- Tuberculosis (TB) remains a major global health problem, especially in developing countries. Caused by Mycobacterium tuberculosis, TB primarily affects the lungs but can spread to other organs. The treatment of TB requires long-term multidrug regimens to prevent resistance and relapse.
- In this blog by Pharmacy Freak, we’ll explore the classification of antitubercular drugs in both standard and WHO-alternative formats. We also highlight the drugs of choice (DOC) for different types of TB infections
Table of Contents
🔬 What Are Antitubercular Drugs?
Antitubercular drugs are antibiotics specifically used to treat tuberculosis. They work by either killing actively growing mycobacteria or inhibiting bacterial protein and cell wall synthesis. TB treatment typically involves multiple drugs over 6 to 9 months, depending on the stage and resistance profile.
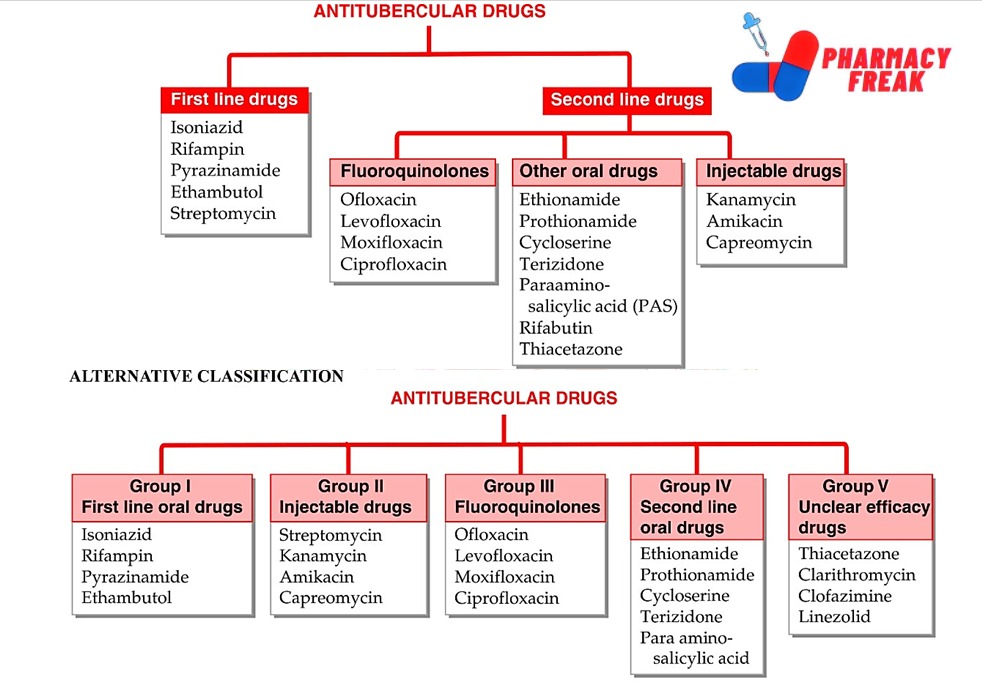
📊 Standard Classification of Antitubercular Drugs
🧪 First-Line Drugs (Most Effective, Least Toxic)
These are the primary drugs used in the initial intensive phase of TB treatment.
- Isoniazid (INH) – Bactericidal for rapidly growing TB bacilli.
✅ DOC for active pulmonary TB and latent TB (Sparsh Gupta, KDT). - Rifampin (RIF) – Broad-spectrum antibiotic that inhibits RNA polymerase.
✅ DOC for all forms of TB including meningitis. - Pyrazinamide (PZA) – Active in acidic environments like TB granulomas.
- Ethambutol (EMB) – Bacteriostatic; inhibits arabinosyl transferase affecting cell wall synthesis.
- Streptomycin (STM) – Aminoglycoside used in severe forms of TB like meningitis and miliary TB.
🧪 Second-Line Drugs
Used when first-line drugs fail or in MDR-TB (multi-drug resistant TB).
A. Fluoroquinolones
- Ofloxacin
- Levofloxacin ✅ DOC for MDR-TB as per WHO guidelines.
- Moxifloxacin
- Ciprofloxacin
These inhibit DNA gyrase and are active against resistant TB strains.
B. Other Oral Drugs
- Ethionamide, Prothionamide – Inhibit mycolic acid synthesis. Used in MDR-TB.
- Cycloserine – Bacteriostatic; inhibits cell wall synthesis.
- Terizidone – Similar to cycloserine.
- Para-aminosalicylic acid (PAS) – Folate synthesis inhibitor; less commonly used.
- Rifabutin – Used in HIV-TB co-infections due to fewer drug interactions.
- Thiacetazone – Rarely used now due to high toxicity in HIV patients.
C. Injectable Drugs
- Kanamycin, Amikacin, Capreomycin – Second-line aminoglycosides used in MDR and XDR TB.
WHO/Alternative Classification of Antitubercular Drugs
This classification is more therapy-oriented and is commonly followed in clinical practice.
| Group | Classification | Examples |
|---|---|---|
| I | First-line oral drugs | Isoniazid, Rifampin, Pyrazinamide, Ethambutol |
| II | Injectable drugs | Streptomycin, Kanamycin, Amikacin, Capreomycin |
| III | Fluoroquinolones | Ofloxacin, Levofloxacin, Moxifloxacin, Ciprofloxacin |
| IV | Second-line oral drugs | Ethionamide, Prothionamide, Cycloserine, Terizidone, PAS |
| V | Drugs with unclear efficacy | Thiacetazone, Clarithromycin, Clofazimine, Linezolid |
💊 Drug of Choice (DOC) for Specific Forms of TB
| Condition | Drug of Choice |
|---|---|
| Pulmonary TB (initial) | Isoniazid + Rifampin + Pyrazinamide + Ethambutol (HRZE) |
| Latent TB | Isoniazid (6–9 months) |
| TB Meningitis | Rifampin + Isoniazid + Pyrazinamide + Streptomycin |
| MDR-TB | Levofloxacin + Amikacin + Ethionamide |
| TB in HIV Patients | Replace Rifampin with Rifabutin |
⚠️ Major Adverse Effects
- Isoniazid – Hepatitis, peripheral neuropathy (prevented by pyridoxine)
- Rifampin – Red/orange urine, hepatotoxicity
- Ethambutol – Optic neuritis
- Streptomycin – Ototoxicity, nephrotoxicity
- PAS – GI upset, hypothyroidism
- Fluoroquinolones – Tendon rupture, QT prolongation
🧠 Trivia Time
- The shortest TB treatment possible under DOTS is 6 months with HRZE (first-line).
- Rifampin not only treats TB but also meningococcal and staphylococcal infections.
🧬 Newer Antitubercular Drugs and Current Treatment Trends
📌 Bedaquiline
- Mechanism: Inhibits mycobacterial ATP synthase
- Indication: Used for MDR and XDR-TB when resistance to fluoroquinolones (FQ) or second-line injectables is confirmed
- Dose: 400 mg daily for 2 weeks, then 200 mg thrice weekly for 22 weeks
- Caution: Prolongs QT interval
📌 Delamanid
- Mechanism: Nitroimidazole class; inhibits mycolic acid synthesis
- Use: Effective in XDR-TB, added in regimens with Linezolid and Clofazimine
- Caution: QT prolongation is a notable side effect
📌 Linezolid
- Mechanism: Binds to 50S ribosomal subunit, blocks initiation complex
- Used in: MDR/XDR TB with resistance to most first- and second-line drugs
- Side Effects: Myelosuppression, optic neuritis if used >4 weeks
Reference
- Tripathi KD. Essentials of Medical Pharmacology. 7th ed. New Delhi: Jaypee Brothers Medical Publishers, Chapter-55 Antitubercular Drugs
- Gupta S, Garg A. Review of Pharmacology. 15th ed. New Delhi: Jaypee Brothers Medical Publishers; 2023. p. 207–212.
- Brunton LL, Chabner BA, Knollmann BC, editors. Goodman and Gilman’s The Pharmacological Basis of Therapeutics. 12th ed. New York: McGraw-Hill Education; 2011. p. 1473–1498.
Related Links
I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com