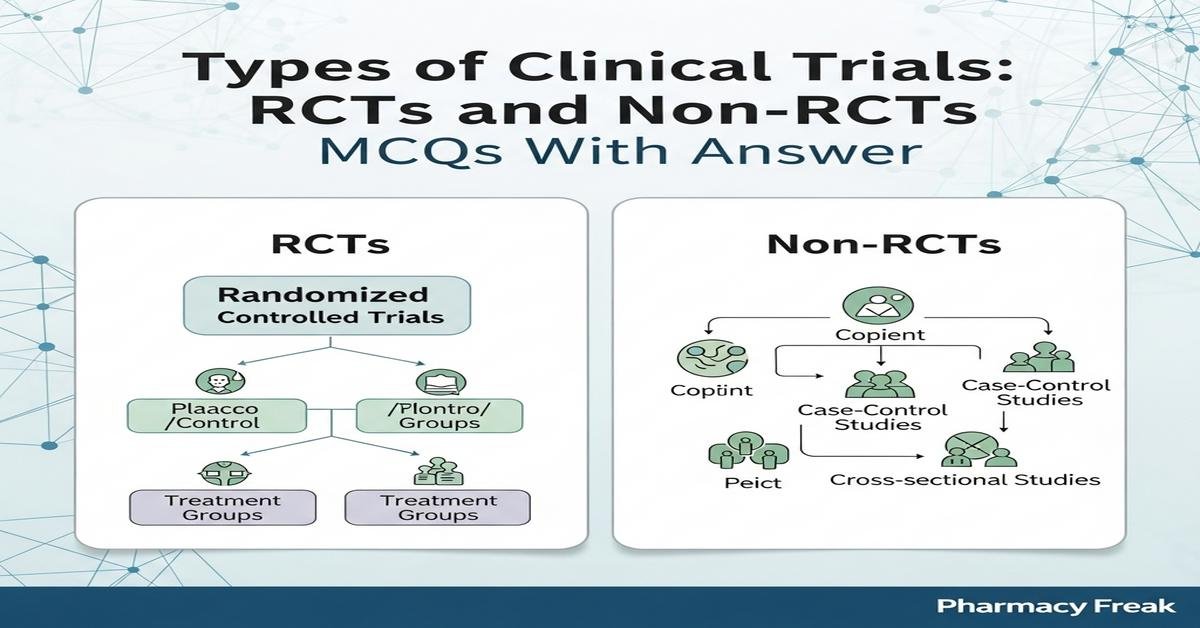
Introduction: This set of MCQs on types of clinical trials—randomized controlled trials (RCTs) and non-randomized trials—is designed specifically for M.Pharm students preparing for advanced exams in Clinical Research and Pharmacovigilance. The questions emphasize trial design principles, bias control, randomization methods, blinding, pragmatic versus explanatory approaches, adaptive and cluster designs, and analytical issues such as intention-to-treat versus per-protocol analyses. Each item tests applied understanding required for designing, appraising, and interpreting clinical trials in drug development and safety monitoring. Use these questions to strengthen conceptual knowledge, recognize methodological pitfalls, and prepare for real-world trial evaluation and regulatory submissions.
Q1. Which feature most clearly distinguishes a randomized controlled trial (RCT) from a non-randomized trial?
- Use of control group
- Prospective data collection
- Random allocation of participants to study arms
- Blinding of outcome assessors
Correct Answer: Random allocation of participants to study arms
Q2. Which type of randomization helps ensure balance of key prognostic factors across treatment groups within small sample sizes?
- Simple randomization
- Block randomization
- Stratified randomization
- Systematic allocation
Correct Answer: Stratified randomization
Q3. Allocation concealment primarily protects against which bias in clinical trials?
- Observer-expectancy bias
- Selection bias
- Attrition bias
- Reporting bias
Correct Answer: Selection bias
Q4. In a double-blind RCT, who is typically unaware of treatment assignments?
- Only the participants
- Only the treating clinicians
- Participants, treating clinicians, and outcome assessors
- Only the outcome assessors
Correct Answer: Participants, treating clinicians, and outcome assessors
Q5. Which trial design is most appropriate when interventions are delivered at the level of groups (e.g., clinics or communities) rather than individuals?
- Crossover trial
- Cluster randomized trial
- Factorial trial
- Parallel individual RCT
Correct Answer: Cluster randomized trial
Q6. A crossover RCT is contraindicated when:
- Outcomes are rapidly reversible after washout
- Toxicity is cumulative and irreversible
- Within-subject variability is low
- Study duration is short with stable condition
Correct Answer: Toxicity is cumulative and irreversible
Q7. Which design element allows an RCT to evaluate two interventions and their interaction simultaneously?
- Factorial design
- Adaptive design
- Stepped-wedge design
- Cross-over design
Correct Answer: Factorial design
Q8. An adaptive trial that changes randomization probabilities to favor better-performing arms during the study is using which approach?
- Response-adaptive randomization
- Stratified randomization
- Minimization
- Blocked randomization
Correct Answer: Response-adaptive randomization
Q9. Which analysis strategy preserves the benefits of randomization by analyzing participants in the groups to which they were originally allocated?
- Per-protocol analysis
- As-treated analysis
- Intention-to-treat analysis
- Post-hoc subgroup analysis
Correct Answer: Intention-to-treat analysis
Q10. Non-randomized controlled trials that use statistical methods to adjust for measured confounders commonly employ which technique?
- Random sequence generation
- Propensity score matching
- Block randomization
- Allocation concealment
Correct Answer: Propensity score matching
Q11. Which non-RCT design is best suited to evaluate the effect of a public health intervention rolled out sequentially to clusters over time?
- Case-control study
- Stepped-wedge cluster trial
- Parallel-group RCT
- Cross-sectional survey
Correct Answer: Stepped-wedge cluster trial
Q12. Equivalence and non-inferiority trials are used primarily to demonstrate:
- That a new treatment is superior to placebo
- That a new treatment is not unacceptably worse than an active comparator
- That treatments have identical molecular mechanisms
- That sample size requirements are minimal
Correct Answer: That a new treatment is not unacceptably worse than an active comparator
Q13. Interim analyses in an RCT are performed to assess early evidence of benefit, harm, or futility. Which safeguard is essential when planning interim analyses?
- Unplanned multiple looks at the data
- Pre-specified stopping rules and statistical adjustment
- Open-label interim reporting to investigators
- Changing primary endpoints during interim review
Correct Answer: Pre-specified stopping rules and statistical adjustment
Q14. Which validity is mainly concerned with the generalizability of trial results to routine clinical populations?
- Internal validity
- Construct validity
- External validity
- Statistical validity
Correct Answer: External validity
Q15. In a non-randomized before-after (pre-post) study evaluating a safety intervention, which major threat undermines causal inference?
- Randomization bias
- Regression to the mean and secular trends
- Allocation concealment failure
- Observer blinding
Correct Answer: Regression to the mean and secular trends
Q16. Minimization as an allocation method in trials primarily aims to:
- Eliminate the need for random numbers
- Achieve balance across multiple prognostic factors
- Guarantee blinding of participants
- Reduce sample size requirements
Correct Answer: Achieve balance across multiple prognostic factors
Q17. Which reporting guideline is most relevant for randomized trials to improve transparency and completeness?
- PRISMA
- STROBE
- CONSORT
- CARE
Correct Answer: CONSORT
Q18. A pragmatic RCT differs from an explanatory RCT primarily by focusing on:
- Mechanistic understanding in ideal conditions
- Efficacy under tightly controlled settings
- Effectiveness in routine clinical practice
- Surrogate endpoints instead of clinical outcomes
Correct Answer: Effectiveness in routine clinical practice
Q19. Which bias is most likely to affect unblinded outcome assessment in subjective endpoints?
- Selection bias
- Detection (assessment) bias
- Attrition bias
- Confounding by indication
Correct Answer: Detection (assessment) bias
Q20. When using historical controls instead of concurrent controls, the principal limitation is:
- Improved internal validity
- Reduced risk of confounding
- Potential for bias due to changes over time (secular trends)
- Enhanced randomization
Correct Answer: Potential for bias due to changes over time (secular trends)

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com