Peripheral vascular diseases (PVDs) refer to disorders that affect blood circulation outside of the heart and brain, commonly involving the arteries and veins of the limbs. These conditions can result from atherosclerosis, vasospasm, thrombosis, or inflammatory vascular diseases. Treatment includes lifestyle modification, surgical intervention, and pharmacological therapy.
This blog from Pharmacy Freak focuses on the classification, clinical uses, drug of choice, adverse effects, and updated treatment strategies for peripheral vascular conditions.
Table of Contents
What is Peripheral Vascular Diseases
Peripheral vascular disease is a broad term for conditions causing obstruction, constriction, or inflammation in peripheral blood vessels, leading to impaired blood flow to the limbs or other organs. It includes conditions like atherosclerotic peripheral arterial disease, thromboangiitis obliterans (Buerger’s disease), Raynaud’s phenomenon, and venous insufficiency.
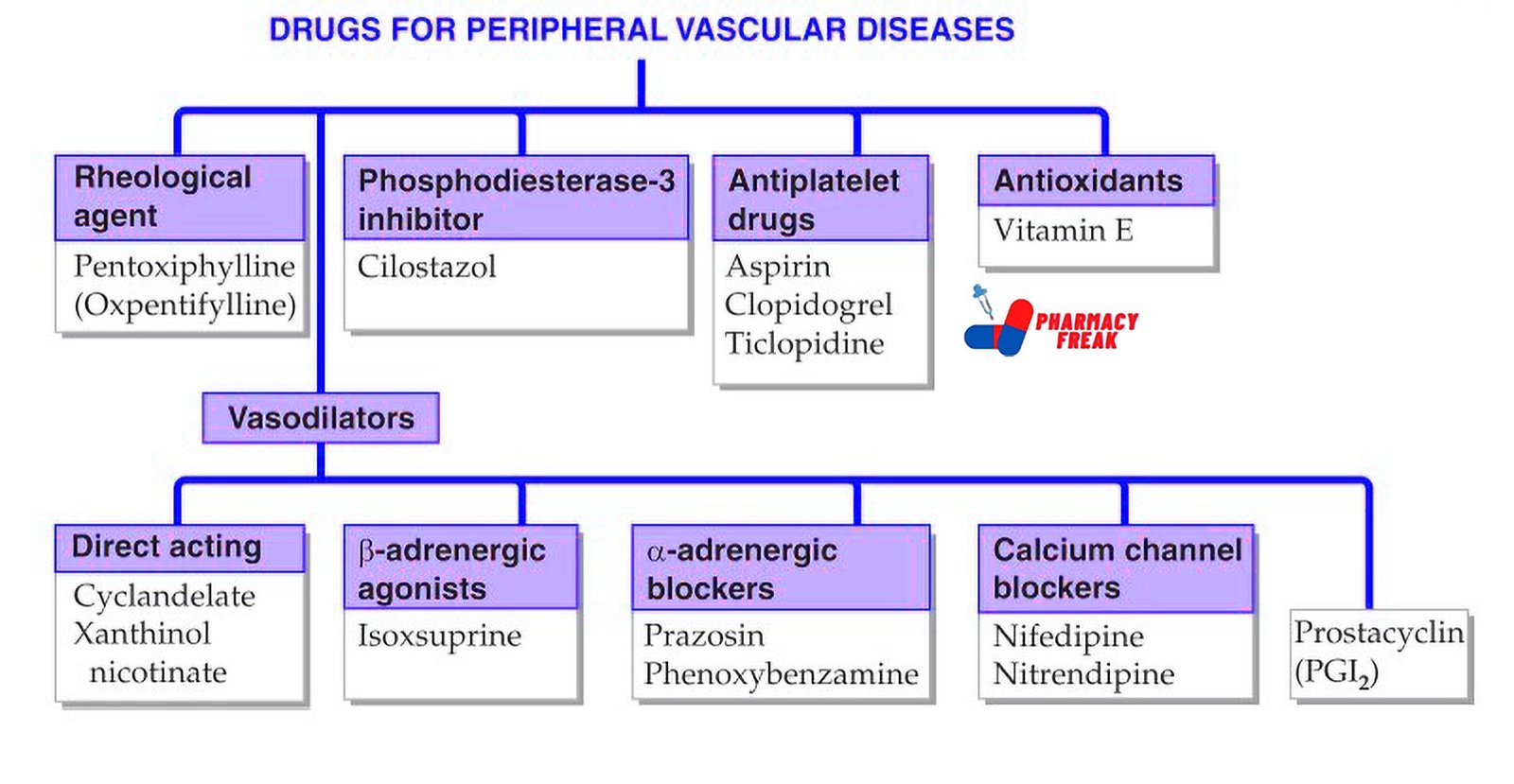
Classification of Drugs for Peripheral Vascular Diseases ( Tripathi)
- Rheological agent: Pentoxiphylline (Oxpentifylline)
- Phosphodiesterase-3 inhibitor: Cilostazol
- Antiplatelet drugs: Aspirin, Clopidogrel, Ticlopidine
- Antioxidants: Vitamin E
- Vasodilators –
- Direct acting: Cyclandelate, Xanthinol nicotinate
- β-adrenergic agonists: Isoxsuprine
- α-adrenergic blockers: Prazosin, Phenoxybenzamine
- Calcium channel blockers: Nifedipine, Nitrendipine
- Prostacyclin (PGI₂)
Classification (General)
Drugs used in PVDs are classified based on the mechanism and condition they target:
- Antiplatelet Drugs
Mechanism: Inhibit platelet aggregation to prevent arterial thrombosis
Examples: Aspirin, Clopidogrel, Cilostazol, Ticlopidine
Use: Atherosclerotic peripheral arterial disease, intermittent claudication
Note: Aspirin and Clopidogrel reduce the risk of cardiovascular events in PVD - Vasodilators
- a. Nitrates
Mechanism: Release nitric oxide, relax vascular smooth muscle
Example: Nitroglycerin
Use: Raynaud’s phenomenon, ischemic symptoms - b. Calcium Channel Blockers
Mechanism: Block calcium entry into vascular smooth muscle
Examples: Nifedipine, Amlodipine
Use: Raynaud’s disease and systemic sclerosis-related vasospasm - c. Phosphodiesterase III Inhibitors
Mechanism: Increase intracellular cAMP, vasodilation, and inhibition of platelet aggregation
Examples: Cilostazol
Use: Intermittent claudication in PAD
Note: Also has antiplatelet effects
- a. Nitrates
- Hemorheological Agents
Mechanism: Improve red blood cell flexibility and decrease blood viscosity
Examples: Pentoxifylline
Use: Intermittent claudication
Note: Less effective than Cilostazol - Anticoagulants
Mechanism: Inhibit clot formation by interfering with coagulation pathways
Examples: Heparin, Low Molecular Weight Heparins (Enoxaparin), Warfarin
Use: Acute limb ischemia, deep vein thrombosis (DVT), prevention of embolism - Fibrinolytics (Thrombolytics)
Mechanism: Promote dissolution of fibrin clots
Examples: Streptokinase, Urokinase, Alteplase (tPA)
Use: Acute arterial occlusion, pulmonary embolism - Endothelin Receptor Antagonists
Mechanism: Block endothelin-1, a potent vasoconstrictor
Example: Bosentan
Use: Pulmonary arterial hypertension, systemic sclerosis-associated Raynaud’s - Prostaglandin Analogues
Mechanism: Vasodilation and inhibition of platelet aggregation
Examples: Alprostadil, Iloprost
Use: Critical limb ischemia, Raynaud’s disease (intravenous use) - Statins
Mechanism: HMG-CoA reductase inhibitors; improve endothelial function and reduce atherosclerotic progression
Examples: Atorvastatin, Rosuvastatin
Use: PAD with coexisting dyslipidemia
Note: Improve walking distance in PAD patients
Uses
Drugs are used in PVD to achieve the following clinical goals:
- Relieve symptoms like claudication or vasospasm
- Prevent thrombosis and embolism
- Improve walking distance and quality of life
- Prevent progression to gangrene or ulceration
- Treat underlying conditions like atherosclerosis and hypertension
Drug of Choice Highlights
- Intermittent claudication – Cilostazol
- Buerger’s disease – Smoking cessation is essential; symptomatic relief with vasodilators
- Raynaud’s phenomenon – Nifedipine
- Critical limb ischemia – Prostaglandin analogues like Iloprost
- Acute arterial occlusion – Heparin (initial), followed by thrombolysis or surgery
- Pulmonary hypertension – Bosentan
- DVT prophylaxis – LMWH or Warfarin depending on setting
Side Effects
- Aspirin – Gastric irritation, bleeding, hypersensitivity
- Clopidogrel – Diarrhea, rash, neutropenia (rare)
- Cilostazol – Headache, palpitations, contraindicated in heart failure
- Pentoxifylline – Nausea, dizziness, flushing
- Calcium channel blockers – Edema, hypotension, headache
- Heparin – Bleeding, heparin-induced thrombocytopenia
- Warfarin – Bleeding, skin necrosis, teratogenicity
- Statins – Myopathy, elevated liver enzymes
- Bosentan – Hepatotoxicity, anemia
- Iloprost – Flushing, jaw pain, hypotension
Updated Clinical Pearls
- Cilostazol is more effective than Pentoxifylline in improving walking distance in intermittent claudication.
- Statins are indicated in all patients with peripheral artery disease, even if cholesterol is normal.
- Smoking cessation is the most critical intervention in thromboangiitis obliterans.
- In Raynaud’s phenomenon, cold avoidance and CCBs are the mainstay.
- In acute arterial occlusion, immediate anticoagulation with heparin is crucial to prevent thrombus propagation.
- Combination therapy with antiplatelet and vasodilators may be required in resistant cases.
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 875–877
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 308–310
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 1047–1052
Related Links
I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com