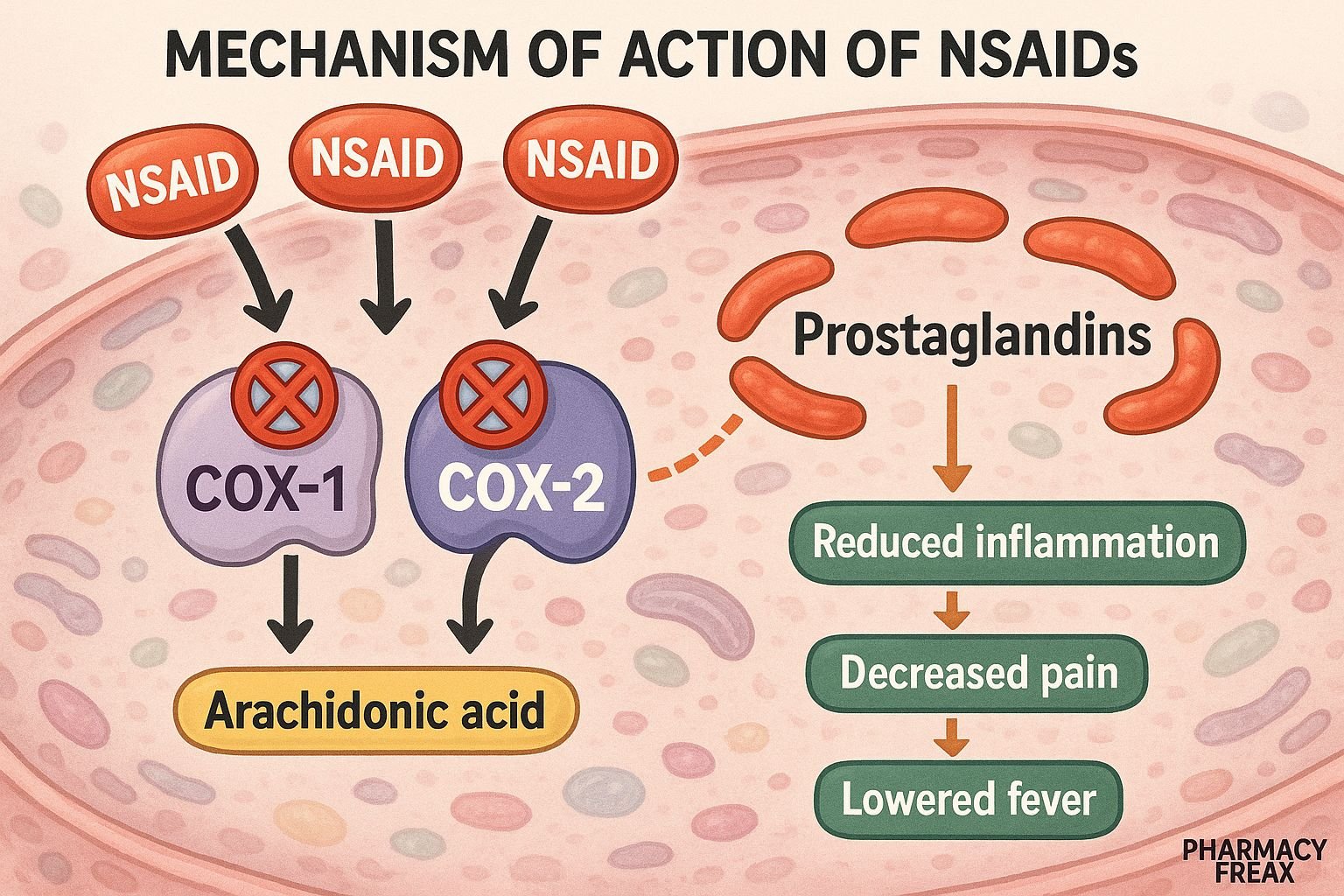
Non-steroidal anti-inflammatory drugs (NSAIDs) are a widely used class of medications with analgesic, anti-inflammatory, and antipyretic properties. They are commonly prescribed for pain relief, reducing inflammation in conditions like arthritis, dysmenorrhea, and fevers. NSAIDs achieve these effects by inhibiting cyclooxygenase enzymes involved in prostaglandin synthesis.
Step‑by‑Step Mechanism of Action
- Inhibition of Cyclooxygenase Enzymes (COX‑1 and COX‑2)
NSAIDs bind reversibly to COX enzymes, blocking the conversion of arachidonic acid to prostaglandin H₂, the precursor for PGE₂, PGI₂, and TXA₂. - Reduction in Prostaglandin Levels
Lower PGE₂ and PGI₂ levels in peripheral tissues result in decreased inflammation, pain, and vasodilation. Decreased hypothalamic PGE₂ lowers fever. - Antiplatelet Effect via TXA₂ Suppression
Specific NSAIDs, like aspirin (irreversibly inhibits COX‑1), reduce TXA₂ production in platelets, inhibiting aggregation and prolonging bleeding time. - Gastrointestinal & Renal Effects
COX‑1 inhibition decreases protective prostaglandins in gastric mucosa (PGE₂, PGI₂), increasing ulcer risk. COX‑mediated prostaglandins in renal afferent arterioles maintain perfusion; inhibition may cause renal dysfunction. - Selectivity Impacts Effects and Safety
- Non-selective NSAIDs (ibuprofen, naproxen) inhibit both COX‑1 and COX‑2.
- Selective COX‑2 inhibitors (e.g., celecoxib) spare COX‑1, reducing GI side effects while retaining anti-inflammatory effects.
Pharmacokinetic Parameters
| Parameter | Ibuprofen (Representative NSAID) |
|---|---|
| Bioavailability | ~80–100% (oral) |
| Peak plasma | 1–2 hours after ingestion |
| Volume of distribution | ~0.1–0.2 L/kg |
| Metabolism | Hepatic (via CYP2C9) |
| Elimination | Renal excretion of metabolites |
| Half-life | 2–3 hours (longer for naproxen/celecoxib) |
| Protein binding | ~99% |
Clinical Uses
- Pain relief: headache, musculoskeletal pain
- Inflammation: osteoarthritis, rheumatoid arthritis
- Fever reduction
- Dysmenorrhea
- Prevention of cardiovascular events (low‑dose aspirin)
- Post-operative pain management
Adverse Effects
- Gastrointestinal: dyspepsia, ulcers, bleeding
- Renal: reduced perfusion, sodium retention, hyperkalemia
- Cardiovascular: fluid retention, hypertension, increased CV risk (esp. COX‑2 inhibitors and high-dose NSAIDs)
- Hypersensitivity: asthma exacerbation, urticaria
- Hematologic: bleeding due to platelet inhibition
- Rare: hepatotoxicity, aseptic meningitis
Comparative Analysis
| NSAID | COX Selectivity | GI Risk | CV Risk | Platelet Effect |
|---|---|---|---|---|
| Aspirin (low-dose) | Irreversible COX‑1 > COX‑2 | Moderate | Low (cardioprotective) | High |
| Ibuprofen | Non-selective | Moderate | Moderate | Mild |
| Naproxen | Non-selective | Higher | Lower | Moderate |
| Celecoxib | COX‑2 selective | Low | Increased (long-term) | None |
MCQs
1. NSAIDs reduce inflammation primarily by inhibiting:
a) 5-lipoxygenase
b) COX‑1 and COX‑2
c) Phospholipase A₂
d) Thromboxane synthase
Answer: b) COX‑1 and COX‑2
2. Low-dose aspirin has cardioprotective effects because it:
a) Inhibits COX‑2 in vascular endothelium
b) Irreversibly inhibits COX‑1 in platelets
c) Inhibits phospholipase C
d) Increases prostacyclin levels
Answer: b) Irreversibly inhibits COX‑1 in platelets
3. A major GI side effect of NSAIDs is due to:
a) Increased gastrin secretion
b) Reduced PGE₂ and PGI₂
c) Increased acid secretion
d) Platelet inhibition
Answer: b) Reduced PGE₂ and PGI₂
4. COX‑2 selective inhibitors are associated with:
a) High GI ulcer risk
b) Reduced CV risk
c) No antipyretic effect
d) Increased cardiovascular risk
Answer: d) Increased cardiovascular risk
5. Which NSAID has the longest half-life?
a) Ibuprofen
b) Celecoxib
c) Aspirin
d) Acetaminophen (not NSAID)
Answer: b) Celecoxib
6. Which of the following NSAIDs irreversibly inhibits COX enzymes?
a) Ibuprofen
b) Naproxen
c) Aspirin
d) Diclofenac
Answer: c) Aspirin
7. What is a common renal effect of chronic NSAID use?
a) Hyperglycemia
b) Increased renal perfusion
c) Sodium retention
d) Diuresis
Answer: c) Sodium retention
8. In which condition is NSAID use relatively contraindicated?
a) Osteoarthritis
b) Asthma
c) Gout
d) Migraine
Answer: b) Asthma
9. Prostaglandins affected by NSAIDs perform all EXCEPT:
a) Maintaining gastric mucosal integrity
b) Promoting renal blood flow
c) Enhancing platelet aggregation
d) Mediating fever
Answer: c) Enhancing platelet aggregation
10. Which enzyme do NSAIDs primarily block to exert antipyretic action?
a) COX‑2 in hypothalamus
b) COX‑1 in liver
c) Phospholipase A₂
d) Cyclin-dependent kinase
Answer: a) COX‑2 in hypothalamus
11. Which NSAID is preferred in patients with cardiovascular disease risk?
a) Celecoxib
b) Etoricoxib
c) Naproxen
d) Indomethacin
Answer: c) Naproxen
12. NSAID-induced bronchospasm is due to increased:
a) Histamine
b) Thromboxane
c) Leukotrienes
d) Acetylcholine
Answer: c) Leukotrienes
13. Why is co-prescription of PPIs common with NSAIDs?
a) Enhance drug absorption
b) Prevent renal toxicity
c) Reduce risk of GI ulceration
d) Increase antipyretic effect
Answer: c) Reduce risk of GI ulceration
14. Which of the following is NOT an effect of prostaglandins?
a) Vasodilation
b) Bronchoconstriction
c) Cytoprotection in GIT
d) Mydriasis
Answer: d) Mydriasis
15. Which statement is true about acetaminophen?
a) It inhibits COX irreversibly
b) It is anti-inflammatory like NSAIDs
c) It lacks anti-inflammatory activity
d) It causes platelet inhibition
Answer: c) It lacks anti-inflammatory activity
FAQs
1. Are NSAIDs safe during pregnancy?
Use with caution, especially in the third trimester; avoid due to risk of premature closure of ductus arteriosus.
2. Can NSAIDs be taken together with proton pump inhibitors?
Yes—co-prescription with PPIs reduces gastrointestinal side effects.
3. Do NSAIDs affect kidney function?
Yes—especially in volume-depleted patients or those with existing renal disease.
4. Can NSAIDs interfere with antihypertensive medications?
Yes—they can blunt the effects of ACE inhibitors, diuretics, and β-blockers.
5. What should be monitored during long-term NSAID therapy?
Renal function, BP, hemoglobin, and signs of GI bleeding.
References
- Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 13th Edition.
- KD Tripathi. Essentials of Medical Pharmacology, 8th Edition.
- Nonsteroidal Anti‑Inflammatory Drugs (NSAIDs) – StatPearls review pubmed.ncbi.nlm.nih.gov+3pubmed.ncbi.nlm.nih.gov+3pubmed.ncbi.nlm.nih.gov+3
- Clinical pharmacology of non‑steroidal anti‑inflammatory drugs pubmed.ncbi.nlm.nih.gov
- COX‑2 inhibitors and cardiovascular risk – PubMed review pubmed.ncbi.nlm.nih.gov+15pubmed.ncbi.nlm.nih.gov+15pubmed.ncbi.nlm.nih.gov+15
I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com