Immunosuppressant drugs are critical in the management of autoimmune diseases, prevention of transplant rejection, and certain inflammatory disorders. They act by inhibiting specific components of the immune response, either selectively or broadly. Their use requires careful monitoring due to risks of infections, malignancy, and drug toxicity.
This blog from Pharmacy Freak explains the classification, mechanisms, uses, drug of choice highlights, and key side effects of immunosuppressants with references from KDT, Sparsh Gupta, and Goodman & Gilman.
Table of Contents
What is Immunosuppressant Drugs
Immunosuppressant drugs are pharmacological agents that reduce or inhibit the immune system’s activity. They are used to prevent immune-mediated damage, particularly in organ transplantation and autoimmune diseases.
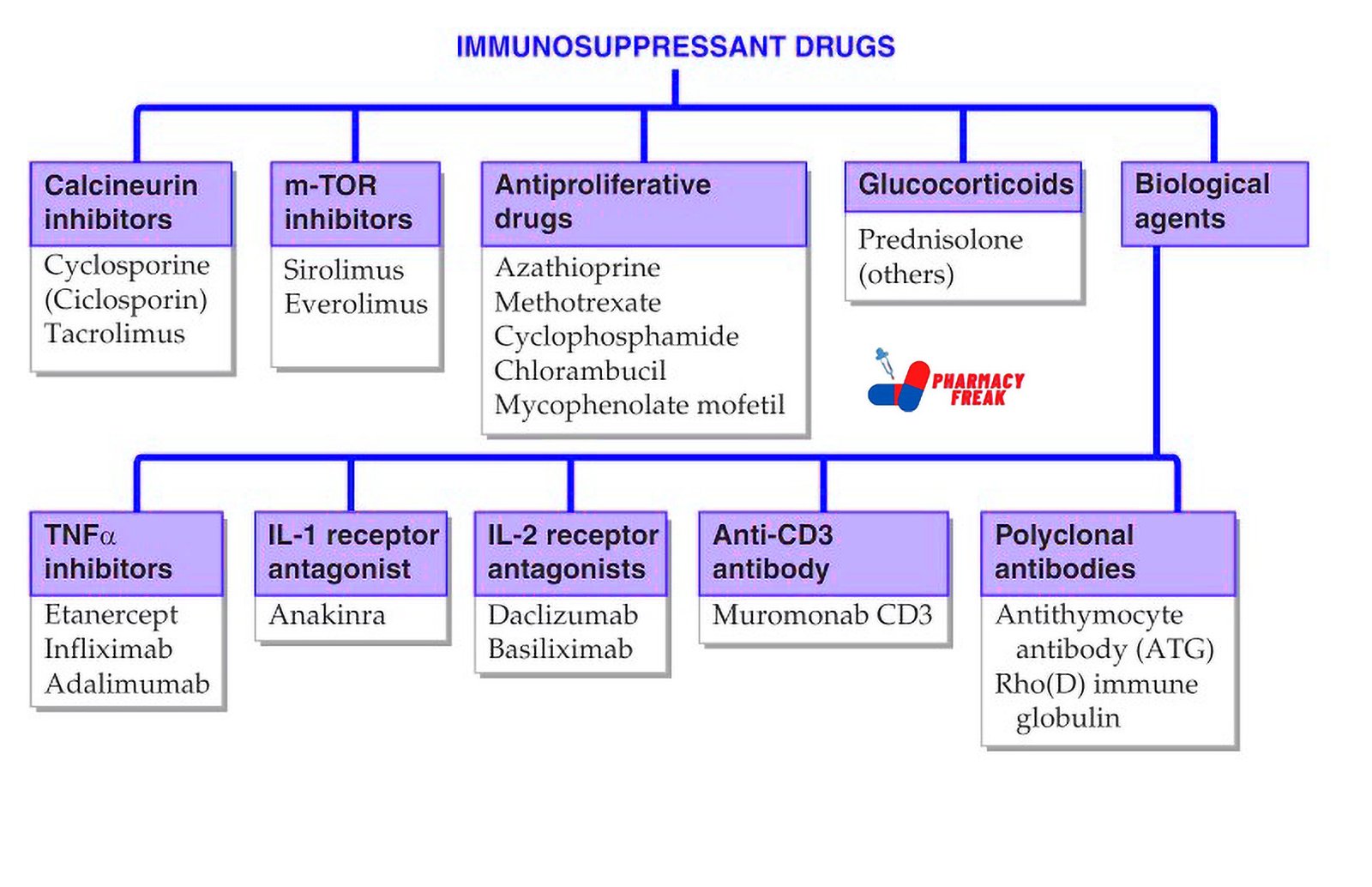
Classification of Immunosuppressant Drugs (KD Tripathi)
- Calcineurin inhibitors: Cyclosporine (Ciclosporin), Tacrolimus
- m-TOR inhibitors: Sirolimus, Everolimus
- Antiproliferative drugs: Azathioprine, Methotrexate, Cyclophosphamide, Chlorambucil, Mycophenolate mofetil
- Glucocorticoids: Prednisolone, others
- Biological agents –
- TNFα inhibitors: Etanercept, Infliximab, Adalimumab
- IL-1 receptor antagonist: Anakinra
- IL-2 receptor antagonists: Daclizumab, Basiliximab
- Anti-CD3 antibody: Muromonab CD3
- Polyclonal antibodies: Antithymocyte antibody (ATG), Rho(D) immune globulin
Classification of Immunosuppressant Drugs (General)
- Calcineurin Inhibitors
Mechanism: Inhibit calcineurin, preventing IL-2 transcription and T-cell activation
Drugs: Cyclosporine, Tacrolimus
Use: Organ transplantation, autoimmune diseases
Note: Tacrolimus is more potent and preferred in many transplant protocols - mTOR Inhibitors
Mechanism: Inhibit mammalian target of rapamycin (mTOR), blocking T-cell proliferation
Drugs: Sirolimus (Rapamycin), Everolimus
Use: Kidney transplantation, coronary stent restenosis prevention
Note: Not nephrotoxic unlike calcineurin inhibitors - Antiproliferative and Antimetabolic Agents
Mechanism: Inhibit DNA synthesis and lymphocyte proliferation
Drugs: Azathioprine, Mycophenolate mofetil, Methotrexate, Leflunomide
Use: Autoimmune diseases (SLE, rheumatoid arthritis), transplantation
Note: Mycophenolate selectively inhibits guanine synthesis in lymphocytes - Glucocorticoids
Mechanism: Broad anti-inflammatory and immunosuppressive actions; inhibit cytokine production
Drugs: Prednisolone, Methylprednisolone, Dexamethasone
Use: Almost all inflammatory and autoimmune diseases, transplant rejection prophylaxis
Note: First-line for acute rejection episodes - Monoclonal Antibodies
Mechanism: Target specific immune markers (CD3, CD20, IL-2 receptor, TNF-α)
Examples:
- Muromonab–CD3 – Binds CD3 receptor on T-cells
- Basiliximab, Daclizumab – IL-2 receptor antagonists
- Rituximab – Anti-CD20 for B-cell lymphomas and autoimmune diseases
- Infliximab, Adalimumab – Anti-TNF agents for rheumatoid arthritis and Crohn’s disease
- Polyclonal Antibodies
Mechanism: Contain antibodies against multiple T-cell antigens
Drugs: Antithymocyte globulin (ATG), Antilymphocyte globulin (ALG)
Use: Induction therapy in transplantation, aplastic anemia - Janus Kinase (JAK) Inhibitors
Mechanism: Block intracellular signaling via JAK-STAT pathway
Drug: Tofacitinib
Use: Rheumatoid arthritis, ulcerative colitis - Others
- Cyclophosphamide – Alkylating agent used in severe autoimmune diseases like lupus nephritis
- Hydroxychloroquine – Antimalarial with immunomodulatory effects
- Thalidomide – Inhibits TNF-α, used in multiple myeloma and leprosy reactions
Uses
Immunosuppressant drugs are used in a wide range of clinical conditions:
- Solid organ transplantation (kidney, liver, heart)
- Hematopoietic stem cell transplantation
- Autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, psoriasis, inflammatory bowel disease)
- Prevention and treatment of graft-versus-host disease
- Nephrotic syndrome and glomerulonephritis
- Certain cancers (as cytotoxic immunosuppressants)
Drug of Choice Highlights
- Kidney transplantation – Tacrolimus + Mycophenolate mofetil + Prednisolone
- Acute transplant rejection – High-dose Methylprednisolone
- Lupus nephritis – Cyclophosphamide or Mycophenolate mofetil
- Rheumatoid arthritis – Methotrexate
- Crohn’s disease or ulcerative colitis – Infliximab
- Multiple sclerosis – Monoclonal antibodies (e.g., Natalizumab)
- Aplastic anemia – Antithymocyte globulin + Cyclosporine
- Autoimmune hemolytic anemia – Prednisolone
- Pemphigus vulgaris – Rituximab or Azathioprine
Side Effects
- Calcineurin inhibitors – Nephrotoxicity, hypertension, neurotoxicity, gingival hyperplasia (with Cyclosporine)
- mTOR inhibitors – Hyperlipidemia, delayed wound healing, mouth ulcers
- Antimetabolites – Bone marrow suppression, GI disturbances, increased infection risk
- Glucocorticoids – Cushingoid features, osteoporosis, hyperglycemia, hypertension
- Monoclonal antibodies – Infusion reactions, cytokine release syndrome, increased risk of malignancy
- Cyclophosphamide – Hemorrhagic cystitis, infertility, secondary malignancies
- JAK inhibitors – Risk of thromboembolism, infections, elevated liver enzymes
Updated Clinical Pearls
- Tacrolimus is preferred over Cyclosporine due to better graft survival and fewer cosmetic side effects.
- Mycophenolate is selectively toxic to lymphocytes and has replaced Azathioprine in many protocols.
- mTOR inhibitors can be used in patients with calcineurin inhibitor-induced nephrotoxicity.
- Glucocorticoids are the mainstay in acute immunologic flares but should be tapered to minimize long-term side effects.
- Biologics require screening for latent infections like tuberculosis and hepatitis before initiation.
- Cyclophosphamide requires hydration and mesna to prevent hemorrhagic cystitis.
References
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. p. 799–812
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 266–270
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 979–994
I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com