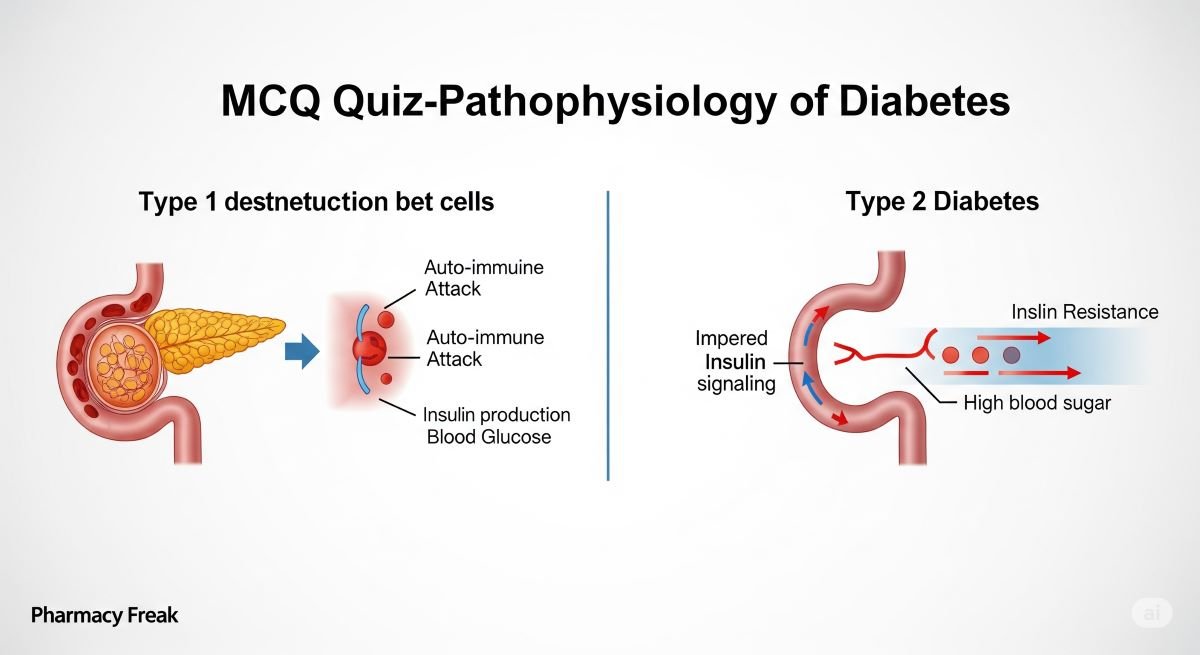
Diabetes mellitus is a group of metabolic disorders defined by hyperglycemia, resulting from defects in insulin secretion, insulin action, or both. Understanding the distinct pathophysiology of Type 1 versus Type 2 diabetes, a core topic in the Patient Care 5 curriculum, is fundamental to selecting appropriate therapy and managing long-term complications. This quiz will test your knowledge on the intricate mechanisms of the disease, from autoimmune beta-cell destruction to the complex interplay of insulin resistance and the development of micro- and macrovascular disease.
1. Which of the following best describes the core pathophysiologic defect in Type 1 Diabetes?
- a. Severe peripheral insulin resistance.
- b. Autoimmune destruction of pancreatic beta cells, leading to absolute insulin deficiency.
- c. Overproduction of glucagon by alpha cells.
- d. A progressive decline in insulin secretion over many years.
Answer: b. Autoimmune destruction of pancreatic beta cells, leading to absolute insulin deficiency.
2. In Type 2 Diabetes, the two primary pathophysiologic defects are:
- a. Absolute insulin deficiency and excessive glucagon secretion.
- b. Autoimmune destruction of beta cells and insulin resistance.
- c. Insulin resistance and a progressive decline in beta-cell function.
- d. Decreased hepatic glucose production and increased glucose uptake by muscle.
Answer: c. Insulin resistance and a progressive decline in beta-cell function.
3. Which hormone is secreted by pancreatic alpha cells in response to low blood glucose?
- a. Insulin
- b. Amylin
- c. Glucagon
- d. Somatostatin
Answer: c. Glucagon
4. The “incretin effect” refers to the enhanced insulin secretion that occurs in response to an oral glucose load compared to an IV glucose infusion. This effect is primarily mediated by:
- a. GLP-1 and GIP
- b. Epinephrine and norepinephrine
- c. Cortisol
- d. Aldosterone
Answer: a. GLP-1 and GIP
5. How is the incretin effect altered in patients with Type 2 Diabetes?
- a. It is exaggerated, leading to hypoglycemia.
- b. It is blunted or diminished, contributing to hyperglycemia.
- c. It remains unchanged.
- d. It only affects glucagon secretion.
Answer: b. It is blunted or diminished, contributing to hyperglycemia.
6. The “Pathophysiology and Management of Diabetes” is a specific learning module in which course?
- a. PHA5787C Patient Care 5
- b. PHA5104 Sterile Compounding
- c. PHA5703 Pharmacy Law and Ethics
- d. PHA5878C Patient Care 3
Answer: a. PHA5787C Patient Care 5
7. Diabetic Ketoacidosis (DKA) is characterized by hyperglycemia, ketosis, and what other key finding?
- a. Metabolic alkalosis
- b. Metabolic acidosis
- c. Respiratory acidosis
- d. Normal blood pH
Answer: b. Metabolic acidosis
8. The development of ketones in DKA is a direct result of:
- a. Excessive carbohydrate intake.
- b. Uncontrolled lipolysis (breakdown of fat) due to absolute insulin deficiency.
- c. Overproduction of glucose by the liver.
- c. Severe dehydration.
Answer: b. Uncontrolled lipolysis (breakdown of fat) due to absolute insulin deficiency.
9. Insulin resistance is defined as:
- a. The complete absence of insulin production.
- b. An allergic reaction to insulin.
- c. A decreased response of peripheral tissues (muscle, fat, liver) to the actions of insulin.
- d. The rapid degradation of insulin in the bloodstream.
Answer: c. A decreased response of peripheral tissues (muscle, fat, liver) to the actions of insulin.
10. In a state of insulin resistance, the liver’s response is to:
- a. Decrease its production of glucose.
- b. Increase its storage of glucose as glycogen.
- c. Continue to produce glucose (gluconeogenesis) even when blood glucose is high.
- d. Shut down completely.
Answer: c. Continue to produce glucose (gluconeogenesis) even when blood glucose is high.
11. The management of diabetes is a topic within the Patient Care 5 curriculum.
- a. True
- b. False
Answer: a. True
12. The pathophysiology of diabetic nephropathy involves which of the following initial changes?
- a. A decrease in glomerular filtration rate (GFR).
- b. Glomerular hyperfiltration and increased intraglomerular pressure.
- c. The formation of kidney stones.
- d. A reduction in the size of the kidneys.
Answer: b. Glomerular hyperfiltration and increased intraglomerular pressure.
13. The presence of what in the urine is the earliest clinical sign of diabetic nephropathy?
- a. Glucose
- b. Ketones
- c. White blood cells
- d. Microalbuminuria
Answer: d. Microalbuminuria
14. Hyperglycemia contributes to macrovascular complications (like atherosclerosis) by:
- a. Causing endothelial dysfunction.
- b. Promoting a pro-inflammatory state.
- c. Creating advanced glycation end-products (AGEs).
- d. All of the above.
Answer: d. All of the above.
15. Hyperosmolar Hyperglycemic State (HHS) differs from DKA in that HHS is characterized by:
- a. More severe ketoacidosis.
- b. Extreme hyperglycemia and severe dehydration, with minimal or no ketoacidosis.
- c. Lower blood glucose levels.
- d. Its occurrence primarily in Type 1 Diabetes.
Answer: b. Extreme hyperglycemia and severe dehydration, with minimal or no ketoacidosis.
16. Which of the following is NOT a microvascular complication of diabetes?
- a. Retinopathy
- b. Nephropathy
- c. Neuropathy
- d. Peripheral artery disease
Answer: d. Peripheral artery disease
17. The pharmacology of oral and injectable diabetes medications is a topic in the Patient Care 5 curriculum.
- a. True
- b. False
Answer: a. True
18. What is the primary role of insulin in muscle and adipose tissue?
- a. To stimulate the breakdown of glycogen.
- b. To promote the uptake and utilization of glucose.
- c. To increase the production of glucose.
- d. To inhibit the action of glucagon.
Answer: b. To promote the uptake and utilization of glucose.
19. In the early stages of Type 2 Diabetes, beta-cells compensate for insulin resistance by:
- a. Undergoing apoptosis.
- b. Decreasing insulin production.
- c. Increasing insulin production (hyperinsulinemia).
- d. Converting into alpha cells.
Answer: c. Increasing insulin production (hyperinsulinemia).
20. An active learning session on diabetes is part of the Patient Care 5 course.
- a. True
- b. False
Answer: a. True
21. Kussmaul respirations (deep, rapid breathing) in a patient with DKA is a compensatory mechanism for:
- a. Respiratory acidosis
- b. Hypoglycemia
- c. Metabolic acidosis
- d. Metabolic alkalosis
Answer: c. Metabolic acidosis
22. Which of the following pathways contributes to the pathophysiology of diabetic neuropathy?
- a. The polyol pathway (conversion of glucose to sorbitol).
- b. The formation of advanced glycation end-products (AGEs).
- c. Oxidative stress.
- d. All of the above.
Answer: d. All of the above.
23. The “fruity” odor on the breath of a patient with DKA is caused by:
- a. The breakdown of protein.
- b. High levels of glucose.
- c. The exhalation of acetone, a type of ketone.
- d. Poor oral hygiene.
Answer: c. The exhalation of acetone, a type of ketone.
24. The introduction to diabetes is a lecture within the Patient Care 5 curriculum.
- a. True
- b. False
Answer: a. True
25. A key difference between Type 1 and Type 2 diabetes is that patients with Type 1 are:
- a. Always diagnosed in old age.
- b. Always overweight or obese.
- c. Prone to ketoacidosis if insulin is withheld.
- d. Able to be managed with diet alone.
Answer: c. Prone to ketoacidosis if insulin is withheld.
26. The pathophysiology of non-proliferative diabetic retinopathy involves:
- a. The growth of new, fragile blood vessels on the retina.
- b. Damage to existing retinal capillaries, leading to microaneurysms and hemorrhages.
- c. A detachment of the retina.
- d. The development of cataracts.
Answer: b. Damage to existing retinal capillaries, leading to microaneurysms and hemorrhages.
27. The progressive nature of Type 2 Diabetes means that:
- a. Most patients will eventually be cured.
- b. Most patients will eventually require combination therapy or insulin as beta-cell function declines over time.
- c. The disease gets easier to manage over time.
- d. Complications will not occur if A1c is <8.0%.
Answer: b. Most patients will eventually require combination therapy or insulin as beta-cell function declines over time.
28. An active learning session on diabetes is part of which course?
- a. PHA5787C Patient Care 5
- b. PHA5163L Professional Skills Lab 3
- c. PHA5781 Patient Care I
- d. PHA5782C Patient Care 2
Answer: a. PHA5787C Patient Care 5
29. Glucagon’s primary site of action is the:
- a. Muscle
- b. Adipose tissue
- c. Liver
- d. Brain
Answer: c. Liver
30. Which of the following is NOT a classic symptom of new-onset Type 1 Diabetes?
- a. Polyuria (frequent urination)
- b. Polydipsia (excessive thirst)
- c. Unexplained weight gain
- d. Polyphagia (excessive hunger)
Answer: c. Unexplained weight gain
31. The term “glucotoxicity” refers to:
- a. The toxic effects of low blood sugar on cells.
- b. The direct damage that chronic hyperglycemia can cause to various cells, including beta cells.
- c. A side effect of metformin.
- d. An allergic reaction to glucagon.
Answer: b. The direct damage that chronic hyperglycemia can cause to various cells, including beta cells.
32. The management of diabetes complications is a topic within the Patient Care 5 curriculum.
- a. True
- b. False
Answer: a. True
33. The development of insulin resistance is strongly linked to:
- a. A low-fat diet.
- b. Regular aerobic exercise.
- c. Central or visceral obesity.
- d. A history of Type 1 Diabetes.
Answer: c. Central or visceral obesity.
34. The role of the GLUT4 transporter is to:
- a. Transport glucose out of the liver.
- b. Facilitate insulin-mediated glucose uptake into muscle and fat cells.
- c. Absorb glucose from the gut.
- d. Reabsorb glucose in the kidney.
Answer: b. Facilitate insulin-mediated glucose uptake into muscle and fat cells.
35. A key pathophysiologic link between diabetes and hypertension is:
- a. The effect of insulin resistance on sodium retention and endothelial function.
- b. The fact that all diabetes medications cause hypertension.
- c. The fact that all hypertension medications cause diabetes.
- d. There is no link between the two conditions.
Answer: a. The effect of insulin resistance on sodium retention and endothelial function.
36. The pathophysiology of diabetic gastroparesis involves:
- a. An overactive stomach.
- b. Damage to the vagus nerve, leading to delayed gastric emptying.
- c. Excessive acid production.
- d. The formation of ulcers.
Answer: b. Damage to the vagus nerve, leading to delayed gastric emptying.
37. In a patient without diabetes, insulin secretion is:
- a. Constant throughout the day.
- b. Pulsatile, with a basal rate and mealtime boluses.
- c. Only secreted at night.
- d. Only secreted after exercise.
Answer: b. Pulsatile, with a basal rate and mealtime boluses.
38. The medicinal chemistry of diabetes medications is a topic within the Patient Care 5 curriculum.
- a. True
- b. False
Answer: a. True
39. Atherosclerotic cardiovascular disease (ASCVD) is considered what type of diabetic complication?
- a. Microvascular
- b. Macrovascular
- c. Neuropathic
- d. Retinopathic
Answer: b. Macrovascular
40. An active learning session covering diabetes is part of which course module?
- a. Module 1: Diabetes Mellitus
- b. Module 3: Women’s Health
- c. Module 4: Medication Safety
- d. Module 8: Men’s Health
Answer: a. Module 1: Diabetes Mellitus
41. The initial “honeymoon period” in Type 1 Diabetes refers to:
- a. The first year of marriage after diagnosis.
- b. A temporary phase after diagnosis where some residual beta-cell function remains, leading to lower insulin requirements.
- c. A period of perfect glycemic control.
- d. The time before any complications develop.
Answer: b. A temporary phase after diagnosis where some residual beta-cell function remains, leading to lower insulin requirements.
42. The pathophysiology of Type 2 Diabetes involves all of the following EXCEPT:
- a. Insulin resistance in the muscle.
- b. Increased glucose production by the liver.
- c. Progressive beta-cell failure.
- d. Autoimmune destruction of beta cells.
Answer: d. Autoimmune destruction of beta cells.
43. Why does polyuria occur in uncontrolled diabetes?
- a. Because the patient is drinking too much water.
- b. High blood glucose levels exceed the kidney’s ability to reabsorb glucose, leading to osmotic diuresis.
- c. The patient’s bladder is overactive.
- d. Insulin acts as a diuretic.
Answer: b. High blood glucose levels exceed the kidney’s ability to reabsorb glucose, leading to osmotic diuresis.
44. A patient’s A1c value reflects:
- a. The amount of glucose attached to hemoglobin over the lifespan of a red blood cell.
- b. Their blood glucose at a single point in time.
- c. Their insulin level.
- d. Their risk of developing Type 1 Diabetes.
Answer: a. The amount of glucose attached to hemoglobin over the lifespan of a red blood cell.
45. What is the role of amylin, a hormone co-secreted with insulin?
- a. It increases glucagon secretion.
- b. It slows gastric emptying and promotes satiety.
- c. It increases hepatic glucose production.
- d. It has no known role in glucose homeostasis.
Answer: b. It slows gastric emptying and promotes satiety.
46. In Type 1 Diabetes, amylin levels are:
- a. Elevated
- b. Normal
- c. Deficient, along with insulin.
- d. Unpredictable
Answer: c. Deficient, along with insulin.
47. The “Ominous Octet” describes eight distinct pathophysiological defects in:
- a. Type 1 Diabetes
- b. Type 2 Diabetes
- c. Gestational Diabetes
- d. Hypoglycemia
Answer: b. Type 2 Diabetes
48. An active learning session on diabetes is part of which course?
- a. PHA5787C Patient Care 5
- b. PHA5163L Professional Skills Lab 3
- c. PHA5781 Patient Care I
- d. PHA5782C Patient Care 2
Answer: a. PHA5787C Patient Care 5
49. The pathophysiology of HHS involves:
- a. Severe dehydration and extreme hyperglycemia.
- b. The presence of enough insulin to prevent ketosis but not enough to control glucose.
- c. A precipitating event, like an infection.
- d. All of the above.
Answer: d. All of the above.
50. The ultimate reason for a pharmacist to have a deep understanding of diabetes pathophysiology is to:
- a. Be able to recommend and manage therapies that target the specific underlying defects of the disease.
- b. Memorize the names of all diabetes medications.
- c. Pass the endocrinology exam.
- d. Impress physicians with their knowledge of the Krebs cycle.
Answer: a. Be able to recommend and manage therapies that target the specific underlying defects of the disease.

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com