Table of Contents
Introduction
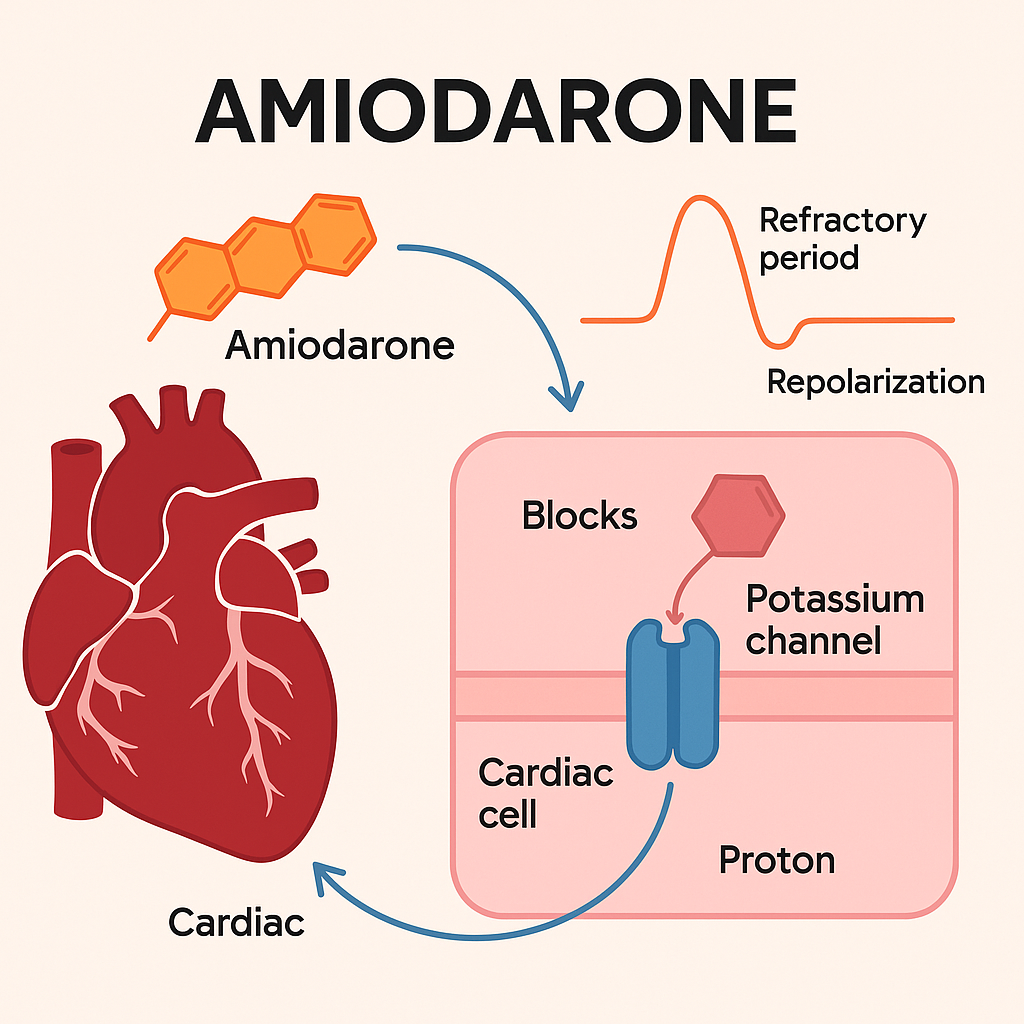
Amiodarone is a powerful Class III antiarrhythmic agent used to treat various life-threatening cardiac arrhythmias, including ventricular tachycardia, ventricular fibrillation, and atrial fibrillation. It has a complex pharmacology, affecting multiple phases of the cardiac action potential and multiple ion channels.
Due to its broad antiarrhythmic profile, multi-organ toxicity, and exam relevance, amiodarone is a high-yield drug for students preparing for USMLE, NCLEX, NAPLEX, GPAT, and NEET-PG.
Mechanism of Action of Amiodarone: Step-by-Step
- Class III primary action – K⁺ channel blockade
Amiodarone prolongs phase 3 repolarization of the cardiac action potential by blocking potassium channels, increasing the action potential duration and refractory period. - Class I action – Na⁺ channel blockade
Inhibits fast inward sodium channels (Class I effect), reducing the rate of depolarization (phase 0). - Class II action – β-adrenergic receptor blockade
Exerts non-competitive beta-blocking effects, reducing sympathetic activity on the heart (Class II effect). - Class IV action – Ca²⁺ channel blockade
Weakly inhibits L-type calcium channels, slowing conduction through the AV node (Class IV effect). - Result: Broad antiarrhythmic profile
The net result is slowed conduction, prolonged refractoriness, and suppressed abnormal automaticity, making it effective in both supraventricular and ventricular arrhythmias.
Pharmacokinetic Parameters of Amiodarone
| Parameter | Value |
|---|---|
| Bioavailability | 35–65% |
| Half-life | 25–60 days (!), very long |
| Protein binding | ~95% |
| Metabolism | Hepatic (CYP3A4) |
| Excretion | Primarily biliary (feces) |
| Time to onset | Delayed (up to weeks for oral form) |
Clinical Uses of Amiodarone
- Ventricular tachycardia (VT)
- Ventricular fibrillation (VF)
- Atrial fibrillation (AF) (especially with structural heart disease)
- Supraventricular tachycardia (SVT)
- Wolff–Parkinson–White (WPW) syndrome
Adverse Effects of Amiodarone (Cumulative & Multi-system)
- Pulmonary fibrosis
- Hepatotoxicity
- Thyroid dysfunction (hypo- or hyperthyroidism due to iodine content)
- Corneal microdeposits
- Photosensitivity and blue-grey skin discoloration
- Bradycardia and heart block
- QT prolongation (risk of torsades is low but present)
- Neuropathy and tremor
Comparative Analysis: Amiodarone vs Sotalol (Both Class III)
| Feature | Amiodarone | Sotalol |
|---|---|---|
| Class III mechanism | K⁺ channel blockade | K⁺ channel blockade |
| Additional effects | Class I, II, IV actions | β-blocker only |
| Half-life | Extremely long (weeks) | Shorter (12–20 hrs) |
| Use in HF/MI | Preferred | Caution due to β-blockade |
| Risk of torsades | Lower (despite QT prolongation) | Higher |
| Organ toxicities | Pulmonary, liver, thyroid | Less common |
Practice MCQs
Q1. What is the primary mechanism of amiodarone?
a. Na⁺ channel blockade
b. K⁺ channel blockade ✅
c. Ca²⁺ channel blockade
d. β-receptor agonism
Q2. Amiodarone has the following class effects EXCEPT:
a. Class I
b. Class II
c. Class III
d. Class V ✅
Q3. Which organ system is commonly affected by chronic amiodarone use?
a. Kidneys
b. Lungs ✅
c. Pancreas
d. Spleen
Q4. Amiodarone causes hypo- or hyperthyroidism due to:
a. Potassium loss
b. Iodine content ✅
c. Liver enzyme induction
d. Sodium retention
Q5. The elimination of amiodarone is primarily through:
a. Renal
b. Pulmonary
c. Fecal (biliary excretion) ✅
d. Salivary
Q6. Which is NOT a side effect of amiodarone?
a. Pulmonary fibrosis
b. Hepatotoxicity
c. Myelosuppression ✅
d. Photosensitivity
Q7. The long half-life of amiodarone can lead to:
a. Acute toxicity
b. Cumulative toxicity ✅
c. Rapid onset of effect
d. Diuretic action
Q8. Amiodarone is effective in all EXCEPT:
a. Atrial fibrillation
b. Ventricular fibrillation
c. Bradyarrhythmias ✅
d. Supraventricular tachycardias
Q9. Which test is important before and during amiodarone therapy?
a. Serum calcium
b. TSH and liver function ✅
c. Urinalysis
d. INR
Q10. Why is amiodarone preferred in heart failure patients?
a. Positive inotrope
b. No proarrhythmic risk
c. Safe beta-blockade
d. Minimal negative inotropy ✅
FAQs
Q1: Is amiodarone safe in pregnancy?
No. It is generally avoided due to risks of fetal hypothyroidism and bradycardia.
Q2: Can amiodarone be used long-term?
Yes, but only with regular monitoring due to long-term toxicity.
Q3: What labs are needed during treatment?
TSH, liver enzymes, pulmonary function, eye exams, and ECG monitoring.
Q4: Does it interact with other drugs?
Yes. It inhibits CYP3A4 and P-gp, increasing levels of warfarin, digoxin, statins, etc.
Q5: How fast does it work?
IV onset is rapid, but oral onset is delayed, requiring loading doses.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK459338/
I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com