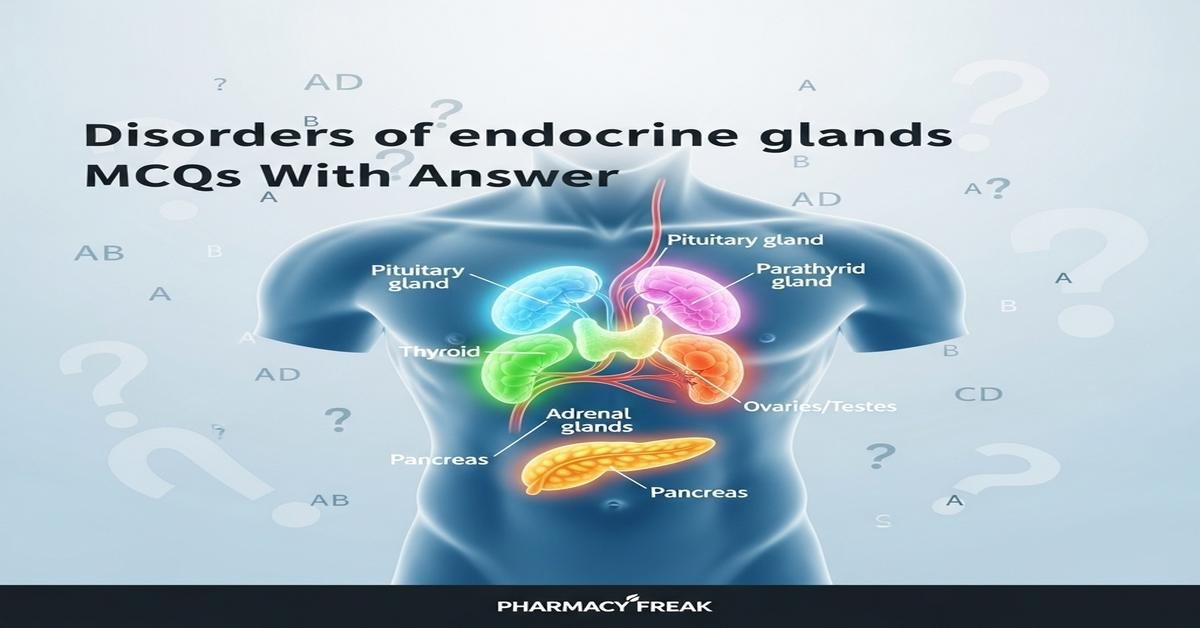
Introduction: Disorders of endocrine glands are central to pharmacology and therapeutics in the B.Pharm curriculum. This concise guide covers key endocrine disorders—thyroid, adrenal, pituitary, pancreatic and parathyroid diseases—focusing on pathophysiology, diagnostic tests, and evidence-based drug therapies. Emphasis is placed on hormones, receptor mechanisms, drug classes (insulins, oral antidiabetics, antithyroid agents, corticosteroids, somatostatin analogs, and mineralocorticoid replacements), adverse effects, and emergency management such as thyroid storm, diabetic ketoacidosis, and adrenal crisis. Targeted for B.Pharm students, these MCQs reinforce clinical reasoning and pharmacotherapeutic decision-making. Now let’s test your knowledge with 50 MCQs on this topic.
Q1. Which hormone is primarily responsible for increasing basal metabolic rate and heat production?
- Insulin
- Thyroxine (T4)
- Cortisol
- Growth hormone
Correct Answer: Thyroxine (T4)
Q2. The most sensitive initial laboratory test for primary hypothyroidism is:
- Serum free T4
- Thyroid peroxidase antibody
- Serum TSH
- Serum total T3
Correct Answer: Serum TSH
Q3. Which drug is a synthetic form of T4 used for lifelong replacement therapy in hypothyroidism?
- Liothyronine
- Propylthiouracil
- Levothyroxine
- Methimazole
Correct Answer: Levothyroxine
Q4. The preferred antithyroid drug in the first trimester of pregnancy is:
- Methimazole
- Propylthiouracil (PTU)
- Radioactive iodine (I-131)
- Levothyroxine
Correct Answer: Propylthiouracil (PTU)
Q5. Which laboratory pattern is most consistent with primary hyperthyroidism?
- High TSH, high T4
- Low TSH, high free T4
- High TSH, low T4
- Low TSH, low T4
Correct Answer: Low TSH, high free T4
Q6. A common adverse effect of methimazole therapy is:
- Hypoglycemia
- Aplastic anemia/agranulocytosis
- Hyperkalemia
- Adrenal suppression
Correct Answer: Aplastic anemia/agranulocytosis
Q7. Which condition is characterized by autoimmune destruction of adrenal cortex leading to deficiency of cortisol and aldosterone?
- Cushing syndrome
- Addison disease (primary adrenal insufficiency)
- Congenital adrenal hyperplasia
- Conn syndrome
Correct Answer: Addison disease (primary adrenal insufficiency)
Q8. First-line treatment for acute adrenal crisis includes:
- Oral levothyroxine
- IV hydrocortisone and aggressive fluid resuscitation
- IM insulin
- Oral fludrocortisone only
Correct Answer: IV hydrocortisone and aggressive fluid resuscitation
Q9. Excess cortisol production most commonly causes which syndrome?
- Cushing syndrome
- Addison disease
- Sheehan syndrome
- Conn syndrome
Correct Answer: Cushing syndrome
Q10. The dexamethasone suppression test is primarily used to evaluate:
- Thyroid function
- Growth hormone deficiency
- Cortisol feedback regulation and Cushing syndrome
- Calcium metabolism
Correct Answer: Cortisol feedback regulation and Cushing syndrome
Q11. Which drug is a glucocorticoid receptor agonist commonly used in replacement therapy and anti-inflammatory treatment?
- Fludrocortisone
- Hydrocortisone
- Spironolactone
- Mitotane
Correct Answer: Hydrocortisone
Q12. Mineralocorticoid replacement for primary adrenal insufficiency is best achieved with:
- Hydrocortisone alone
- Fludrocortisone
- Prednisone only
- Ketoconazole
Correct Answer: Fludrocortisone
Q13. Which enzyme defect commonly causes congenital adrenal hyperplasia with virilization and salt-wasting?
- 11β-hydroxylase deficiency
- 21-hydroxylase deficiency
- Aromatase overactivity
- 17α-hydroxylase deficiency
Correct Answer: 21-hydroxylase deficiency
Q14. The cell type that secretes insulin in the pancreas is:
- Alpha cell
- Beta cell
- Delta cell
- PP cell (gamma cell)
Correct Answer: Beta cell
Q15. Hemoglobin A1c reflects average blood glucose over approximately:
- 1 week
- 1 month
- 3 months
- 6 months
Correct Answer: 3 months
Q16. First-line oral pharmacotherapy for type 2 diabetes that decreases hepatic gluconeogenesis and improves insulin sensitivity is:
- Sulfonylureas
- Metformin
- Insulin glargine
- Pioglitazone
Correct Answer: Metformin
Q17. Which class of antidiabetic drugs works by inhibiting sodium-glucose co-transporter 2 (SGLT2) in the kidney?
- DPP-4 inhibitors
- Sulfonylureas
- SGLT2 inhibitors
- Alpha-glucosidase inhibitors
Correct Answer: SGLT2 inhibitors
Q18. A major adverse effect associated with SGLT2 inhibitors is:
- Hypoglycemia
- Genital mycotic infections and euglycemic DKA risk
- Severe lactic acidosis
- Thyroid storm
Correct Answer: Genital mycotic infections and euglycemic DKA risk
Q19. Which insulin has the fastest onset of action for prandial glucose control?
- Insulin glargine
- Regular human insulin
- Insulin lispro (rapid-acting)
- Neutral protamine Hagedorn (NPH)
Correct Answer: Insulin lispro (rapid-acting)
Q20. In type 1 diabetes presenting with diabetic ketoacidosis (DKA), the immediate priority is:
- Administer oral hypoglycemics
- Rapid IV insulin, fluid resuscitation, and electrolyte correction
- Start long-acting subcutaneous insulin only
- Give metformin
Correct Answer: Rapid IV insulin, fluid resuscitation, and electrolyte correction
Q21. Which hormone secreted by the anterior pituitary stimulates cortisol release from the adrenal cortex?
- TSH (thyroid stimulating hormone)
- ACTH (adrenocorticotropic hormone)
- LH (luteinizing hormone)
- Prolactin
Correct Answer: ACTH (adrenocorticotropic hormone)
Q22. A pituitary adenoma producing excessive growth hormone in adults typically causes:
- Gigantism
- Acromegaly
- Hypothyroidism
- Hyperprolactinemia
Correct Answer: Acromegaly
Q23. Pharmacologic therapy for acromegaly often includes which somatostatin analog?
- Octreotide
- Bromocriptine
- Levothyroxine
- Desmopressin
Correct Answer: Octreotide
Q24. Which drug is a dopamine agonist used to treat prolactin-secreting pituitary adenomas?
- Cabergoline
- Hydrocortisone
- Metformin
- Finasteride
Correct Answer: Cabergoline
Q25. Diabetes insipidus due to ADH deficiency is best treated with:
- Desmopressin (DDAVP)
- Hydrochlorothiazide alone
- Fludrocortisone
- Insulin
Correct Answer: Desmopressin (DDAVP)
Q26. Syndrome of inappropriate antidiuretic hormone secretion (SIADH) commonly causes which electrolyte abnormality?
- Hypernatremia
- Hyponatremia
- Hyperkalemia
- Hypocalcemia
Correct Answer: Hyponatremia
Q27. Primary hyperparathyroidism typically presents with which biochemical profile?
- High PTH, high serum calcium
- Low PTH, high serum calcium
- High PTH, low serum calcium
- Low PTH, low serum calcium
Correct Answer: High PTH, high serum calcium
Q28. The most common cause of hypercalcemia due to increased bone resorption is:
- Hypoparathyroidism
- Primary hyperparathyroidism
- Vitamin D deficiency
- Insulin overdose
Correct Answer: Primary hyperparathyroidism
Q29. Bisphosphonates treat osteoporosis by which primary mechanism?
- Increasing RANKL expression
- Stimulating osteoclast activity
- Inhibiting osteoclast-mediated bone resorption
- Increasing PTH secretion
Correct Answer: Inhibiting osteoclast-mediated bone resorption
Q30. A patient with pheochromocytoma is most likely to present with:
- Hypotension and bradycardia
- Episodes of hypertension, headache, and sweating
- Hypoglycemia and weight gain
- Hypercalcemia and bone pain
Correct Answer: Episodes of hypertension, headache, and sweating
Q31. Which test is most specific for diagnosing a pheochromocytoma?
- Serum cortisol
- Plasma free metanephrines or 24-hour urinary metanephrines
- Thyroid function tests
- Serum aldosterone
Correct Answer: Plasma free metanephrines or 24-hour urinary metanephrines
Q32. Primary hyperaldosteronism (Conn syndrome) often causes which electrolyte and blood pressure changes?
- Hyperkalemia and hypotension
- Hypokalemia and hypertension
- Hyponatremia and hypotension
- Hypercalcemia and bradycardia
Correct Answer: Hypokalemia and hypertension
Q33. Spironolactone treats hyperaldosteronism by acting as a:
- ACE inhibitor
- Mineralocorticoid receptor antagonist
- Beta-blocker
- Thyroid antagonist
Correct Answer: Mineralocorticoid receptor antagonist
Q34. Which endocrine neoplasia syndrome includes medullary thyroid carcinoma, pheochromocytoma, and parathyroid tumors?
- MEN type 1
- MEN type 2A
- MEN type 2B
- Von Hippel-Lindau disease
Correct Answer: MEN type 2A
Q35. A prolactinoma in a woman commonly causes which clinical symptom?
- Galactorrhea and amenorrhea
- Weight loss and polyuria
- Heat intolerance and palpitations
- Muscle weakness and hyperpigmentation
Correct Answer: Galactorrhea and amenorrhea
Q36. Which diagnostic test is most useful to monitor long-term glycemic control in diabetic patients?
- Fasting plasma glucose
- Random blood glucose
- HbA1c
- Serum insulin level
Correct Answer: HbA1c
Q37. The mechanism of action of sulfonylureas involves:
- Inhibition of hepatic gluconeogenesis
- Blocking SGLT2 in renal tubules
- Closing ATP-sensitive K+ channels in pancreatic beta cells to increase insulin release
- Inhibiting DPP-4 enzyme
Correct Answer: Closing ATP-sensitive K+ channels in pancreatic beta cells to increase insulin release
Q38. Which adverse effect is particularly important with thiazolidinediones (pioglitazone)?
- Bladder cancer risk and fluid retention/heart failure exacerbation
- Severe hypoglycemia
- Thyroid storm
- Pancreatitis exclusively
Correct Answer: Bladder cancer risk and fluid retention/heart failure exacerbation
Q39. In hyperthyroid emergencies (thyroid storm), the immediate pharmacologic interventions include:
- Only levothyroxine
- Beta-blockers, antithyroid drugs, iodine, and glucocorticoids
- Insulin infusion
- Desmopressin
Correct Answer: Beta-blockers, antithyroid drugs, iodine, and glucocorticoids
Q40. Elevated prolactin levels can be caused by which medication class?
- Dopamine agonists
- Dopamine antagonists (e.g., antipsychotics)
- Thyroid hormones
- Somatostatin analogs
Correct Answer: Dopamine antagonists (e.g., antipsychotics)
Q41. Which drug is used to treat hormone-secreting metastatic medullary thyroid carcinoma by inhibiting RET tyrosine kinase?
- Levothyroxine
- Vandetanib (or cabozantinib)
- Methimazole
- Octreotide
Correct Answer: Vandetanib (or cabozantinib)
Q42. A classic laboratory finding in primary hypothyroidism is:
- Low TSH, high T4
- High TSH, low free T4
- High TSH, high T4
- Low TSH, low T4
Correct Answer: High TSH, low free T4
Q43. Which agent is used to treat acromegaly by antagonizing growth hormone receptors?
- Pegvisomant
- Octreotide
- Bromocriptine
- Cabergoline
Correct Answer: Pegvisomant
Q44. Long-term systemic corticosteroid therapy commonly causes which metabolic complication?
- Hypoglycemia
- Hyperglycemia and insulin resistance
- Hypotension
- Decreased appetite
Correct Answer: Hyperglycemia and insulin resistance
Q45. Which laboratory study is most appropriate to evaluate suspected primary hyperparathyroidism?
- Serum PTH with simultaneous serum calcium
- Serum TSH alone
- 24-hour urinary glucose
- Fasting insulin level
Correct Answer: Serum PTH with simultaneous serum calcium
Q46. Insulin secretagogues that act primarily by closing KATP channels but are shorter-acting and used at mealtime are:
- First-generation sulfonylureas
- Meglitinides (repaglinide, nateglinide)
- Biguanides
- GLP-1 receptor agonists
Correct Answer: Meglitinides (repaglinide, nateglinide)
Q47. GLP-1 receptor agonists lower blood glucose by:
- Increasing renal glucose reabsorption
- Stimulating insulin release and slowing gastric emptying
- Directly inhibiting hepatic gluconeogenesis only
- Blocking alpha-glucosidase in the intestine
Correct Answer: Stimulating insulin release and slowing gastric emptying
Q48. Which endocrine emergency is characterized by severe hypothyroidism with hypothermia, bradycardia, and altered mental status?
- Thyroid storm
- Myxedema coma
- Diabetic ketoacidosis
- Adrenal crisis
Correct Answer: Myxedema coma
Q49. The most appropriate initial screening test for suspected Cushing syndrome is:
- 24-hour urinary free cortisol or late-night salivary cortisol or low-dose dexamethasone suppression test
- Serum potassium
- Serum TSH
- Random plasma glucose
Correct Answer: 24-hour urinary free cortisol or late-night salivary cortisol or low-dose dexamethasone suppression test
Q50. Which medication can precipitate adrenal insufficiency if abruptly discontinued after long-term use?
- Short-acting insulin
- Long-term systemic corticosteroids
- Sulfonylureas
- Thyroid hormone replacement
Correct Answer: Long-term systemic corticosteroids

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com