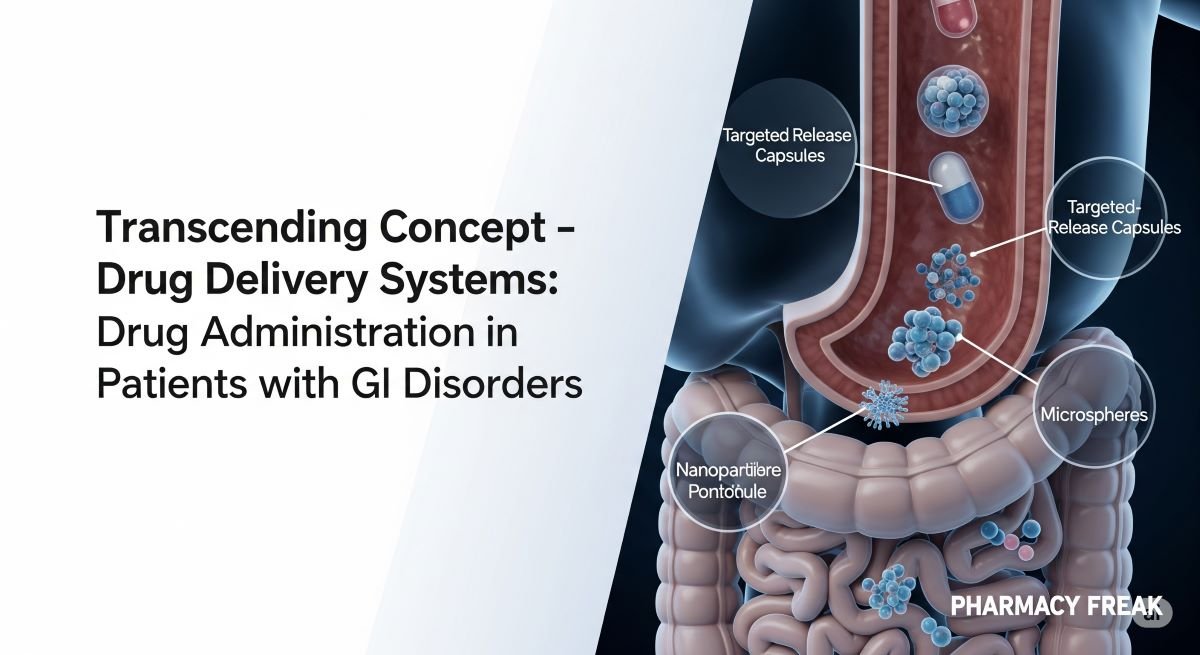
The effectiveness of a medication depends not only on the active drug but also on its delivery system. This “transcending concept,” a cornerstone of the PharmD curriculum explored in courses like Drug Delivery Systems and Patient Care 4, becomes particularly critical when managing patients with gastrointestinal disorders. Conditions that alter GI motility, pH, or absorptive surfaces, as well as the presence of enteral feeding tubes, can fundamentally change a drug’s pharmacokinetic profile. This quiz will test your knowledge on navigating these complex drug administration challenges to ensure patient safety and therapeutic efficacy.
1. A patient has a J-tube (jejunostomy tube). Which of the following statements is true regarding drug administration?
- a. All oral medications are safe to administer through a J-tube.
- b. Drugs that require an acidic environment for absorption may have reduced bioavailability.
- c. Extended-release formulations can be crushed and given via a J-tube.
- d. The J-tube is the preferred route for all IV medications.
Answer: b. Drugs that require an acidic environment for absorption may have reduced bioavailability.
2. Which of the following oral dosage forms should generally NEVER be crushed for administration via an enteral feeding tube?
- a. Immediate-release tablets
- b. Enteric-coated tablets
- c. Scored tablets
- d. Chewable tablets
Answer: b. Enteric-coated tablets
3. What is the primary purpose of an enteric coating on a tablet like aspirin or bisacodyl?
- a. To improve the taste of the medication.
- b. To protect the drug from degradation in stomach acid or to protect the stomach from the drug.
- c. To provide immediate release in the stomach.
- d. To allow the tablet to be easily split in half.
Answer: b. To protect the drug from degradation in stomach acid or to protect the stomach from the drug.
4. A patient with severe gastroparesis (delayed gastric emptying) is prescribed an immediate-release oral pain medication. What is a potential pharmacokinetic consequence?
- a. The drug will be absorbed much faster than normal.
- b. The time to peak concentration (Tmax) will be significantly delayed.
- c. The drug’s bioavailability will increase to over 100%.
- d. The drug will be completely metabolized in the stomach.
Answer: b. The time to peak concentration (Tmax) will be significantly delayed.
5. When administering medications through an enteral feeding tube, what is a critical step to prevent clogging?
- a. Mixing all medications together before administration.
- b. Using carbonated beverages to dissolve the medications.
- c. Flushing the tube with water before and after each medication.
- d. Administering medications as a thick paste.
Answer: c. Flushing the tube with water before and after each medication.
6. The topic “Administering Medications Through Enteral Tubes” is a specific lecture within which course?
- a. PHA5784C Patient Care 4
- b. PHA5104 Sterile Compounding
- c. PHA5703 Pharmacy Law and Ethics
- d. PHA5878C Patient Care 3
Answer: a. PHA5784C Patient Care 4
7. A patient with chronic diarrhea and rapid GI transit may have reduced absorption of which type of oral medication?
- a. An immediate-release liquid formulation.
- b. A sublingual tablet.
- c. An extended-release (ER) or long-acting (LA) formulation.
- d. An orally disintegrating tablet (ODT).
Answer: c. An extended-release (ER) or long-acting (LA) formulation.
8. Certain mesalamine formulations (e.g., Asacol HD) are designed for patients with ulcerative colitis. Their delivery system relies on a pH-sensitive coating that releases the drug at:
- a. The acidic pH of the stomach.
- b. The slightly acidic pH of the duodenum.
- c. The more alkaline pH of the terminal ileum and colon.
- d. Any pH level.
Answer: c. The more alkaline pH of the terminal ileum and colon.
9. A patient with severe nausea and vomiting is unable to tolerate oral medications. Which of the following represents an alternative route of administration for an antiemetic?
- a. An intravenous (IV) injection
- b. A rectal (PR) suppository
- c. A transdermal patch
- d. All of the above
Answer: d. All of the above
10. Why must enteral tube feeds be held before and after administering medications like phenytoin or ciprofloxacin?
- a. The medications taste bad when mixed with feeds.
- b. The tube feed can bind to the medication, significantly reducing its absorption.
- c. The combination increases the risk of clogging the tube.
- d. The medications curdle the tube feed formula.
Answer: b. The tube feed can bind to the medication, significantly reducing its absorption.
11. The course “Drug Delivery Systems” covers the rational formulation and usage of drug products.
- a. True
- b. False
Answer: a. True
12. A patient with celiac disease has significant villous atrophy in the small intestine. This is most likely to:
- a. Increase the absorption of all oral drugs.
- b. Decrease the absorption of oral drugs due to a reduced surface area.
- c. Have no effect on drug absorption.
- d. Increase the first-pass metabolism of drugs.
Answer: b. Decrease the absorption of oral drugs due to a reduced surface area.
13. A patient is taking ketoconazole, a drug that requires an acidic environment for absorption. If this patient is also taking omeprazole, what is the likely outcome?
- a. The absorption of ketoconazole will be increased.
- b. The absorption of ketoconazole will be significantly decreased.
- c. The absorption of omeprazole will be decreased.
- d. There is no interaction between these two agents.
Answer: b. The absorption of ketoconazole will be significantly decreased.
14. If a liquid formulation of a medication is available, it is generally preferred for feeding tube administration over a crushed tablet.
- a. True
- b. False
Answer: a. True
15. What is a major concern when using sorbitol-containing liquid medications, especially in large volumes, for a patient with a feeding tube?
- a. It can cause osmotic diarrhea.
- b. It causes significant constipation.
- c. It has a high risk of clogging the tube.
- d. It interacts with plastic tubing.
Answer: a. It can cause osmotic diarrhea.
16. Which of the following dosage forms bypasses the GI tract and first-pass metabolism entirely?
- a. An immediate-release oral tablet
- b. An enteric-coated oral tablet
- c. An intravenous injection
- d. An oral capsule
Answer: c. An intravenous injection
17. A patient with short bowel syndrome who has had a large portion of their small intestine removed will likely experience:
- a. Increased absorption of nutrients and drugs.
- b. Malabsorption of nutrients and drugs.
- c. No change in absorption.
- d. Delayed gastric emptying.
Answer: b. Malabsorption of nutrients and drugs.
18. The “Drug Dosage Form Administration” module in the Drug Delivery Systems course covers anatomical and physiological properties important for drug delivery.
- a. True
- b. False
Answer: a. True
19. Why should a pharmacist be cautious when a provider orders a sublingual tablet to be given through a G-tube?
- a. The sublingual formulation is designed for rapid absorption through the oral mucosa and will bypass first-pass metabolism, which will not occur if given via G-tube.
- b. It is the preferred method of administration.
- c. It will cause the tube to clog.
- d. It will increase the drug’s potency.
Answer: a. The sublingual formulation is designed for rapid absorption through the oral mucosa and will bypass first-pass metabolism, which will not occur if given via G-tube.
20. A patient with a J-tube has their medications administered directly into the:
- a. Stomach
- b. Duodenum
- c. Jejunum
- d. Esophagus
Answer: c. Jejunum
21. The “Biopharmaceutics” module in the Drug Delivery Systems course covers the relationship between a drug’s properties and its fate in the body.
- a. True
- b. False
Answer: a. True
22. A patient with severe Crohn’s disease and active inflammation may have unpredictable absorption of oral medications due to:
- a. Altered intestinal transit time.
- b. Changes in intestinal pH.
- c. Damaged mucosal surface area.
- d. All of the above.
Answer: d. All of the above.
23. Which of the following is an example of an orally disintegrating tablet (ODT)?
- a. A tablet designed to be swallowed whole.
- b. A tablet that dissolves on the tongue without water.
- c. An enteric-coated tablet.
- d. An extended-release tablet.
Answer: b. A tablet that dissolves on the tongue without water.
24. ODT formulations are particularly useful for which patient population with GI issues?
- a. Patients with severe diarrhea.
- b. Patients with dysphagia (difficulty swallowing) or nausea.
- c. Patients with gastroparesis.
- d. Patients with constipation.
Answer: b. Patients with dysphagia (difficulty swallowing) or nausea.
25. When crushing tablets for tube administration, what is the best practice?
- a. Crush multiple medications together to save time.
- b. Crush each medication separately, mix with water, and flush between each one.
- c. Use a pill crusher that has been used for hazardous drugs.
- d. Crush the tablets into a fine powder and pour it directly into the tube without water.
Answer: b. Crush each medication separately, mix with water, and flush between each one.
26. The abbreviation “SR” on a tablet stands for:
- a. Super-release
- b. Standard-release
- c. Sustained-release
- d. Sublingual-release
Answer: c. Sustained-release
27. A patient with a history of bariatric surgery (e.g., gastric bypass) may have altered absorption of oral drugs due to:
- a. A change in gastric pH.
- b. A reduced surface area for absorption.
- c. Bypassing a portion of the small intestine.
- d. All of the above.
Answer: d. All of the above.
28. What is the primary reason for flushing an enteral tube with water?
- a. To provide the patient with hydration.
- b. To ensure the medication is delivered to the GI tract and to maintain tube patency.
- c. To cool down the tube.
- d. To check for leaks.
Answer: b. To ensure the medication is delivered to the GI tract and to maintain tube patency.
29. The “Transcending Concept” of Drug Delivery Systems is a module in which course?
- a. PHA5784C Patient Care 4
- b. PHA5163L Professional Skills Lab 3
- c. PHA5781 Patient Care I
- d. PHA5782C Patient Care 2
Answer: a. PHA5784C Patient Care 4
30. A gelatin capsule’s shell will dissolve in the:
- a. Mouth
- b. Esophagus
- c. Stomach
- d. Colon
Answer: c. Stomach
31. Some medications, like pancreatic enzymes, are formulated as enteric-coated beads inside a capsule. If a patient cannot swallow the capsule, what is the correct administration method?
- a. The capsule must be swallowed whole.
- b. The capsule can be opened and the beads can be crushed.
- c. The capsule can be opened and the intact beads can be mixed with an acidic food like applesauce.
- d. The medication cannot be given.
Answer: c. The capsule can be opened and the intact beads can be mixed with an acidic food like applesauce.
32. The absorption of which of the following nutrients can be significantly impaired in a patient with Crohn’s disease affecting the terminal ileum?
- a. Vitamin C
- b. Vitamin B12
- c. Iron
- d. Vitamin K
Answer: b. Vitamin B12
33. What is the pharmacist’s best resource for determining if a specific tablet can be crushed?
- a. A Google image search.
- b. Asking the patient.
- c. Professional drug information resources that provide this information (e.g., ISMP’s “Do Not Crush” list).
- d. The color of the tablet.
Answer: c. Professional drug information resources that provide this information (e.g., ISMP’s “Do Not Crush” list).
34. The presence of food in the stomach generally does what to gastric emptying?
- a. Speeds it up.
- b. Slows it down.
- c. Has no effect.
- d. Stops it completely.
Answer: b. Slows it down.
35. A patient with a G-tube has their medications administered directly into the:
- a. Esophagus
- b. Jejunum
- c. Duodenum
- d. Stomach
Answer: d. Stomach
36. A patient is prescribed an oral solution that is known to be very viscous. What is a potential problem for enteral tube administration?
- a. It may be difficult to draw up and push through the tube, increasing clogging risk.
- b. It will be absorbed too quickly.
- c. It will have improved bioavailability.
- d. It has a lower risk of causing diarrhea.
Answer: a. It may be difficult to draw up and push through the tube, increasing clogging risk.
37. How can a pharmacist help manage drug therapy in a patient with gastroparesis?
- a. Recommend switching essential medications to liquid or ODT formulations.
- b. Advise the patient to take their medications with large, fatty meals.
- c. Recommend adding more slowly-absorbed drugs.
- d. All medications should be switched to IV.
Answer: a. Recommend switching essential medications to liquid or ODT formulations.
38. The pH of the stomach is typically ____, while the pH of the small intestine is ____.
- a. Acidic, Alkaline
- b. Alkaline, Acidic
- c. Neutral, Acidic
- d. Acidic, Neutral
Answer: a. Acidic, Alkaline
39. Understanding drug dosage forms and how they are designed is a key objective in the Drug Delivery Systems course.
- a. True
- b. False
Answer: a. True
40. A patient has a clogged G-tube after a crushed medication was administered. What is the first-line intervention?
- a. Attempt to flush the tube with warm water using a syringe.
- b. Immediately call for surgical removal of the tube.
- c. Push a carbonated beverage into the tube.
- d. Use a guidewire to clear the clog.
Answer: a. Attempt to flush the tube with warm water using a syringe.
41. The rate-limiting step for the absorption of a poorly soluble drug is often:
- a. Its transit time through the stomach.
- b. Its dissolution in the GI fluids.
- c. Its metabolism by CYP3A4.
- d. Its binding to plasma proteins.
Answer: b. Its dissolution in the GI fluids.
42. Which dosage form would be most appropriate for a patient with severe mucositis and odynophagia (painful swallowing)?
- a. A large, uncoated tablet.
- b. An oral liquid, IV formulation, or transdermal patch.
- c. An extended-release capsule.
- d. An effervescent tablet.
Answer: b. An oral liquid, IV formulation, or transdermal patch.
43. A pharmacist’s role in drug administration for patients with GI disorders includes:
- a. Identifying potential issues based on dosage form and patient condition.
- b. Recommending alternative formulations or routes.
- c. Educating nurses and patients on proper administration techniques.
- d. All of the above.
Answer: d. All of the above.
44. If a medication must be separated from tube feeds, what is the general recommendation?
- a. Hold the feed for at least 1-2 hours before and after drug administration.
- b. Hold the feed for 5 minutes.
- c. The drug cannot be given.
- d. The feed can be run at a slower rate.
Answer: a. Hold the feed for at least 1-2 hours before and after drug administration.
45. Why is a J-tube placement sometimes preferred over a G-tube?
- a. It is easier to place.
- b. It allows for feeding and medication administration while bypassing the stomach, which is useful in gastroparesis or high aspiration risk.
- c. It can handle thicker liquids.
- d. It never clogs.
Answer: b. It allows for feeding and medication administration while bypassing the stomach, which is useful in gastroparesis or high aspiration risk.
46. A patient with a GI disorder that causes fat malabsorption may have difficulty absorbing which type of medication?
- a. A highly water-soluble drug.
- b. A highly lipophilic (fat-soluble) drug.
- c. An injectable drug.
- d. An inhaled drug.
Answer: b. A highly lipophilic (fat-soluble) drug.
47. The primary reason for using an extended-release formulation is to:
- a. Provide a faster onset of action.
- b. Reduce dosing frequency and provide a more consistent drug level.
- c. Improve the taste.
- d. Make the tablet cheaper.
Answer: b. Reduce dosing frequency and provide a more consistent drug level.
48. An active learning session covering drug administration in GI disorders is part of which course?
- a. PHA5784C Patient Care 4
- b. PHA5163L Professional Skills Lab 3
- c. PHA5781 Patient Care I
- d. PHA5782C Patient Care 2
Answer: a. PHA5784C Patient Care 4
49. For a patient with a J-tube, which of the following is true?
- a. First-pass metabolism is completely avoided.
- b. First-pass metabolism is NOT avoided, but gastric emptying is.
- c. The drug is absorbed directly into the bloodstream.
- d. Only liquid medications can be given.
Answer: b. First-pass metabolism is NOT avoided, but gastric emptying is.
50. The ultimate goal of understanding drug delivery systems in patients with GI disorders is to:
- a. Ensure the patient receives the intended dose in a manner that allows for optimal absorption and therapeutic effect.
- b. Always choose the most complex dosage form.
- c. Be able to compound any medication for tube administration.
- d. Avoid using oral medications in all patients with GI issues.
Answer: a. Ensure the patient receives the intended dose in a manner that allows for optimal absorption and therapeutic effect.

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com