Introduction
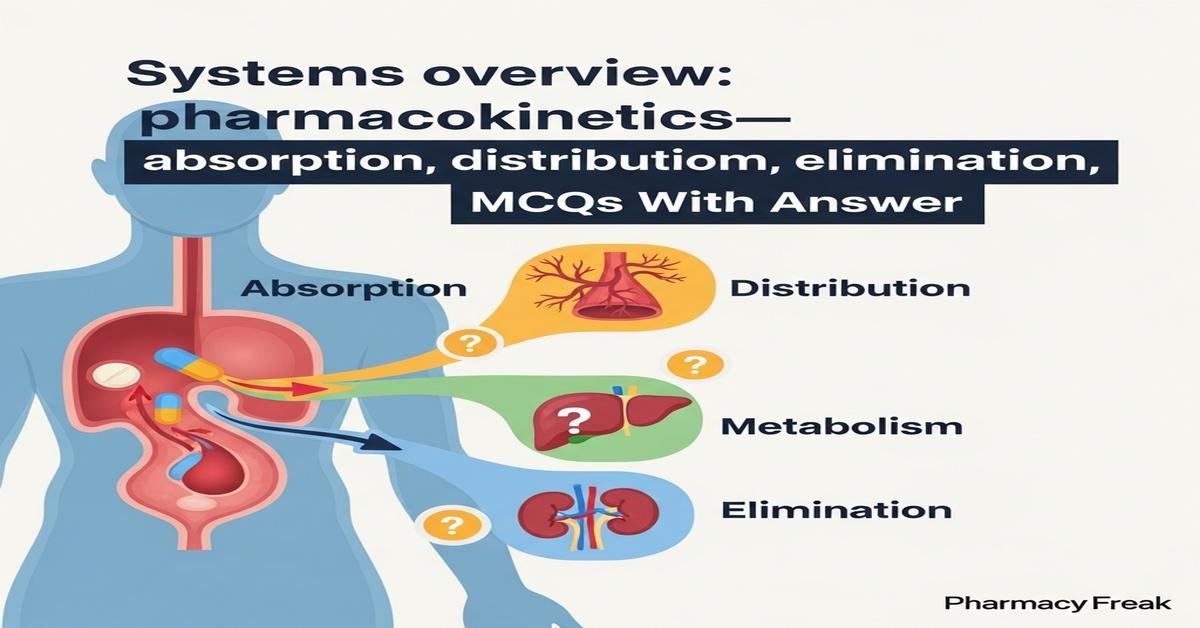
This MCQ set focuses on an integrated systems overview of pharmacokinetics — covering absorption, distribution, metabolism and elimination — tailored for M.Pharm students. Questions probe mechanistic principles, quantitative relationships and clinical implications: bioavailability and first‑pass effects, factors affecting membrane permeation and transporters, determinants of volume of distribution and protein binding, hepatic and extrahepatic metabolic pathways including enzyme kinetics and polymorphisms, as well as renal and biliary routes of drug clearance. Emphasis is on applying concepts to dosing, interpretation of clearance and half‑life, nonlinear kinetics and special situations such as enterohepatic recirculation. Use these items for exam prep and to deepen problem‑solving skills in advanced pharmacokinetics.
Q1. Which factor primarily determines the rate of passive diffusion of a weak acid drug across the gastric mucosa?
- Lipid solubility and degree of ionization at gastric pH
- Hepatic extraction ratio
- Plasma protein binding in systemic circulation
- P-glycoprotein mediated efflux
Correct Answer: Lipid solubility and degree of ionization at gastric pH
Q2. Bioavailability (F) of an orally administered drug is least directly affected by which of the following?
- Extent of intestinal metabolism by CYP enzymes
- Drug solubility and dissolution rate
- Renal tubular secretion
- First‑pass hepatic extraction
Correct Answer: Renal tubular secretion
Q3. A drug with a high volume of distribution (Vd) most likely demonstrates which characteristic?
- Extensive tissue penetration and low plasma concentration
- Predominant confinement to blood plasma
- Exclusive renal elimination as unchanged drug
- High hepatic extraction ratio
Correct Answer: Extensive tissue penetration and low plasma concentration
Q4. Which statement best describes the hepatic extraction ratio (E) of a drug?
- It represents the fraction of drug removed from blood in a single pass through the liver
- It is equal to renal clearance divided by glomerular filtration rate
- It measures the fraction of drug bound to plasma proteins
- It is independent of hepatic blood flow
Correct Answer: It represents the fraction of drug removed from blood in a single pass through the liver
Q5. Which mechanism most commonly causes a drug to display nonlinear (capacity‑limited) pharmacokinetics at therapeutic doses?
- Saturation of metabolizing enzymes following Michaelis‑Menten kinetics
- Increased plasma protein binding at high concentrations
- Enhanced renal glomerular filtration with dose
- Induction of P‑glycoprotein transporters acutely
Correct Answer: Saturation of metabolizing enzymes following Michaelis‑Menten kinetics
Q6. Which parameter is directly proportional to clearance when calculating steady‑state concentration during constant rate infusion?
- Rate of drug infusion
- Volume of distribution
- Half‑life (t1/2)
- Bioavailability (F) after oral dosing
Correct Answer: Rate of drug infusion
Q7. For a drug eliminated primarily by glomerular filtration and tubular secretion, which clinical factor will most reduce renal clearance?
- Concurrent administration of a transporter inhibitor that blocks proximal tubular secretion
- Increased urine pH that enhances ion trapping of the drug
- Increase in glomerular filtration rate due to hyperfiltration
- Proteinuria increasing free drug in urine
Correct Answer: Concurrent administration of a transporter inhibitor that blocks proximal tubular secretion
Q8. Which of the following best explains the concept of enterohepatic recirculation?
- Biliary excretion of drug conjugates followed by intestinal deconjugation and reabsorption
- Direct renal excretion of unchanged drug with reabsorption in the distal tubule
- Sustained release formulation prolonging absorption
- Metabolic activation of prodrugs in the gut lumen
Correct Answer: Biliary excretion of drug conjugates followed by intestinal deconjugation and reabsorption
Q9. A drug is highly bound (>95%) to plasma albumin. Which statement is most accurate regarding its pharmacokinetics?
- Only unbound fraction is available for glomerular filtration, metabolism and pharmacologic effect
- High plasma protein binding increases the drug’s hepatic clearance proportionally
- Protein binding prevents the drug from undergoing enterohepatic recycling
- High binding makes volume of distribution very large (>100 L/kg)
Correct Answer: Only unbound fraction is available for glomerular filtration, metabolism and pharmacologic effect
Q10. Clearance (CL) of a drug is defined as which of the following?
- The volume of plasma completely cleared of drug per unit time
- Total amount of drug eliminated per unit time regardless of concentration
- The fraction of dose excreted unchanged in urine
- The time required for plasma concentration to decrease by 50%
Correct Answer: The volume of plasma completely cleared of drug per unit time
Q11. Which kinetic parameter should be increased to achieve a rapid target concentration for a drug with a long half‑life?
- Administer a loading dose calculated from Vd
- Increase maintenance infusion rate without a loading dose
- Reduce the dosing interval without changing dose
- Decrease bioavailability by changing formulation
Correct Answer: Administer a loading dose calculated from Vd
Q12. Which of the following is a major consequence of induction of hepatic CYP enzymes for chronic therapy?
- Increased clearance leading to lower plasma concentrations of substrate drugs
- Immediate competitive inhibition of drug metabolism
- Decreased glucuronidation without affecting oxidation
- Reduced renal excretion due to transporter down‑regulation
Correct Answer: Increased clearance leading to lower plasma concentrations of substrate drugs
Q13. For a drug that follows first‑order elimination, which statement is true about half‑life (t1/2)?
- Half‑life is constant and independent of concentration
- Half‑life increases as plasma concentration approaches Km
- Half‑life equals volume of distribution divided by dose
- Half‑life is shorter for drugs with high protein binding only
Correct Answer: Half‑life is constant and independent of concentration
Q14. A drug with extraction ratio close to 1 is best described as?
- High‑extraction drug; hepatic clearance primarily dependent on hepatic blood flow
- Low‑extraction drug; hepatic clearance primarily dependent on intrinsic clearance and protein binding
- Predominantly renally cleared drug
- Drug undergoing enterohepatic cycling exclusively
Correct Answer: High‑extraction drug; hepatic clearance primarily dependent on hepatic blood flow
Q15. Which laboratory measure is most useful to adjust dosing for renally eliminated drugs in patients with chronic kidney disease?
- Estimated creatinine clearance (CrCl) or eGFR
- Serum albumin concentration
- Plasma cholinesterase activity
- Hepatic transaminase levels
Correct Answer: Estimated creatinine clearance (CrCl) or eGFR
Q16. Which phase II metabolic reaction most increases drug water solubility to facilitate renal excretion?
- Glucuronidation
- Oxidation by CYP3A4
- Reduction by nitroreductases
- Methylation by COMT
Correct Answer: Glucuronidation
Q17. A drug displays large interindividual variability due to polymorphic metabolism. Which approach is most appropriate to reduce adverse effects?
- Therapeutic drug monitoring and dose individualization
- Switching to a prodrug of the same active moiety
- Assuming average population dose for all patients
- Shortening dosing interval without measuring levels
Correct Answer: Therapeutic drug monitoring and dose individualization
Q18. Which process can actively lower renal drug reabsorption of a weak base in the urine?
- Acidification of urine to enhance ionization and reduce reabsorption
- Administration of a PPI to reduce gastric acidity
- Increasing plasma protein binding to trap drug in plasma
- Giving a bile acid sequestrant to increase enterohepatic recycling
Correct Answer: Acidification of urine to enhance ionization and reduce reabsorption
Q19. Which mathematical relation links half‑life (t1/2), volume of distribution (Vd) and clearance (CL)?
- t1/2 = (0.693 × Vd) / CL
- t1/2 = CL ÷ Vd
- t1/2 = Vd × CL
- t1/2 = Dose ÷ (Vd × CL)
Correct Answer: t1/2 = (0.693 × Vd) / CL
Q20. Which statement describes why highly lipophilic drugs often have prolonged elimination half‑lives?
- They distribute extensively into adipose and tissues (large Vd), reducing plasma concentrations and prolonging elimination
- They are rapidly eliminated unchanged by the kidneys due to strong filtration
- They are rapidly metabolized by first‑pass hepatic enzymes leading to short half‑life
- They cannot cross cell membranes and remain confined to plasma
Correct Answer: They distribute extensively into adipose and tissues (large Vd), reducing plasma concentrations and prolonging elimination

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com