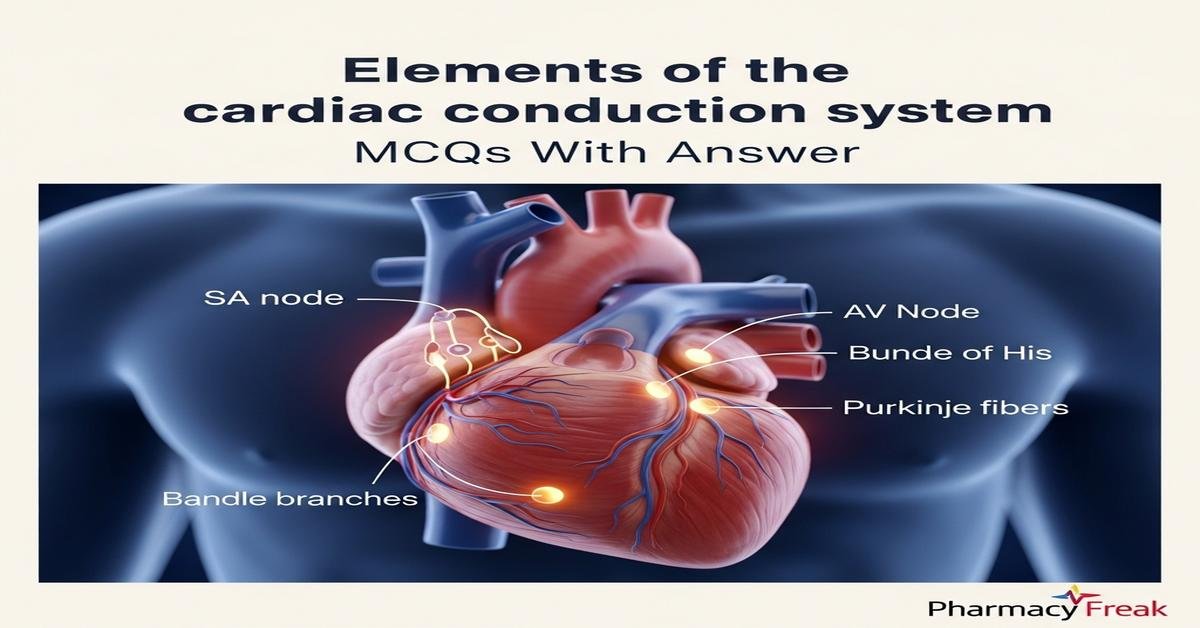
The cardiac conduction system coordinates heart rhythm through specialized structures—SA node, AV node, bundle of His, bundle branches, and Purkinje fibers—ensuring synchronized atrial and ventricular contraction. Understanding electrical conduction, pacemaker potentials, refractory periods and ion channel physiology is essential for B. Pharm students studying cardiovascular pharmacology and antiarrhythmic drug actions. Knowledge of conduction pathways, conduction velocity, autonomic modulation and common arrhythmias links basic electrophysiology to drug mechanisms and therapeutic strategies. This foundation helps predict drug effects, adverse reactions, and rational prescribing. Clear grasp of anatomy, physiology and electrophysiology of the conduction system enhances clinical reasoning and pharmacotherapy competence. Now let’s test your knowledge with 30 MCQs on this topic.
Q1. Which structure is the primary pacemaker of the heart under normal physiological conditions?
- Sinoatrial (SA) node
- Atrioventricular (AV) node
- Bundle of His
- Purkinje fibers
Correct Answer: Sinoatrial (SA) node
Q2. Which ionic current is primarily responsible for phase 4 spontaneous depolarization in SA nodal cells?
- Fast sodium (INa)
- Funny current (If) carried by HCN channels
- L-type calcium current (ICa,L)
- Delayed rectifier potassium current (IK)
Correct Answer: Funny current (If) carried by HCN channels
Q3. In pacemaker action potentials, which phase corresponds to the rapid upstroke in SA nodal cells?
- Phase 0 due to sodium influx
- Phase 0 due to L-type calcium influx
- Phase 1 due to transient outward potassium current
- Phase 3 due to delayed rectifier potassium current
Correct Answer: Phase 0 due to L-type calcium influx
Q4. Which region has the fastest intrinsic conduction velocity?
- Atrial myocardium
- AV node
- Purkinje fibers
- Ventricular myocardium
Correct Answer: Purkinje fibers
Q5. Which channel blockade is the main action of Class III antiarrhythmic drugs?
- Sodium channel blockade
- Beta-adrenergic receptor blockade
- Potassium channel blockade to prolong repolarization
- Calcium channel blockade at L-type channels
Correct Answer: Potassium channel blockade to prolong repolarization
Q6. Adenosine terminates certain supraventricular tachycardias primarily by:
- Blocking fast sodium channels in atrial myocytes
- Activating A1 receptors to increase AV nodal potassium conductance and hyperpolarize cells
- Inhibiting L-type calcium channels in ventricles
- Stimulating beta-1 receptors to decrease AV conduction
Correct Answer: Activating A1 receptors to increase AV nodal potassium conductance and hyperpolarize cells
Q7. Which ECG change is most characteristic of first-degree AV block?
- Progressively lengthening PR interval until a dropped beat
- Constantly prolonged PR interval greater than 200 ms
- Complete dissociation between P waves and QRS complexes
- Widened QRS complexes with left-axis deviation
Correct Answer: Constantly prolonged PR interval greater than 200 ms
Q8. Which electrolyte disturbance most commonly decreases membrane excitability and slows conduction in the heart?
- Hypokalemia
- Hyperkalemia
- Hyponatremia
- Hypocalcemia
Correct Answer: Hyperkalemia
Q9. Which protein forms gap junction channels that electrically couple cardiomyocytes?
- Actin
- Troponin
- Connexins
- Dystrophin
Correct Answer: Connexins
Q10. In the context of re-entrant arrhythmias, a substrate required to sustain re-entry includes:
- Homogeneous conduction velocity and refractory period
- An anatomical or functional conduction block creating a circuit with slow conduction in one limb
- Global increase in automaticity in all atrial cells
- Complete absence of gap junctions throughout the myocardium
Correct Answer: An anatomical or functional conduction block creating a circuit with slow conduction in one limb
Q11. Which antiarrhythmic drug class primarily slows phase 0 depolarization in ventricular myocytes?
- Class I (sodium channel blockers)
- Class II (beta blockers)
- Class III (potassium channel blockers)
- Class IV (calcium channel blockers)
Correct Answer: Class I (sodium channel blockers)
Q12. The His-Purkinje system initiates ventricular depolarization; dysfunction here most likely produces which ECG finding?
- Prolonged PR interval only
- Bundle branch block with widened QRS complex
- ST-segment elevation
- Peaked T waves only
Correct Answer: Bundle branch block with widened QRS complex
Q13. Which statement about AV nodal conduction is correct?
- AV node has faster conduction velocity than Purkinje fibers
- AV node provides a physiologic delay to allow ventricular filling
- AV node is the primary pacemaker under normal conditions
- AV nodal cells rely primarily on fast sodium current for phase 0
Correct Answer: AV node provides a physiologic delay to allow ventricular filling
Q14. Which ion channel alteration explains how Class IV antiarrhythmics decrease AV nodal conduction?
- Blockade of L-type calcium channels reducing calcium influx during phase 0 in nodal cells
- Inhibition of HCN channels reducing If current
- Enhancement of delayed rectifier potassium currents
- Blockade of fast sodium channels in Purkinje fibers
Correct Answer: Blockade of L-type calcium channels reducing calcium influx during phase 0 in nodal cells
Q15. Digitalis toxicity often causes arrhythmias by which primary electrophysiologic mechanism?
- Excessive beta-adrenergic stimulation
- Increased intracellular calcium leading to delayed afterdepolarizations (DADs)
- Prolonged repolarization causing early afterdepolarizations (EADs)
- Blockade of HCN channels causing bradycardia only
Correct Answer: Increased intracellular calcium leading to delayed afterdepolarizations (DADs)
Q16. Which change on action potential duration and effective refractory period is expected with potassium channel blockers?
- Shortened AP duration and shortened ERP
- Prolonged AP duration and prolonged ERP
- No change in AP duration but shortened ERP
- Prolonged AP duration but shortened ERP
Correct Answer: Prolonged AP duration and prolonged ERP
Q17. Which autonomic effect increases heart rate by acting on the SA node?
- Vagal stimulation increasing acetylcholine release
- Sympathetic stimulation increasing cAMP and If current
- Increased baroreceptor firing causing decreased sympathetic output
- Parasympathetic stimulation decreasing If current
Correct Answer: Sympathetic stimulation increasing cAMP and If current
Q18. The “funny” current (If) is permeable to which ions and modulated by which second messenger?
- Permeable to chloride and inhibited by cGMP
- Permeable to sodium and potassium and enhanced by cAMP
- Permeable to calcium only and activated by IP3
- Permeable to potassium only and inhibited by cAMP
Correct Answer: Permeable to sodium and potassium and enhanced by cAMP
Q19. A patient with Wolff-Parkinson-White (WPW) syndrome has an accessory pathway (bundle of Kent). Which ECG feature is typical?
- Prolonged PR interval and narrow QRS
- Short PR interval and a delta wave with widened QRS
- ST depression and peaked T waves
- U waves and low voltage QRS
Correct Answer: Short PR interval and a delta wave with widened QRS
Q20. Which drug would be most appropriate to acutely slow AV nodal conduction in atrial fibrillation to control ventricular rate?
- Amiodarone intravenous bolus
- IV verapamil or diltiazem (non-dihydropyridine calcium channel blockers)
- Digoxin oral loading only
- Class Ic agent like flecainide IV
Correct Answer: IV verapamil or diltiazem (non-dihydropyridine calcium channel blockers)
Q21. Which property best describes Class IA antiarrhythmics such as procainamide?
- Marked beta-blockade with no sodium channel effect
- Moderate sodium channel blockade with potassium channel blockade, prolonging QT
- Pure potassium channel blockade shortening action potential
- Selective AV nodal calcium channel blockade
Correct Answer: Moderate sodium channel blockade with potassium channel blockade, prolonging QT
Q22. Which mechanism is most likely responsible for atrial fibrillation maintenance in the remodeled atrium?
- Enhanced uniform automaticity across atrial tissue
- Multiple micro-reentrant circuits due to heterogenous conduction and refractory periods
- Complete loss of SA nodal function only
- Isolated Purkinje fiber triggered activity in ventricles
Correct Answer: Multiple micro-reentrant circuits due to heterogenous conduction and refractory periods
Q23. Hypokalemia predisposes to which arrhythmogenic mechanism?
- Enhanced Na+/K+ pump activity preventing afterdepolarizations
- Prolonged repolarization and increased risk of early afterdepolarizations (EADs)
- Shortened action potential duration and decreased ectopy
- Increased gap junction conductance leading to uniform conduction
Correct Answer: Prolonged repolarization and increased risk of early afterdepolarizations (EADs)
Q24. Which effect on the ECG correlates with slowed conduction through the AV node?
- Prolongation of the PR interval
- Widening of the QRS complex
- Elevation of the ST segment
- Inversion of the T wave only
Correct Answer: Prolongation of the PR interval
Q25. Which statement about Purkinje fibers is true?
- They have the highest resting membrane potential and do not conduct rapidly
- They rely predominantly on fast sodium channels for rapid phase 0 conduction
- They are the primary site of autonomic pacemaking under normal conditions
- They lack gap junctions and conduct purely by local currents
Correct Answer: They rely predominantly on fast sodium channels for rapid phase 0 conduction
Q26. Which antiarrhythmic strategy specifically increases the effective refractory period of the AV node to prevent rapid ventricular response?
- Enhancing sodium conductance in AV nodal cells
- Blocking L-type calcium channels or increasing vagal tone
- Blocking delayed rectifier potassium channels only in ventricles
- Stimulating HCN channels to increase If
Correct Answer: Blocking L-type calcium channels or increasing vagal tone
Q27. Early afterdepolarizations (EADs) are most often associated with which condition?
- Short QT interval due to hypercalcemia
- Prolonged action potential duration, often from hypokalemia or Class III drugs
- Increased conduction velocity in Purkinje fibers
- Decreased intracellular calcium and suppressed automaticity
Correct Answer: Prolonged action potential duration, often from hypokalemia or Class III drugs
Q28. Which statement best describes the role of the AV node during atrial premature beats?
- AV node always conducts premature atrial impulses without delay
- AV node can exhibit decremental conduction, increasing delay for premature impulses and sometimes blocking them
- AV node speeds up conduction for premature impulses to preserve rhythm
- AV node converts premature atrial impulses into ventricular tachycardia
Correct Answer: AV node can exhibit decremental conduction, increasing delay for premature impulses and sometimes blocking them
Q29. Which laboratory test or measurement is most important when starting a drug known to prolong QT interval?
- Serum magnesium only
- Baseline and follow-up ECG to monitor QTc interval
- Lipid profile to assess cardiovascular risk
- Complete blood count for leukopenia risk
Correct Answer: Baseline and follow-up ECG to monitor QTc interval
Q30. Which electrophysiologic feature distinguishes nodal (AV) tissue from ventricular working myocardium?
- Nodal tissue has a stable resting membrane potential and fast sodium-dependent phase 0
- Nodal tissue shows slow, calcium-dependent phase 0 and lacks a true phase 1 notch
- Nodal cells have larger amplitude action potentials and faster conduction velocity
- Nodal tissue is unaffected by autonomic neurotransmitters
Correct Answer: Nodal tissue shows slow, calcium-dependent phase 0 and lacks a true phase 1 notch

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com