Table of Contents
Introduction
Macrolides are a widely used class of bacteriostatic antibiotics that inhibit bacterial protein synthesis. They are especially effective against Gram-positive cocci, atypical organisms, and some Gram-negative pathogens. Common macrolides include erythromycin, azithromycin, and clarithromycin. Their use extends to respiratory tract infections, STDs, and skin infections, with azithromycin being a favorite due to its long half-life and once-daily dosing.
Macrolides are frequently asked in USMLE, NCLEX, GPAT, and NEET-PG due to their mechanism, resistance, and adverse effect profile.
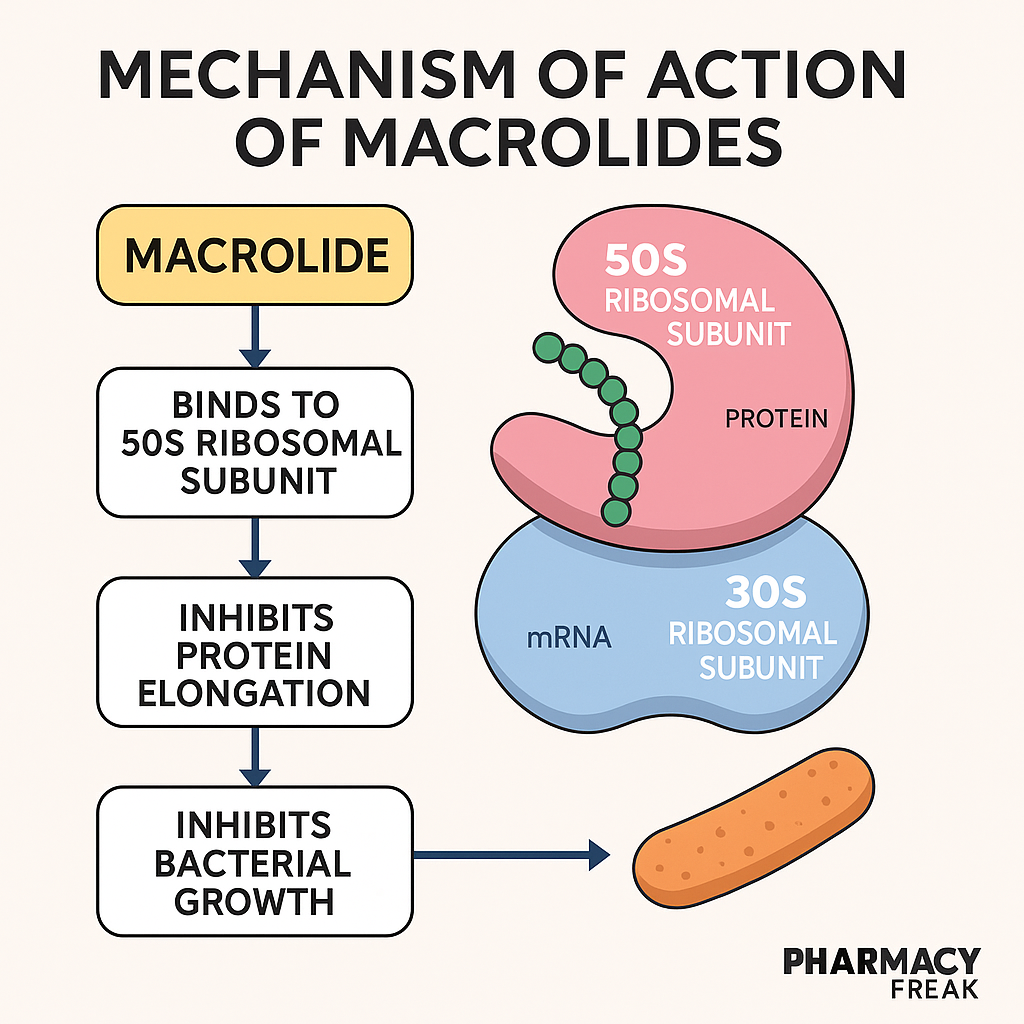
Stepwise Mechanism of Action of Macrolides
- Target: 50S ribosomal subunit
Macrolides bind to the 23S rRNA of the 50S subunit of bacterial ribosomes. - Inhibition of translocation
This binding blocks the translocation step of protein elongation, preventing the transfer of peptidyl-tRNA from the A to P site. - Inhibition of bacterial protein synthesis
As a result, bacterial protein production is halted, leading to growth arrest. Hence, macrolides are primarily bacteriostatic, though they may be bactericidal at high doses. - Effect on intracellular organisms
Macrolides accumulate within phagocytes, enabling targeting of intracellular pathogens like Mycoplasma, Chlamydia, and Legionella.
Pharmacokinetic Parameters of Macrolides
| Parameter | Azithromycin Example |
|---|---|
| Bioavailability | ~37% (azithromycin) |
| Half-life | ~68 hours (azithromycin) |
| Protein binding | ~50% (varies) |
| Metabolism | Hepatic (CYP3A4 pathway) |
| Excretion | Biliary (mostly), renal (minor) |
| Therapeutic range | Not routinely monitored |
Clinical Uses of Macrolides
- Community-acquired pneumonia (CAP)
- Atypical pneumonia (Mycoplasma, Chlamydia, Legionella)
- Pharyngitis, sinusitis, otitis media
- Pertussis (whooping cough)
- STDs (chlamydia, nongonococcal urethritis)
- H. pylori infections (clarithromycin as part of triple therapy)
- Prophylaxis in HIV (MAC infection)
Adverse Effects of Macrolides
- Gastrointestinal upset – diarrhea, nausea (especially erythromycin)
- QT prolongation and risk of torsades de pointes
- Cholestatic hepatitis (rare)
- Ototoxicity (with high doses)
- Drug interactions – especially erythromycin and clarithromycin (CYP3A4 inhibitors)
- Metallic taste (clarithromycin)
Comparative Analysis: Erythromycin vs Azithromycin
| Feature | Erythromycin | Azithromycin |
|---|---|---|
| Dosing frequency | Multiple times/day | Once daily |
| GI side effects | Common | Rare |
| QT prolongation risk | High | Moderate |
| Drug interactions | Significant (CYP3A4 inhibitor) | Minimal |
| Intracellular activity | Moderate | Excellent |
Practice MCQs
Q1. Macrolides inhibit which ribosomal subunit?
a. 30S
b. 40S
c. 50S ✅
d. 60S
Q2. The primary mechanism of macrolides is:
a. DNA polymerase inhibition
b. Peptidoglycan synthesis inhibition
c. Protein synthesis inhibition ✅
d. RNA synthesis inhibition
Q3. Which step is blocked by macrolides?
a. tRNA charging
b. Translocation ✅
c. Peptide bond formation
d. Ribosome assembly
Q4. Which organism is best treated with azithromycin?
a. E. coli
b. Mycoplasma pneumoniae ✅
c. MRSA
d. Mycobacterium tuberculosis
Q5. Major adverse effect of erythromycin is:
a. Renal toxicity
b. Hepatotoxicity
c. GI intolerance ✅
d. Seizures
Q6. Which macrolide has the longest half-life?
a. Erythromycin
b. Clarithromycin
c. Azithromycin ✅
d. Roxithromycin
Q7. Macrolides can cause QT prolongation due to:
a. Na⁺ channel blockade
b. Ca²⁺ channel inhibition
c. K⁺ channel blockade ✅
d. Increased heart rate
Q8. Clarithromycin is part of triple therapy for:
a. Pneumonia
b. H. pylori infection ✅
c. Malaria
d. Typhoid
Q9. Which macrolide is safest in hepatic patients?
a. Erythromycin
b. Azithromycin ✅
c. Clarithromycin
d. Roxithromycin
Q10. Macrolides are ineffective against:
a. Legionella
b. MRSA ✅
c. Mycoplasma
d. Chlamydia
FAQs
Q1: Are macrolides safe in pregnancy?
Yes, azithromycin and erythromycin are considered safe in pregnancy.
Q2: Why is azithromycin preferred over erythromycin?
Azithromycin has better GI tolerance, fewer drug interactions, and once-daily dosing.
Q3: Can macrolides be used in penicillin-allergic patients?
Yes, they are often the drug of choice for respiratory infections in penicillin-allergic individuals.
Q4: Which macrolide inhibits CYP3A4 significantly?
Erythromycin and clarithromycin — leading to potential drug interactions.
Q5: Is macrolide activity time- or concentration-dependent?
Macrolides exhibit time-dependent killing with post-antibiotic effect.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK539768/
I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com