Table of Contents
Introduction
Benzodiazepines are a class of psychoactive drugs widely used for their anxiolytic, sedative, hypnotic, anticonvulsant, and muscle relaxant effects. They are commonly prescribed in conditions like generalized anxiety disorder (GAD), insomnia, status epilepticus, and alcohol withdrawal.
Popular benzodiazepines include:
- Diazepam
- Lorazepam
- Alprazolam
- Clonazepam
- Midazolam
- Temazepam
These drugs are important for exams like USMLE, NCLEX, GPAT, and NEET-PG.
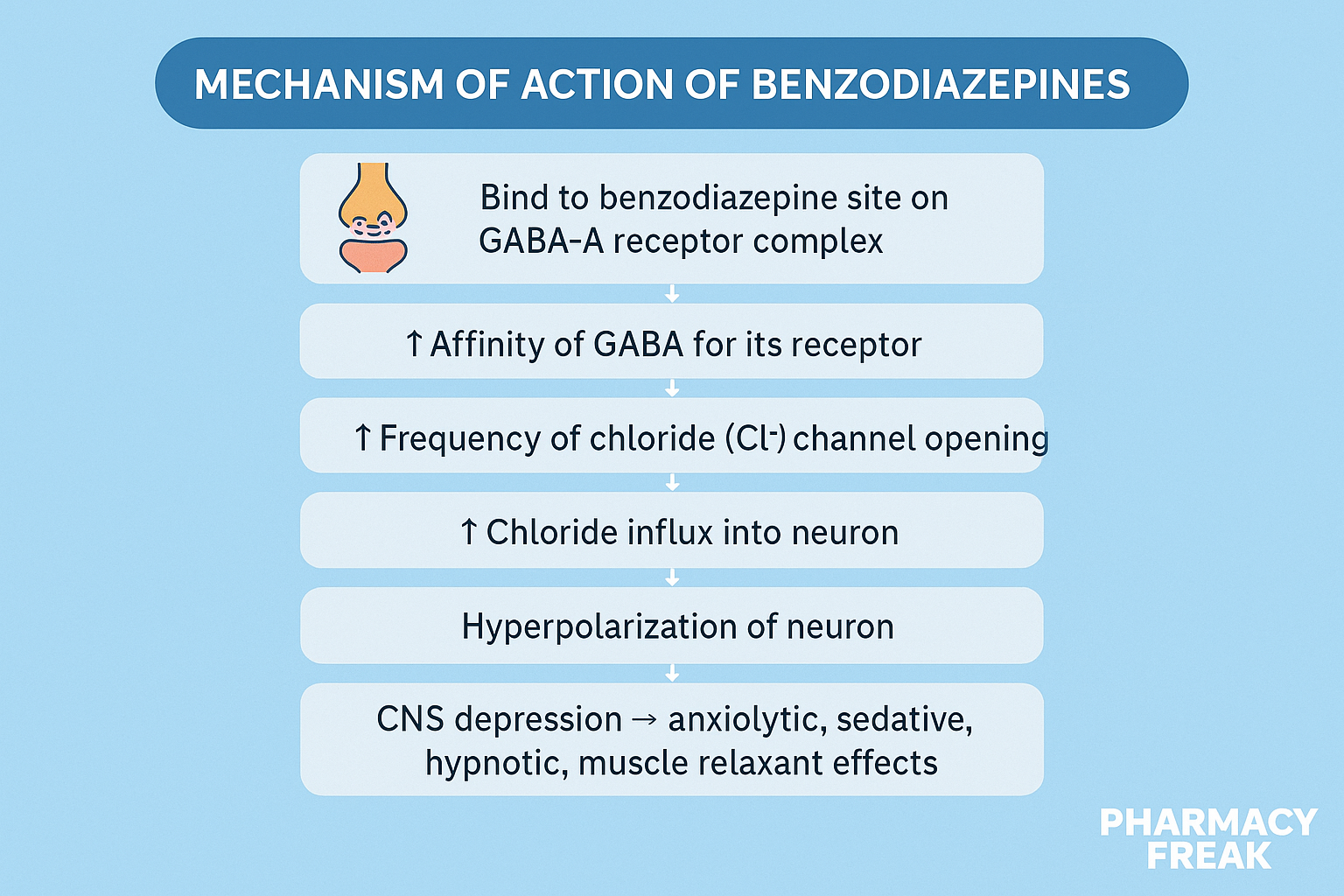
Stepwise Mechanism of Action of Benzodiazepines
- Binding to GABA-A receptor complex
Benzodiazepines bind to a specific site on the GABA-A receptor, located between the α and γ subunits. - Positive allosteric modulation
They do not activate the receptor directly, but act as positive allosteric modulators, enhancing the effect of endogenous GABA. - Increased chloride ion influx
This binding increases the frequency of chloride channel opening in response to GABA. - Hyperpolarization of the neuron
Chloride influx leads to membrane hyperpolarization, making it less likely to fire an action potential. - CNS depression
The result is dose-dependent central nervous system depression, with effects ranging from anxiolysis to sedation, hypnosis, and coma.
Pharmacokinetic Parameters of Benzodiazepines
| Drug | Onset | Half-life | Metabolism | Notes |
|---|---|---|---|---|
| Diazepam | Rapid | 20–50 hrs | Hepatic (active metabolites) | Long-acting |
| Lorazepam | Intermediate | 10–20 hrs | Hepatic (no active metabolite) | Preferred in elderly |
| Alprazolam | Intermediate | 12–15 hrs | Hepatic | High abuse potential |
| Clonazepam | Slow | 18–50 hrs | Hepatic | Used in epilepsy |
| Midazolam | Rapid | 1.5–2.5 hrs | Hepatic | Used in anesthesia |
Clinical Uses of Benzodiazepines
- Generalized anxiety disorder (GAD)
- Panic disorder
- Acute agitation
- Insomnia (short-term use)
- Seizures and status epilepticus (lorazepam, diazepam)
- Alcohol withdrawal
- Muscle spasms
- Premedication before procedures (e.g., midazolam)
Adverse Effects of Benzodiazepines
- Sedation and drowsiness
- Cognitive impairment and confusion
- Anterograde amnesia
- Motor incoordination and falls
- Respiratory depression (especially with opioids)
- Tolerance and dependence
- Withdrawal symptoms – rebound anxiety, insomnia, seizures
- Paradoxical agitation (rare, especially in elderly)
Comparative Analysis: Benzodiazepines vs Barbiturates
| Feature | Benzodiazepines | Barbiturates |
|---|---|---|
| GABA-A interaction | ↑ Frequency of Cl⁻ channel | ↑ Duration of Cl⁻ channel |
| Safety profile | Safer | Narrow therapeutic index |
| Risk of overdose | Low (alone) | High |
| Reversal agent | Flumazenil | None |
| Abuse potential | Moderate | High |
Practice MCQs
Q1. Benzodiazepines bind to which receptor?
a. NMDA
b. GABA-B
c. GABA-A ✅
d. AMPA
Q2. What is the mechanism of benzodiazepines at the receptor level?
a. Direct agonism
b. Inhibit GABA
c. Increase GABA release
d. Enhance GABA effect allosterically ✅
Q3. Benzodiazepines increase the:
a. Duration of Cl⁻ channel opening
b. Frequency of Cl⁻ channel opening ✅
c. GABA synthesis
d. Glutamate release
Q4. Which benzodiazepine is commonly used in seizures?
a. Alprazolam
b. Diazepam ✅
c. Temazepam
d. Flurazepam
Q5. Which of the following has no active metabolite and is preferred in elderly?
a. Diazepam
b. Alprazolam
c. Lorazepam ✅
d. Midazolam
Q6. Which condition is a contraindication for long-term benzodiazepine use?
a. Short-term insomnia
b. Panic attacks
c. Chronic anxiety ✅
d. Pre-op sedation
Q7. Which is the reversal agent for benzodiazepine overdose?
a. Naloxone
b. Atropine
c. Flumazenil ✅
d. Protamine
Q8. Which is a rare paradoxical effect of benzodiazepines?
a. Sedation
b. Anterograde amnesia
c. Euphoria
d. Agitation ✅
Q9. Benzodiazepines act primarily by:
a. Enhancing serotonin
b. Blocking norepinephrine
c. Enhancing GABAergic inhibition ✅
d. Increasing dopamine
Q10. Which drug has the shortest half-life?
a. Clonazepam
b. Diazepam
c. Midazolam ✅
d. Lorazepam
FAQs
Q1: Are benzodiazepines addictive?
Yes. Long-term use can lead to tolerance, dependence, and withdrawal.
Q2: Can they be used for long-term anxiety?
No. Safer alternatives like SSRIs are preferred for chronic anxiety.
Q3: Are they safe in the elderly?
Use with caution. Prefer lorazepam or oxazepam due to lack of active metabolites.
Q4: Can they cause respiratory depression?
Yes, especially when combined with opioids or alcohol.
Q5: Is there an antidote for overdose?
Yes, flumazenil is a benzodiazepine receptor antagonist.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Review of Pharmacology – Sparsh Gupta
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK532879/
I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com