Cardiac arrhythmias are disorders of impulse generation, conduction, or both, and can lead to symptoms like palpitations, dizziness, syncope, or even sudden cardiac death. Antiarrhythmic drugs are agents used to suppress abnormal rhythms and restore normal heart rhythm and rate.
This blog from Pharmacy Freak outlines the classification, clinical uses, drug of choice insights, and adverse effects of antiarrhythmic drugs using key academic references suitable for pharmacology students and professionals.
Table of Contents
What is Antiarrhythmic Drugs
Antiarrhythmic drugs are pharmacological agents used to prevent, suppress, or treat cardiac arrhythmias by altering the electrical conduction pathways of the heart. These agents act on cardiac ion channels or autonomic receptors.
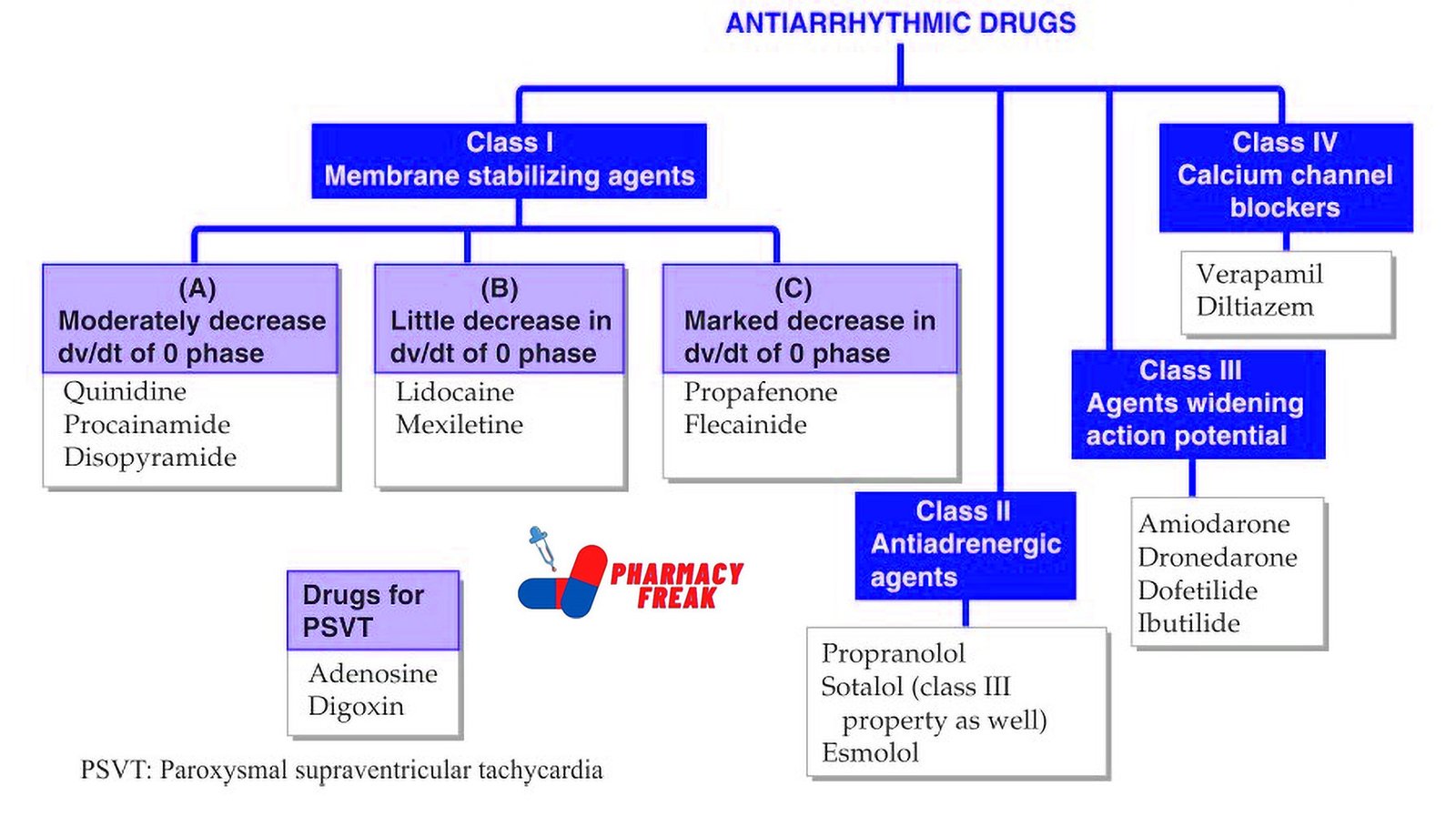
Classification of Antiarrhythmic Drugs (KD Tripathi)
- Class I – Membrane stabilizing agents:
(A) Moderately decrease dv/dt of phase 0: Quinidine, Procainamide, Disopyramide
(B) Little decrease in dv/dt of phase 0: Lidocaine, Mexiletine
(C) Marked decrease in dv/dt of phase 0: Propafenone, Flecainide - Class II – Antiadrenergic agents: Propranolol, Sotalol (also has Class III property), Esmolol
- Class III – Agents widening action potential: Amiodarone, Dronedarone, Dofetilide, Ibutilide
- Class IV – Calcium channel blockers: Verapamil, Diltiazem
Drugs for PSVT (Paroxysmal Supraventricular Tachycardia): Adenosine, Digoxin
Classification (General)
The most widely used classification is the Vaughan Williams Classification, which categorizes antiarrhythmics into five main classes:
Class I – Sodium Channel Blockers
- These drugs inhibit fast sodium channels, reducing phase 0 depolarization in myocardial cells. They are further subdivided into:
- Class IA: Moderate Na+ channel blockade; prolong action potential duration
Examples: Quinidine, Procainamide, Disopyramide
Use: Atrial and ventricular arrhythmias - Class IB: Weak Na+ channel blockade; shorten action potential duration
Examples: Lidocaine, Mexiletine, Phenytoin
Use: Ventricular arrhythmias, especially post-MI - Class IC: Strong Na+ channel blockade; minimal effect on action potential duration
Examples: Flecainide, Propafenone
Use: Supraventricular arrhythmias in structurally normal hearts
Class II – Beta Blockers
These drugs block beta-adrenergic receptors, reducing sympathetic stimulation.
Examples: Propranolol, Metoprolol, Esmolol
Use: Rate control in atrial fibrillation, supraventricular tachycardia, and prevention of post-MI arrhythmias
Class III – Potassium Channel Blockers
They prolong repolarization by blocking potassium channels, thereby increasing the action potential duration and refractory period.
Examples: Amiodarone, Sotalol, Dofetilide, Ibutilide
Use: Atrial fibrillation, ventricular tachycardia, and re-entrant arrhythmias
Note: Amiodarone is one of the most effective but has significant toxicity
Class IV – Calcium Channel Blockers
These inhibit L-type calcium channels, primarily affecting the SA and AV nodes.
Examples: Verapamil, Diltiazem
Use: Supraventricular tachycardias, rate control in atrial fibrillation
Class V – Miscellaneous Agents
These act through different or multiple mechanisms and do not fall into the above classes.
- Adenosine – Inhibits AV nodal conduction; used for acute termination of paroxysmal supraventricular tachycardia
- Digoxin – Increases vagal tone, slows AV conduction; used in atrial fibrillation with CHF
- Magnesium sulfate – Used in torsades de pointes and digitalis-induced arrhythmias
- Ivabradine – Inhibits funny current (If) in SA node; used in heart rate control in heart failure
Uses
Antiarrhythmic drugs are used in the treatment of:
- Supraventricular arrhythmias (e.g., atrial fibrillation, AV nodal reentrant tachycardia)
- Ventricular arrhythmias (e.g., ventricular tachycardia, ventricular fibrillation)
- Rate control in atrial fibrillation
- Post-myocardial infarction arrhythmias
- Congenital long QT syndrome
- Drug-induced arrhythmias
Drug of Choice Highlights
- Atrial fibrillation – Rate control: Metoprolol or Diltiazem; Rhythm control: Amiodarone
- Acute PSVT – Adenosine (IV push)
- Ventricular arrhythmia post-MI – Lidocaine
- Digitalis-induced arrhythmias – Phenytoin or Magnesium sulfate
- Torsades de pointes – Magnesium sulfate
- Prevention of post-MI arrhythmias – Beta blockers
- Atrial flutter – Amiodarone or Dofetilide
Side Effects
Class I
- IA (Quinidine) – Cinchonism, torsades de pointes
- IB (Lidocaine) – CNS toxicity (tremor, confusion)
- IC (Flecainide) – Proarrhythmic in structural heart disease
Class II
- Bradycardia, hypotension, bronchospasm (non-selective beta blockers)
Class III
- Amiodarone – Pulmonary fibrosis, hepatotoxicity, thyroid dysfunction, corneal deposits, photosensitivity
- Sotalol – QT prolongation, torsades de pointes
Class IV
- Constipation (Verapamil), bradycardia, AV block, hypotension
Class V
- Adenosine – Transient asystole, flushing, chest pain
- Digoxin – Bradyarrhythmias, AV block, GI symptoms, visual disturbances
- Magnesium – Hypotension, respiratory depression at high doses
Updated Clinical Pearls
- Amiodarone has properties of all four Vaughan Williams classes but should be used cautiously due to its multi-organ toxicity.
- Beta blockers are the most effective drugs for reducing post-MI mortality and should be included in long-term management.
- In patients with structural heart disease, Class IC agents should be avoided due to proarrhythmic risk.
- Adenosine has a very short half-life and is ideal for emergency use in supraventricular tachycardia.
- Torsades de pointes is typically triggered by prolonged QT interval and is best managed with IV magnesium sulfate.
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 555–566
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 227–231
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 873–889
Related Links

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com