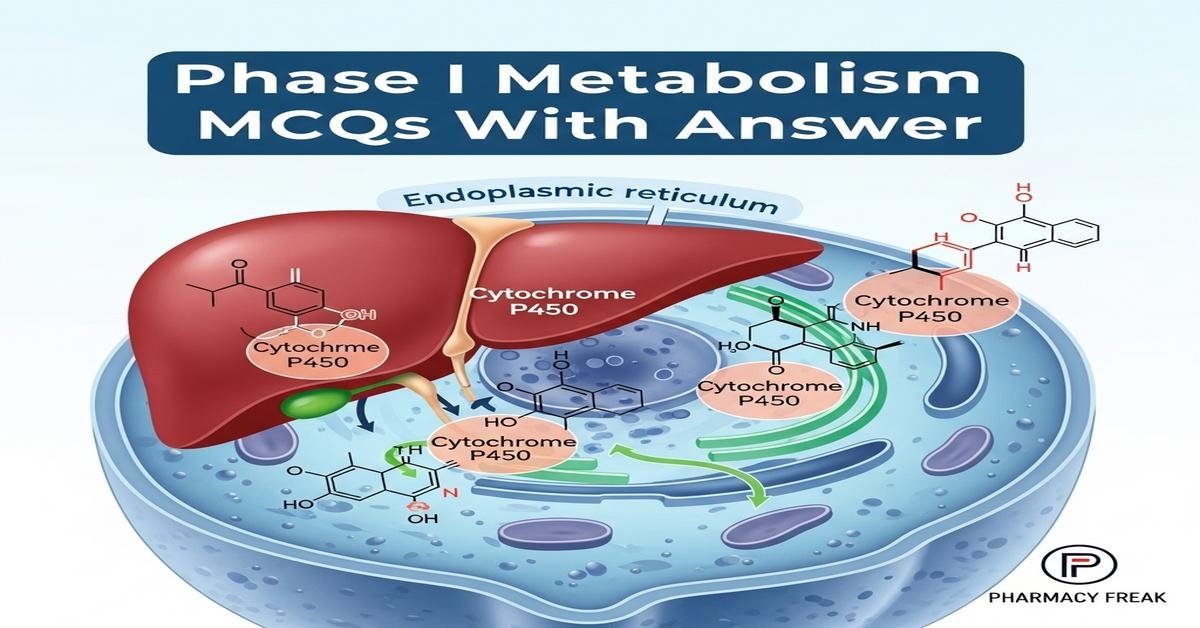
Phase I metabolism MCQs With Answer
Phase I metabolism is a key topic for B. Pharm students, covering enzymatic reactions that modify drugs via oxidation, reduction and hydrolysis. This introduction focuses on cytochrome P450s, flavin monooxygenases, esterases, and key concepts such as regioselectivity, stereoselectivity, bioactivation, enzyme kinetics, inhibitors and polymorphisms. These Phase I metabolism MCQs With Answer help reinforce mechanisms, clinical implications, experimental models and drug–drug interactions important for pharmacokinetics and drug safety. Clear explanations and targeted practice improve exam readiness and practical understanding of metabolic pathways. Now let’s test your knowledge with 50 MCQs on this topic.
Q1. Which enzyme family is primarily responsible for oxidative Phase I drug metabolism in the liver?
- Uridine diphosphate glucuronosyltransferases
- Cytochrome P450 monooxygenases
- Glutathione S-transferases
- N-acetyltransferases
Correct Answer: Cytochrome P450 monooxygenases
Q2. Which cofactor is essential for cytochrome P450 catalytic activity?
- ATP
- NADPH
- CoA
- UDP-glucuronic acid
Correct Answer: NADPH
Q3. Which Phase I reaction converts an ester into an alcohol and a carboxylic acid?
- N-dealkylation
- Hydrolysis
- Oxidative deamination
- Sulfoxidation
Correct Answer: Hydrolysis
Q4. Which CYP isoform is most often implicated in drug–drug interactions due to its high abundance and broad substrate specificity?
- CYP2D6
- CYP3A4
- CYP1A2
- CYP2E1
Correct Answer: CYP3A4
Q5. A drug showing first-pass metabolism primarily undergoes which process?
- Renal elimination before systemic circulation
- Metabolism in the gut wall and liver during absorption
- Direct conjugation in plasma
- Excretion via bile without modification
Correct Answer: Metabolism in the gut wall and liver during absorption
Q6. Which Phase I reaction introduces an oxygen atom into a substrate, often forming a hydroxyl group?
- Dehydrogenation
- Hydroxylation
- Nitration
- Acetylation
Correct Answer: Hydroxylation
Q7. Which term describes an enzyme that is permanently inactivated by forming a covalent bond with the enzyme during metabolism?
- Competitive inhibitor
- Mechanism-based (suicide) inhibitor
- Noncompetitive inhibitor
- Allosteric activator
Correct Answer: Mechanism-based (suicide) inhibitor
Q8. Which experimental system best preserves cellular architecture and phase I plus phase II capacity for in vitro metabolism studies?
- Recombinant CYP microsomes
- Human liver microsomes
- Primary human hepatocytes
- Bacterial expression systems
Correct Answer: Primary human hepatocytes
Q9. What is the primary reactive metabolite formed from acetaminophen responsible for hepatotoxicity?
- NAPQI (N-acetyl-p-benzoquinone imine)
- Glutathione conjugate
- Acetylated metabolite
- Hydroxy-acetaminophen
Correct Answer: NAPQI (N-acetyl-p-benzoquinone imine)
Q10. Which Phase I reaction commonly leads to increased water solubility by converting lipophilic groups to polar groups?
- Oxidation
- Glucuronidation
- Sulfation
- Methylation
Correct Answer: Oxidation
Q11. CYP2D6 polymorphism often results in which clinical consequence?
- Uniform metabolism in all populations
- Variable metabolism leading to poor or ultra-rapid metabolizer phenotypes
- Enhanced glucuronidation only
- No impact on drug clearance
Correct Answer: Variable metabolism leading to poor or ultra-rapid metabolizer phenotypes
Q12. Which assay is commonly used to assess CYP activity using known probe substrates?
- ELISA for albumin
- Probe substrate assay with LC-MS detection
- Immunohistochemistry
- Genomic PCR for transporter genes
Correct Answer: Probe substrate assay with LC-MS detection
Q13. Flavin-containing monooxygenases (FMOs) mainly catalyze which type of reaction?
- N- and S-oxidation of nucleophilic heteroatoms
- Glucuronidation of phenols
- Peptide bond hydrolysis
- Reductive dehalogenation
Correct Answer: N- and S-oxidation of nucleophilic heteroatoms
Q14. Which parameter represents the substrate concentration at which reaction velocity is half of Vmax in Michaelis–Menten kinetics?
- kcat
- Km
- CLint
- IC50
Correct Answer: Km
Q15. Which metabolic reaction often results in removal of a methyl or alkyl group attached to nitrogen or oxygen?
- Dealkylation
- Decarboxylation
- Conjugation
- Oxidative coupling
Correct Answer: Dealkylation
Q16. Which of the following is a common non-P450 Phase I enzyme involved in alcohol metabolism?
- Monoamine oxidase
- Alcohol dehydrogenase
- Thiopurine methyltransferase
- UDP-glucuronosyltransferase
Correct Answer: Alcohol dehydrogenase
Q17. Grapefruit juice primarily affects which metabolic process?
- Induction of renal transporters
- Inhibition of intestinal CYP3A4 and P-gp leading to increased bioavailability
- Activation of hepatic glucuronidation
- Enhancement of biliary excretion
Correct Answer: Inhibition of intestinal CYP3A4 and P-gp leading to increased bioavailability
Q18. Which term describes the creation of a more reactive intermediate that can bind to macromolecules and cause toxicity?
- Detoxification
- Bioactivation
- Conjugation
- Elimination
Correct Answer: Bioactivation
Q19. Which of the following is NOT a typical Phase I metabolic reaction?
- Hydroxylation
- Oxidation
- Glucuronidation
- Reduction
Correct Answer: Glucuronidation
Q20. Which substrate preference differentiates CYP2C9 from CYP2C19?
- CYP2C9 prefers acidic drugs while CYP2C19 prefers basic drugs
- CYP2C9 metabolizes only steroids while CYP2C19 does not
- Both have identical substrate specificity
- CYP2C19 exclusively metabolizes peptides
Correct Answer: CYP2C9 prefers acidic drugs while CYP2C19 prefers basic drugs
Q21. Which experimental preparation is enriched for ER-bound CYP enzymes and used in many in vitro metabolism studies?
- Plasma fractions
- Microsomes
- Crude mitochondrial pellets
- Nuclear extracts
Correct Answer: Microsomes
Q22. Which clinical strategy can reduce formation of a toxic reactive metabolite from a drug?
- Co-administration with enzyme inducers
- Co-administration with inhibitors of the bioactivating enzyme
- Increasing drug dose
- Administering drug via inhalation exclusively
Correct Answer: Co-administration with inhibitors of the bioactivating enzyme
Q23. Stereoselective metabolism leads to which phenomenon?
- Both enantiomers are metabolized equally
- Different enantiomers are metabolized at different rates producing different pharmacokinetics
- Stereochemistry never affects metabolism
- Only racemic mixtures are metabolized
Correct Answer: Different enantiomers are metabolized at different rates producing different pharmacokinetics
Q24. Which is a common clinical consequence of CYP inhibition by a co-administered drug?
- Decreased plasma levels of the substrate drug
- No change in drug exposure
- Increased plasma levels of the substrate drug and potential toxicity
- Immediate renal elimination of the substrate
Correct Answer: Increased plasma levels of the substrate drug and potential toxicity
Q25. Which enzyme catalyzes deamination of monoamines and is important for neurotransmitter metabolism rather than typical drug Phase I metabolism?
- Monoamine oxidase (MAO)
- Cytochrome P450 3A4
- UDP-glucuronosyltransferase
- Glutathione S-transferase
Correct Answer: Monoamine oxidase (MAO)
Q26. Which factor most influences intrinsic clearance (CLint) of a drug in vitro?
- Plasma protein binding only
- Enzyme concentration and substrate affinity (Vmax and Km)
- Drug taste
- Route of administration
Correct Answer: Enzyme concentration and substrate affinity (Vmax and Km)
Q27. Which reaction type is catalyzed by aldehyde dehydrogenase in ethanol metabolism?
- Oxidation of acetaldehyde to acetate
- Hydrolysis of ester bonds
- Conjugation to glucuronic acid
- Reduction of ketones
Correct Answer: Oxidation of acetaldehyde to acetate
Q28. Which statement best describes noncompetitive inhibition of a Phase I enzyme?
- Inhibitor competes with substrate for the active site raising Km
- Inhibitor binds a separate site decreasing Vmax without changing Km
- Inhibitor is converted to a product by the enzyme
- Inhibition can be overcome by increasing substrate concentration
Correct Answer: Inhibitor binds a separate site decreasing Vmax without changing Km
Q29. Epoxidation of aromatic compounds by CYP enzymes can lead to which result?
- Formation of stable, nonreactive metabolites only
- Formation of reactive epoxide intermediates that can bind DNA or proteins
- Immediate conjugation to sulfate in plasma
- Reduction to alcohols exclusively
Correct Answer: Formation of reactive epoxide intermediates that can bind DNA or proteins
Q30. Which substrate would most likely undergo N-oxidation rather than O-dealkylation?
- Aliphatic alcohol
- Tertiary aromatic amine
- Simple ether
- Carboxylic acid
Correct Answer: Tertiary aromatic amine
Q31. Which CYP isoform is predominantly involved in metabolism of codeine to morphine?
- CYP3A4
- CYP2D6
- CYP1A2
- CYP2E1
Correct Answer: CYP2D6
Q32. What is the significance of regioselectivity in Phase I metabolism?
- It determines the organ of excretion
- It determines which position on a molecule is metabolized, influencing activity and toxicity
- It only applies to Phase II reactions
- It dictates protein binding in plasma
Correct Answer: It determines which position on a molecule is metabolized, influencing activity and toxicity
Q33. Which method helps predict human hepatic clearance from in vitro microsomal data?
- Allometric scaling without metabolism data
- In vitro–in vivo extrapolation (IVIVE) using CLint and scaling factors
- Measuring taste and solubility only
- Clinical trials without preclinical studies
Correct Answer: In vitro–in vivo extrapolation (IVIVE) using CLint and scaling factors
Q34. Which Phase I enzyme is important for reducing nitro groups to amines under certain conditions?
- Nitroreductase
- CYP3A4
- UDP-glucuronosyltransferase
- Carboxylesterase
Correct Answer: Nitroreductase
Q35. Which of the following increases drug metabolism by inducing CYP enzymes?
- Rifampicin
- Ketoconazole
- Fluoxetine
- Grapefruit juice
Correct Answer: Rifampicin
Q36. Which analytical technique is most commonly used to identify metabolites formed in Phase I reactions?
- Light microscopy
- Liquid chromatography–mass spectrometry (LC-MS)
- Urine dipstick test
- pH titration
Correct Answer: Liquid chromatography–mass spectrometry (LC-MS)
Q37. Which factor does NOT typically affect hepatic phase I metabolism?
- Genetic polymorphisms of enzymes
- Co-administered enzyme inducers/inhibitors
- Dietary factors such as grapefruit juice
- Ambient room lighting
Correct Answer: Ambient room lighting
Q38. Which Phase I reaction often precedes Phase II conjugation by introducing a functional group for conjugation?
- Hydroxylation
- Glucuronidation
- Sulfation
- Acetylation
Correct Answer: Hydroxylation
Q39. Which drug is a classic example of a prodrug activated by CYP-mediated oxidation?
- Propranolol
- Enalapril (activated to enalaprilat)
- Aspirin
- Metformin
Correct Answer: Enalapril (activated to enalaprilat)
Q40. Which type of inhibition can be overcome by increasing substrate concentration?
- Noncompetitive inhibition
- Irreversible inhibition
- Competitive inhibition
- Mechanism-based inhibition
Correct Answer: Competitive inhibition
Q41. A drug metabolized primarily by CYP2C9 could show increased plasma concentration with co-administration of which inhibitor?
- Fluconazole
- Carbamazepine
- Rifampicin
- St. John’s Wort
Correct Answer: Fluconazole
Q42. Which Phase I enzyme activity can be assessed using testosterone 6β-hydroxylation as a probe?
- CYP1A2
- CYP2D6
- CYP3A4
- CYP2E1
Correct Answer: CYP3A4
Q43. Which structural change typically reduces a drug’s activity through Phase I metabolism?
- Introduction of a hydrophobic alkyl chain
- Formation of a polar hydroxylated metabolite that decreases receptor binding
- Methylation increasing lipophilicity
- Conversion to a prodrug
Correct Answer: Formation of a polar hydroxylated metabolite that decreases receptor binding
Q44. Which clinical test can be used to phenotype CYP2D6 activity in a patient?
- Urinary cortisol measurement
- Administration of dextromethorphan and measuring metabolite ratios
- Fasting blood glucose test
- Serum creatinine clearance only
Correct Answer: Administration of dextromethorphan and measuring metabolite ratios
Q45. Which reaction is catalyzed by carboxylesterases in drug metabolism?
- Hydrolysis of esters to alcohols and acids
- N-oxidation of tertiary amines
- Oxidative deamination of amines
- Glutathione conjugation
Correct Answer: Hydrolysis of esters to alcohols and acids
Q46. Which metabolic pathway is most likely to be involved when a nitroaromatic drug becomes reduced under anaerobic conditions in the gut?
- Oxidative demethylation in the liver
- Reduction by gut microbial enzymes
- Glucuronidation in plasma
- Sulfation in kidney
Correct Answer: Reduction by gut microbial enzymes
Q47. Which descriptor indicates the rate of product formation per enzyme active site under saturated substrate conditions?
- Km
- kcat
- IC50
- CLr
Correct Answer: kcat
Q48. Which is a limitation of using recombinant single CYP enzymes for metabolism studies?
- They perfectly replicate hepatic cofactor and protein interactions
- They lack the full complement of hepatic enzymes and cellular context influencing metabolism
- They are identical to primary hepatocytes in all aspects
- They cannot be used to study specific CYP isoforms
Correct Answer: They lack the full complement of hepatic enzymes and cellular context influencing metabolism
Q49. Which Phase I change would most likely increase a drug’s susceptibility to Phase II glucuronidation?
- Removal of hydroxyl groups
- Formation of polar groups like hydroxyl or carboxyl
- Methylation of phenolic OH
- Conversion to a more lipophilic form
Correct Answer: Formation of polar groups like hydroxyl or carboxyl
Q50. Which approach helps reduce variability in drug metabolism caused by genetic polymorphisms in a clinical setting?
- Ignoring genotype information
- Therapeutic drug monitoring and dose adjustment based on phenotype/genotype
- Prescribing standard doses for all patients
- Avoiding all drugs metabolized by CYP enzymes
Correct Answer: Therapeutic drug monitoring and dose adjustment based on phenotype/genotype

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com