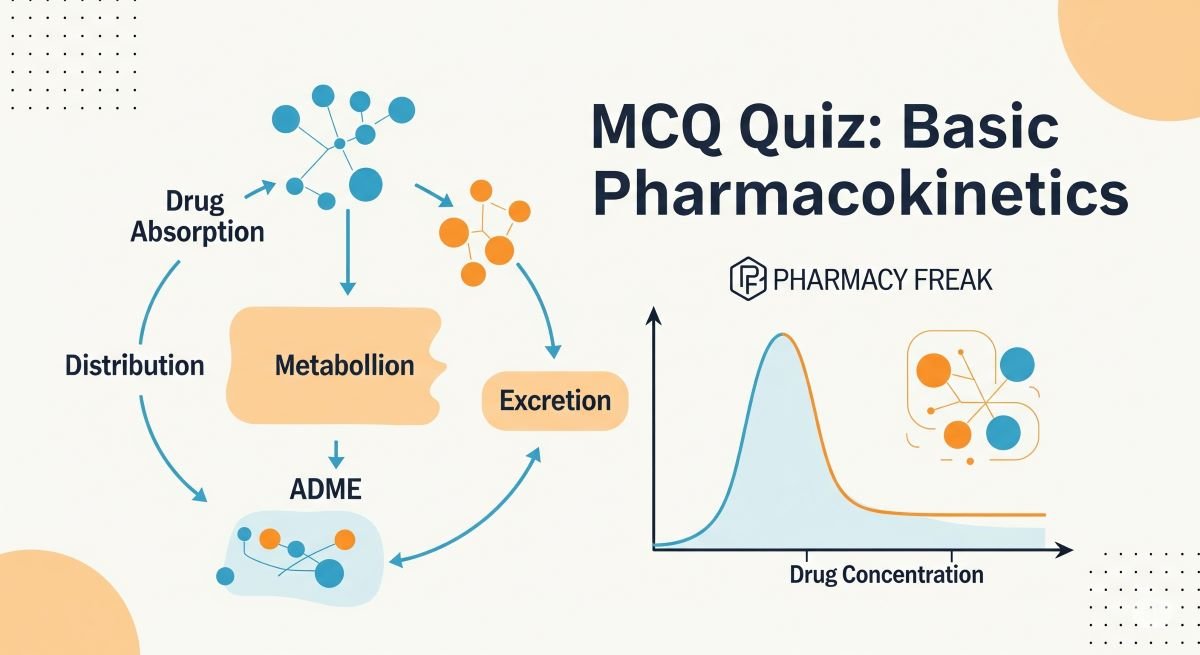
Welcome, PharmD students, to your MCQ quiz on Basic Pharmacokinetics! Building on introductory concepts, this quiz delves deeper into the fundamental principles governing how drugs move through and are processed by the body (ADME). Understanding key parameters like volume of distribution, clearance, half-life, and the orders of drug elimination is essential for designing safe and effective dosing regimens. This quiz will test your grasp of these core pharmacokinetic concepts and their clinical significance. Let’s reinforce your knowledge!
1. The four main processes in pharmacokinetics (ADME) are Absorption, Distribution, Metabolism, and:
- a) Efficacy
- b) Elimination (Excretion)
- c) Potency
- d) Reaction
Answer: b) Elimination (Excretion)
2. The fraction of an administered drug that reaches the systemic circulation unchanged is known as:
- a) Clearance (CL)
- b) Bioavailability (F)
- c) Volume of distribution (Vd)
- d) Half-life (t½)
Answer: b) Bioavailability (F)
3. Which pharmacokinetic parameter describes the theoretical volume into which a drug distributes in the body to achieve the concentration observed in plasma?
- a) Elimination rate constant (k)
- b) Area Under the Curve (AUC)
- c) Clearance (CL)
- d) Volume of distribution (Vd)
Answer: d) Volume of distribution (Vd)
4. A drug with first-order elimination kinetics means that:
- a) A constant amount of drug is eliminated per unit of time.
- b) The rate of drug elimination is proportional to the plasma drug concentration.
- c) The elimination half-life changes with the dose.
- d) The drug is not metabolized before excretion.
Answer: b) The rate of drug elimination is proportional to the plasma drug concentration.
5. The elimination half-life (t½) of a drug is the time required for:
- a) The drug to exert its maximum therapeutic effect.
- b) The plasma drug concentration to increase by 50%.
- c) The plasma drug concentration to decrease by 50%.
- d) Complete absorption of the drug.
Answer: c) The plasma drug concentration to decrease by 50%.
6. Drug clearance (CL) is best defined as:
- a) The amount of drug eliminated from the body per unit time.
- b) The volume of plasma cleared of drug per unit time.
- c) The time it takes for the drug concentration to halve.
- d) The extent of drug distribution into tissues.
Answer: b) The volume of plasma cleared of drug per unit time.
7. If a drug has an elimination half-life of 4 hours, what percentage of the drug will remain in the body after 12 hours (assuming first-order kinetics)?
- a) 50%
- b) 25%
- c) 12.5%
- d) 6.25%
Answer: c) 12.5% (After 1 t½ (4h) = 50%; After 2 t½ (8h) = 25%; After 3 t½ (12h) = 12.5%)
8. The Area Under the Curve (AUC) of a plasma drug concentration-time graph is a measure of:
- a) The peak plasma concentration (Cmax).
- b) The time to reach peak concentration (Tmax).
- c) The total systemic exposure to the drug.
- d) The rate of drug absorption.
Answer: c) The total systemic exposure to the drug.
9. For a drug that follows first-order elimination, the elimination rate constant (k) can be calculated from the half-life (t½) using the formula:
- a) k = t½ / 0.693
- b) k = 0.693 / t½
- c) k = t½ * 0.693
- d) k = 1 / (t½ * 0.693)
Answer: b) k = 0.693 / t½
10. Zero-order elimination kinetics are characterized by:
- a) A constant fraction of drug eliminated per unit time.
- b) A constant amount of drug eliminated per unit time, regardless of concentration.
- c) An elimination rate proportional to drug concentration.
- d) A constant elimination half-life.
Answer: b) A constant amount of drug eliminated per unit time, regardless of concentration.
11. The volume of distribution (Vd) relates the amount of drug in the body to the:
- a) Dose administered.
- b) Concentration of drug in the urine.
- c) Concentration of drug in the plasma.
- d) Rate of drug metabolism.
Answer: c) Concentration of drug in the plasma.
12. If a drug is highly bound to plasma proteins, its apparent volume of distribution (Vd) will likely be:
- a) Larger, because more drug is in the tissues.
- b) Smaller, because more drug is retained in the vascular compartment.
- c) Unaffected by protein binding.
- d) Equal to total body water.
Answer: b) Smaller, because more drug is retained in the vascular compartment.
13. Total body clearance (CL_total) is the sum of clearances from all eliminating organs. For many drugs, this is primarily:
- a) CL_renal + CL_pulmonary
- b) CL_hepatic + CL_biliary
- c) CL_renal + CL_hepatic
- d) CL_skin + CL_salivary
Answer: c) CL_renal + CL_hepatic
14. “Steady state” concentration (Css) is achieved when:
- a) The rate of drug administration is zero.
- b) The rate of drug absorption equals the rate of drug distribution.
- c) The rate of drug administration equals the rate of drug elimination.
- d) The drug is completely eliminated from the body.
Answer: c) The rate of drug administration equals the rate of drug elimination.
15. For a drug administered by continuous intravenous infusion, the time to reach steady state depends primarily on the drug’s:
- a) Dose
- b) Infusion rate
- c) Elimination half-life
- d) Volume of distribution
Answer: c) Elimination half-life
16. A loading dose is sometimes administered to:
- a) Decrease the drug’s half-life.
- b) Reduce the bioavailability of the drug.
- c) Achieve therapeutic drug concentrations more rapidly for drugs with long half-lives.
- d) Increase the rate of drug metabolism.
Answer: c) Achieve therapeutic drug concentrations more rapidly for drugs with long half-lives.
17. For a drug eliminated by first-order kinetics, how many half-lives does it generally take to reach approximately 94-97% of steady-state concentration?
- a) 1-2
- b) 2-3
- c) 4-5
- d) More than 7
Answer: c) 4-5
18. The equation CL = k * Vd relates which three pharmacokinetic parameters?
- a) Clearance, absorption rate constant, and volume of distribution.
- b) Clearance, elimination rate constant, and bioavailability.
- c) Clearance, elimination rate constant, and volume of distribution.
- d) Clearance, half-life, and dose.
Answer: c) Clearance, elimination rate constant, and volume of distribution.
19. Hepatic clearance can be affected by:
- a) Only blood flow to the liver.
- b) Only the intrinsic metabolizing activity of liver enzymes.
- c) Only plasma protein binding.
- d) Blood flow to the liver, plasma protein binding, and intrinsic enzyme activity.
Answer: d) Blood flow to the liver, plasma protein binding, and intrinsic enzyme activity.
20. Renal clearance of a drug involves which processes?
- a) Only glomerular filtration.
- b) Only active tubular secretion.
- c) Only passive tubular reabsorption.
- d) Glomerular filtration, active tubular secretion, and passive tubular reabsorption.
Answer: d) Glomerular filtration, active tubular secretion, and passive tubular reabsorption.
21. If a drug is primarily reabsorbed in the renal tubules, its renal clearance will be ________ than the glomerular filtration rate (GFR).
- a) Greater
- b) Less
- c) Equal to
- d) Unrelated to
Answer: b) Less
22. Altering urine pH can significantly affect the renal excretion of drugs that are:
- a) Highly protein-bound.
- b) Weak acids or weak bases, by changing their degree of ionization and reabsorption.
- c) Excreted solely by glomerular filtration.
- d) Metabolized by the kidney.
Answer: b) Weak acids or weak bases, by changing their degree of ionization and reabsorption.
23. For a drug given orally, the average steady-state concentration (Css,avg) is determined by:
- a) Only the dose.
- b) Only the dosing interval.
- c) (Dose * F) / (CL * dosing interval).
- d) Only the clearance.
Answer: c) (Dose * F) / (CL * dosing interval).
24. The “peak” plasma drug concentration (Cmax) after an oral dose occurs when:
- a) The rate of drug elimination is maximal.
- b) The rate of drug absorption equals the rate of drug elimination.
- c) All of the drug has been absorbed.
- d) The drug begins to distribute into tissues.
Answer: b) The rate of drug absorption equals the rate of drug elimination.
25. The “trough” plasma drug concentration (Cmin) at steady state is the:
- a) Maximum concentration achieved after a dose.
- b) Average concentration during the dosing interval.
- c) Minimum concentration observed just before the next dose.
- d) Concentration at which the drug is 50% eliminated.
Answer: c) Minimum concentration observed just before the next dose.
26. Which of the following scenarios would most likely lead to drug accumulation?
- a) Dosing interval is much longer than the drug’s half-life.
- b) Dosing interval is shorter than the drug’s half-life, and the drug is given repeatedly.
- c) The drug has very low bioavailability.
- d) The drug has a very large volume of distribution.
Answer: b) Dosing interval is shorter than the drug’s half-life, and the drug is given repeatedly.
27. A drug with a high extraction ratio by the liver means that:
- a) Its hepatic clearance is primarily limited by intrinsic enzyme activity.
- b) Its hepatic clearance is primarily limited by liver blood flow.
- c) It has very low oral bioavailability due to diffusion barriers.
- d) It is not significantly metabolized by the liver.
Answer: b) Its hepatic clearance is primarily limited by liver blood flow.
28. Creatinine clearance is often used as an estimate of:
- a) Hepatic function
- b) Glomerular filtration rate (GFR) and thus renal function
- c) Drug absorption rate
- d) Plasma protein binding
Answer: b) Glomerular filtration rate (GFR) and thus renal function
29. If the volume of distribution (Vd) of a drug increases (e.g., due to a disease state), and clearance remains constant, the drug’s half-life will:
- a) Decrease
- b) Increase
- c) Remain unchanged
- d) Become zero
Answer: b) Increase (Since t½ = (0.693 * Vd) / CL)
30. If the clearance (CL) of a drug decreases (e.g., due to renal impairment), and Vd remains constant, the drug’s half-life will:
- a) Decrease
- b) Increase
- c) Remain unchanged
- d) Become unpredictable
Answer: b) Increase
31. For most drugs, which order of kinetics describes their elimination at therapeutic concentrations?
- a) Zero-order kinetics
- b) First-order kinetics
- c) Second-order kinetics
- d) Mixed-order kinetics
Answer: b) First-order kinetics
32. The pharmacokinetic concept of “linearity” implies that as the dose increases:
- a) The AUC increases disproportionately more.
- b) The AUC increases proportionally.
- c) The half-life decreases.
- d) Clearance increases.
Answer: b) The AUC increases proportionally.
33. What does a one-compartment body model assume regarding drug distribution?
- a) Drug distributes into multiple distinct tissue compartments at different rates.
- b) Drug distributes instantaneously and homogeneously throughout a single, uniform compartment (the body).
- c) Drug remains only in the plasma.
- d) Drug distribution is a zero-order process.
Answer: b) Drug distributes instantaneously and homogeneously throughout a single, uniform compartment (the body).
34. A two-compartment model often better describes drugs that:
- a) Are eliminated solely by the kidneys.
- b) Distribute rapidly into a central compartment (e.g., blood and highly perfused organs) and then more slowly into a peripheral tissue compartment.
- c) Follow zero-order elimination.
- d) Have very small volumes of distribution.
Answer: b) Distribute rapidly into a central compartment (e.g., blood and highly perfused organs) and then more slowly into a peripheral tissue compartment.
35. The “distribution phase” in a two-compartment model is characterized by:
- a) A slower decline in plasma concentration as the drug equilibrates with tissues.
- b) A rapid decline in plasma concentration primarily due to drug distribution out of the central compartment.
- c) Only drug elimination occurring.
- d) A constant plasma concentration.
Answer: b) A rapid decline in plasma concentration primarily due to drug distribution out of the central compartment.
36. The “elimination phase” in a pharmacokinetic model primarily reflects:
- a) Drug absorption from the site of administration.
- b) Drug distribution into deep tissue compartments.
- c) The removal of drug from the body through metabolism and excretion.
- d) The drug binding to plasma proteins.
Answer: c) The removal of drug from the body through metabolism and excretion.
37. The bioavailability (F) of an orally administered drug can be calculated by comparing the _______ after oral administration to the _______ after IV administration of the same dose.
- a) Cmax / Cmax
- b) Tmax / Tmax
- c) AUC / AUC
- d) Vd / Vd
Answer: c) AUC / AUC
38. Which factor would decrease the oral bioavailability of a drug?
- a) Rapid dissolution in GI fluids.
- b) High stability in gastric acid.
- c) Significant first-pass hepatic metabolism.
- d) High permeability across the intestinal wall.
Answer: c) Significant first-pass hepatic metabolism.
39. The maintenance dose rate required to achieve a target average steady-state concentration (Css,avg) can be calculated as:
- a) Css,avg * Vd
- b) Css,avg / CL
- c) Css,avg * CL
- d) (Css,avg * CL) / F (for oral dosing)
Answer: d) (Css,avg * CL) / F (for oral dosing) (or Css,avg * CL for IV)
40. The loading dose (LD) aims to rapidly achieve a plasma concentration similar to the steady-state concentration and can be calculated as:
- a) (Target Concentration * CL) / F
- b) (Target Concentration * Vd) / F
- c) Target Concentration / k
- d) Target Concentration * t½
Answer: b) (Target Concentration * Vd) / F
41. If a drug follows zero-order elimination, its half-life:
- a) Is constant.
- b) Increases as the concentration decreases.
- c) Decreases as the concentration decreases (i.e., is not constant and depends on concentration).
- d) Is always very short.
Answer: c) Decreases as the concentration decreases (i.e., is not constant and depends on concentration).
42. Saturation of metabolic enzymes can lead to a shift from:
- a) Zero-order to first-order kinetics.
- b) First-order to zero-order kinetics at high drug concentrations.
- c) Active transport to passive diffusion.
- d) Renal excretion to hepatic metabolism.
Answer: b) First-order to zero-order kinetics at high drug concentrations.
43. Therapeutic drug monitoring (TDM) is most useful for drugs that:
- a) Have a very wide therapeutic range.
- b) Exhibit a good correlation between plasma concentration and clinical effects/toxicity, and have a narrow therapeutic range.
- c) Are eliminated solely by zero-order kinetics.
- d) Are administered as a single dose.
Answer: b) Exhibit a good correlation between plasma concentration and clinical effects/toxicity, and have a narrow therapeutic range.
44. Which patient population might require dosage adjustments due to altered pharmacokinetics, particularly renal function?
- a) Young healthy adults
- b) Neonates and elderly patients
- c) Athletes
- d) Patients with only dermatological conditions
Answer: b) Neonates and elderly patients
45. The rate of absorption of a drug from an intramuscular injection can be influenced by:
- a) Only the needle size.
- b) Blood flow to the muscle, drug formulation, and lipid solubility of the drug.
- c) Only the volume injected.
- d) The patient’s hair color.
Answer: b) Blood flow to the muscle, drug formulation, and lipid solubility of the drug.
46. Enterohepatic circulation involves the excretion of a drug or its metabolite into the bile, followed by reabsorption from the:
- a) Kidneys
- b) Lungs
- c) Intestines
- d) Stomach
Answer: c) Intestines
47. For drugs that are weak acids, alkalinization of the urine (increasing urine pH) would generally _______ their renal excretion.
- a) Decrease (by increasing reabsorption of the non-ionized form)
- b) Increase (by increasing ionization and reducing reabsorption)
- c) Have no effect on
- d) Cause precipitation in the tubules
Answer: b) Increase (by increasing ionization and reducing reabsorption)
48. The primary purpose of studying basic pharmacokinetics is to:
- a) Understand the mechanism of drug action at the receptor level.
- b) Develop a rational basis for designing dosage regimens that optimize therapeutic outcomes and minimize toxicity.
- c) Determine the cost-effectiveness of a drug.
- d) Synthesize new drug molecules.
Answer: b) Develop a rational basis for designing dosage regimens that optimize therapeutic outcomes and minimize toxicity.
49. If two oral formulations of the same drug produce similar AUC values but different Cmax and Tmax values, they are considered:
- a) Bioequivalent
- b) Therapeutically identical in all aspects
- c) To have the same absorption rate but different extent of absorption
- d) To have the same extent of absorption but potentially different rates of absorption
Answer: d) To have the same extent of absorption but potentially different rates of absorption
50. Understanding basic pharmacokinetics allows clinicians to predict how physiological changes (e.g., aging, organ dysfunction) or drug interactions might alter:
- a) Only the drug’s color.
- b) The drug’s ADME processes and thus its concentration-time profile.
- c) Only the drug’s taste.
- d) The patient’s preference for the medication.
Answer: b) The drug’s ADME processes and thus its concentration-time profile.

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com

These questions are very well formed and extremely beneficial for students and teachers, Thank you so much