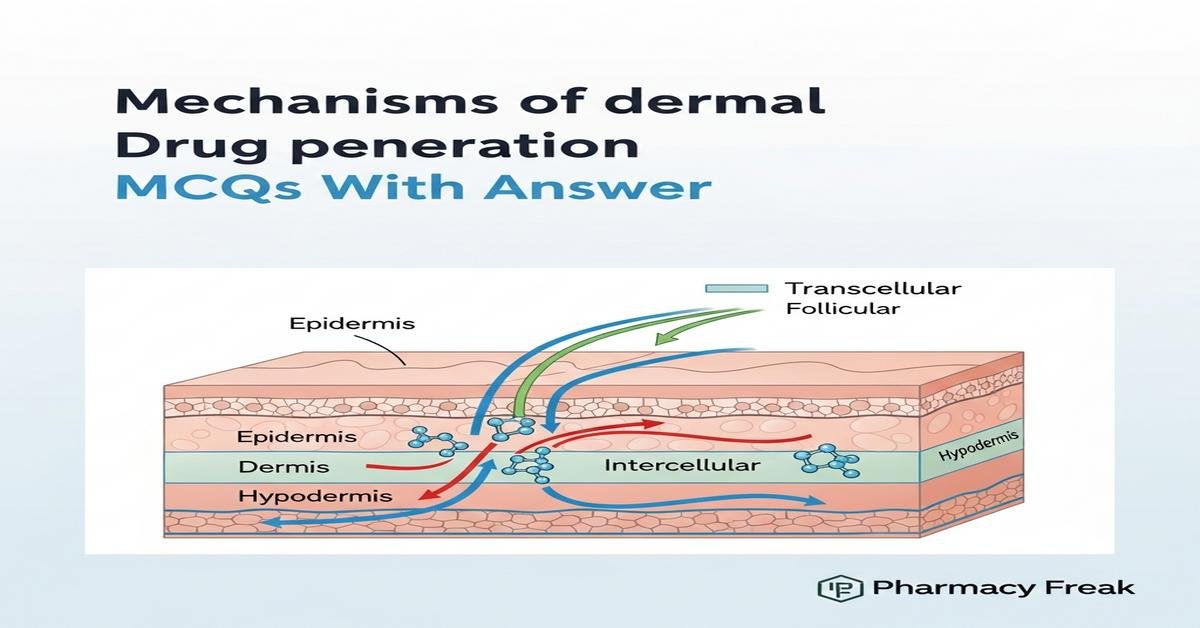
Understanding mechanisms of dermal drug penetration is essential for B.Pharm students designing topical and transdermal therapies. This concise overview covers major penetration routes (transcellular, intercellular, appendageal), the barrier role of the stratum corneum, and key determinants of percutaneous absorption such as partition coefficient, diffusion coefficient, molecular size, thermodynamic activity, vehicle effects, hydration and skin metabolism. It also introduces enhancement strategies—chemical enhancers, prodrugs, microneedles, iontophoresis and nanoformulations (liposomes, solid lipid nanoparticles)—plus practical tools like Fick’s law, permeability coefficient, lag time and Franz diffusion cells for evaluation. Now let’s test your knowledge with 30 MCQs on this topic.
Q1. Which skin layer provides the principal barrier to dermal drug penetration?
- Stratum corneum
- Viable epidermis
- Dermis
- Hypodermis
Correct Answer: Stratum corneum
Q2. Which set correctly lists the primary anatomical routes for drug passage across the skin?
- Intercellular, transcellular and appendageal routes
- Transendothelial, paracellular and follicular routes
- Endocytic, exocytic and transcytotic routes
- Vascular, lymphatic and neural routes
Correct Answer: Intercellular, transcellular and appendageal routes
Q3. Fick’s first law of diffusion at steady state states that flux (J) is directly proportional to which of the following?
- Diffusion coefficient and concentration gradient
- Molecular weight and skin thickness
- Partition coefficient and lag time
- Vehicle viscosity and occlusion time
Correct Answer: Diffusion coefficient and concentration gradient
Q4. The permeability coefficient (P) for skin is best expressed by which relationship?
- P = (K × D) / h
- P = (h × D) / K
- P = K / (D × h)
- P = D / (K × h)
Correct Answer: P = (K × D) / h
Q5. For optimal transdermal delivery, the ideal octanol/water partition coefficient (LogP) of a drug is generally considered to be:
- Less than 0 (very hydrophilic)
- Around 1–3 (balanced lipophilicity)
- Greater than 6 (very lipophilic)
- Irrelevant for skin permeation
Correct Answer: Around 1–3 (balanced lipophilicity)
Q6. A commonly cited molecular weight threshold above which skin permeation becomes very limited is approximately:
- 100 Da
- 250 Da
- 500 Da
- 1000 Da
Correct Answer: 500 Da
Q7. Which term best describes the true driving force for passive dermal permeation of a drug?
- Thermodynamic activity of the drug
- Absolute drug concentration in the vehicle
- Vehicle viscosity
- Application area size
Correct Answer: Thermodynamic activity of the drug
Q8. How does skin hydration generally affect stratum corneum permeability?
- Hydration increases permeability by swelling corneocytes and fluidizing lipids
- Hydration decreases permeability by tightening lipid packing
- Hydration has no effect on permeability
- Hydration only affects hair follicles, not the stratum corneum
Correct Answer: Hydration increases permeability by swelling corneocytes and fluidizing lipids
Q9. Chemical penetration enhancers primarily act by which mechanism?
- Disrupting stratum corneum lipids and increasing drug partitioning/diffusion
- Blocking skin enzymes to prevent metabolism
- Forming irreversible covalent bonds with keratin
- Increasing blood flow in the dermis only
Correct Answer: Disrupting stratum corneum lipids and increasing drug partitioning/diffusion
Q10. Iontophoresis enhances transdermal delivery by which physical principle?
- Application of low electrical current to drive charged molecules
- Use of high-frequency ultrasound to create cavitation
- Thermal heating to increase skin temperature
- Mechanical abrasion of the stratum corneum
Correct Answer: Application of low electrical current to drive charged molecules
Q11. Which in vitro apparatus is most widely used to measure percutaneous absorption and steady-state flux?
- Franz diffusion cell
- Rotating basket dissolution tester
- Parallel plate viscometer
- High-performance liquid chromatography system
Correct Answer: Franz diffusion cell
Q12. What does the ‘lag time’ in skin permeation studies represent?
- Time required to reach steady-state flux across the skin
- Time before the formulation dries on skin
- Time taken for systemic clearance after absorption
- Time for drug synthesis in the formulation
Correct Answer: Time required to reach steady-state flux across the skin
Q13. Activation of topical prodrugs in the skin commonly relies on which enzyme class?
- Esterases
- Monoamine oxidases
- Amylases
- Lipoxygenases
Correct Answer: Esterases
Q14. Occlusive dressings enhance transdermal delivery primarily by which effect?
- Reducing transepidermal water loss and increasing stratum corneum hydration
- Increasing dermal blood flow directly
- Inactivating skin esterases
- Increasing drug molecular weight
Correct Answer: Reducing transepidermal water loss and increasing stratum corneum hydration
Q15. The formulation vehicle influences dermal absorption mainly by altering which factors?
- Drug thermodynamic activity and partitioning into skin
- Skin thickness and hair follicle density
- Systemic renal clearance of the drug
- Ambient humidity only
Correct Answer: Drug thermodynamic activity and partitioning into skin
Q16. Tape-stripping is a technique used in dermal studies to:
- Sequentially remove layers of stratum corneum to study penetration depth
- Measure transdermal electrical resistance only
- Deliver drugs via microporation
- Quantify dermal blood flow
Correct Answer: Sequentially remove layers of stratum corneum to study penetration depth
Q17. What is meant by the ‘skin reservoir’ effect?
- Accumulation of drug within skin layers that releases slowly over time
- Storage of drugs in subcutaneous fat exclusively
- Permanent binding of all drug to epidermal proteins
- Immediate systemic elimination after topical application
Correct Answer: Accumulation of drug within skin layers that releases slowly over time
Q18. The appendageal (shunt) route includes which structures that can facilitate penetration of larger or hydrophilic molecules?
- Hair follicles and sweat glands
- Dermal capillaries and lymphatics
- Subcutaneous adipocytes and muscle fibers
- Corneocyte envelopes only
Correct Answer: Hair follicles and sweat glands
Q19. Liposomal formulations can enhance dermal delivery primarily by:
- Serving as carriers that interact with epidermal lipids and increase drug solubility
- Raising drug molecular weight to prevent permeation
- Blocking follicular uptake exclusively
- Neutralizing skin pH permanently
Correct Answer: Serving as carriers that interact with epidermal lipids and increase drug solubility
Q20. Sonophoresis (ultrasound-enhanced delivery) increases skin permeability mainly through:
- Cavitation and mechanical disruption of stratum corneum lipids
- Generation of an electric field to move ions
- Formation of permanent pores in capillaries
- Neutralizing chemical enhancers
Correct Answer: Cavitation and mechanical disruption of stratum corneum lipids
Q21. Which of the following are common chemical penetration enhancers?
- Terpenes, fatty acids and surfactants
- Anticoagulants and beta-blockers
- Antibiotics only
- Neutral pH buffers exclusively
Correct Answer: Terpenes, fatty acids and surfactants
Q22. The term that denotes the mass of drug crossing unit area of skin per unit time is:
- Flux
- Lag time
- Partition coefficient
- Viscosity
Correct Answer: Flux
Q23. In skin permeation, the partition coefficient (K) commonly refers to the ratio of drug concentration between which phases?
- Stratum corneum lipids and vehicle
- Blood plasma and urine
- Dermis and hypodermis
- Hair shaft and sweat
Correct Answer: Stratum corneum lipids and vehicle
Q24. Which advantage is commonly attributed to solid lipid nanoparticles (SLNs) for topical delivery?
- Controlled release and improved chemical stability of lipophilic drugs
- Immediate systemic absorption without skin retention
- Complete inhibition of skin enzymes
- Guaranteed enhancement of hydrophilic drug permeation
Correct Answer: Controlled release and improved chemical stability of lipophilic drugs
Q25. A prodrug strategy for dermal delivery is often used to:
- Increase drug lipophilicity to improve skin permeation and then be converted in skin
- Decrease drug potency to reduce side effects systemically
- Enhance transdermal delivery by increasing molecular weight only
- Prevent any metabolic conversion in the skin
Correct Answer: Increase drug lipophilicity to improve skin permeation and then be converted in skin
Q26. How does the degree of ionization of a drug affect its dermal permeation?
- Unionized form permeates skin more readily than ionized form
- Ionized form always permeates better than unionized form
- Ionization has no effect on permeation
- Only basic drugs are affected by ionization
Correct Answer: Unionized form permeates skin more readily than ionized form
Q27. Increasing skin temperature typically affects dermal absorption by:
- Increasing diffusion coefficients and thereby permeability
- Decreasing drug solubility in the vehicle only
- Lowering thermodynamic activity of the drug
- Reducing blood flow in the dermis
Correct Answer: Increasing diffusion coefficients and thereby permeability
Q28. Microneedles enhance delivery by which principal mechanism?
- By physically bypassing the stratum corneum to create microchannels for drug entry
- By chemically dissolving corneocytes without creating channels
- By producing a sustained electrical field across the skin
- By increasing epidermal enzymatic activity
Correct Answer: By physically bypassing the stratum corneum to create microchannels for drug entry
Q29. Surfactants act as penetration enhancers primarily because they:
- Solubilize and extract lipids from the stratum corneum, disrupting barrier structure
- Form a rigid film that blocks diffusion
- Convert drugs into large micellar complexes that cannot permeate
- Reduce skin hydration permanently
Correct Answer: Solubilize and extract lipids from the stratum corneum, disrupting barrier structure
Q30. The SI units typically used for permeability coefficient (P) in skin permeation studies are:
- cm/s
- mg/mL
- mm Hg
- mol/kg
Correct Answer: cm/s

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com