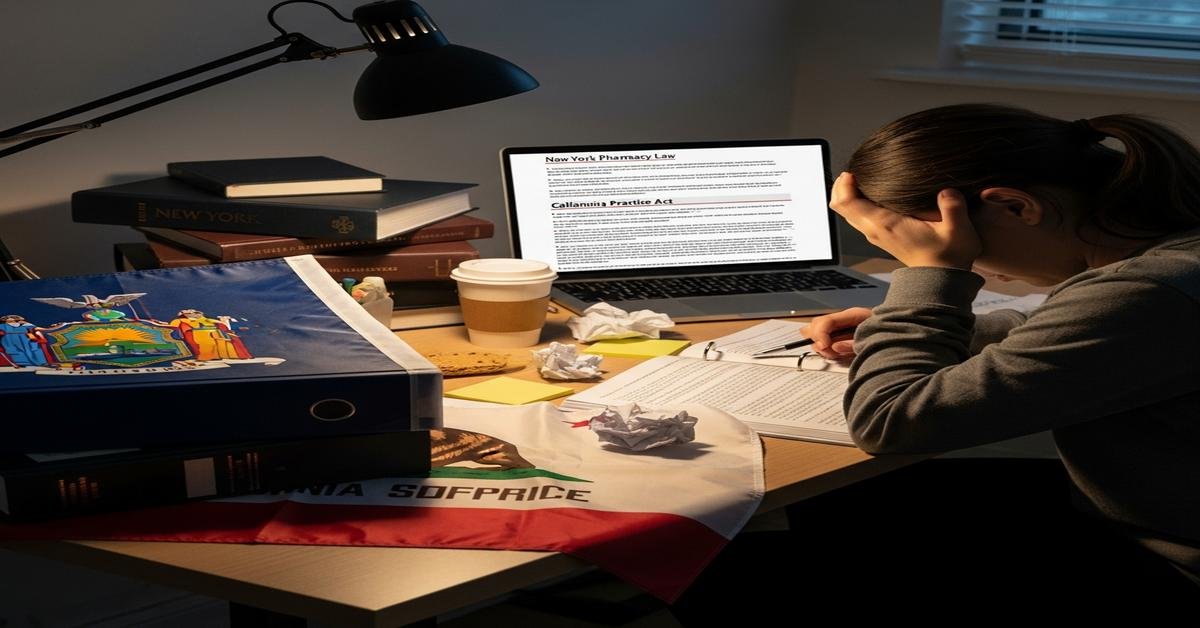
You passed the MPJE in New York and think you’re “good at law.” Then California happens. The rules feel familiar—until the details don’t. California doesn’t even use the MPJE, and its law weaves into clinical practice in ways New York rarely tests. If you walk in with NY habits, you’ll miss questions and make risky calls at the bench. Here’s why, plus the top three legal differences you must re-learn before tackling California.
California vs. New York: Your NY MPJE prep won’t help in CA
California does not use the MPJE. The CPJE is a hybrid exam that mixes clinical judgment with California-specific law. You’ll get scenario questions where the “right” clinical answer is wrong if you miss a California rule (for example, when a pharmacist can independently furnish therapy).
Why this matters: NY prep trains you to recall statutes. CA expects you to operationalize them. The test—and daily practice—punishes you for not knowing how a rule changes workflow, documentation, and patient counseling.
Legal difference #1: Pharmacist scope and independent furnishing
California gives pharmacists broad, protocol-based authority that New York does not broadly grant in community practice. You’re expected to know not just that you “can,” but how you document, educate, and follow up.
- Independent furnishing in CA (no prescriber visit needed):
- Self-administered hormonal contraceptives after a screening tool, blood pressure check (when needed), counseling, and documentation.
- Naloxone (various formulations) to patients or caregivers; counseling and device training required.
- Nicotine replacement therapy products with assessment and tobacco cessation counseling.
- Travel medications for routine self-administered prophylaxis under protocol.
- HIV PrEP and PEP in limited quantities with required screenings, labs, counseling, and follow-up/referral. These are protocol- and documentation-heavy.
- Ordering/assessing CLIA-waived tests related to drug therapy management (for example, A1c to support diabetes medication management), with results used to adjust therapy under allowable authority.
- Immunizations: pharmacists may administer ACIP-recommended vaccines generally starting at age 3 and older, with training, reporting, and PCP notification requirements.
- New York is narrower in community settings:
- Collaborative Drug Therapy Management (CDTM) is largely confined to hospitals and certain affiliated clinics with physician agreements. Community-wide independent furnishing (for PrEP/PEP or contraceptives) is not broadly authorized statewide; availability hinges on specific standing orders or limited programs.
- Immunizations are permitted for adults for many ACIP vaccines; influenza can be given to certain minors (younger pediatric routine vaccines remain more restricted than California).
Exam traps to expect in CA: furnish vs. refer decisions; screening tools; what must be on the patient fact sheet; required documentation elements; and when to notify the patient’s prescriber. New York tests “can you do it?” California tests “can you do it correctly, end-to-end?”
Legal difference #2: Controlled substances — PDMP, opioid limits, and e‑prescribing
Both states are strict, but in different ways. If you memorize one state’s workflow and apply it to the other, you’ll get procedures and timelines wrong.
- PDMP use
- California (CURES): Prescribers must check CURES before initially prescribing Schedule II–IV to a patient and then periodically (commonly every four months) if therapy continues. Pharmacists are not universally required to check CURES before dispensing, but pharmacies must report dispensing of Schedule II–V to CURES, typically by the next business day.
- New York (I-STOP/PMP): Prescribers must consult the PMP before issuing most Schedule II–IV prescriptions. Pharmacists are encouraged but not broadly mandated to check; pharmacies must report dispensing, generally within 24 hours.
- Initial opioid supply for acute pain
- New York: Initial opioid prescriptions for acute pain are capped at a 7-day supply. Dispensing beyond that requires a new prescription.
- California: No statewide day-supply cap specific to acute pain. Risk management relies on prescriber CURES checks, counseling, and clinical judgment. Health plans or systems may impose their own limits, but that’s not state law.
- E-prescribing mandates and paper exceptions
- Both states: E-prescribing is the rule for all prescriptions, including controlled substances. Paper is the exception and must be justified.
- California: If a paper controlled-substance prescription is allowed due to a valid exception (for example, temporary tech failure), it must be on a California-compliant security form with a unique serial number/barcode.
- New York: Under an exception, controlled-substance prescriptions must use New York’s official serialized prescription forms. Prescribers must document the exception reason. Expect tighter documentation scrutiny.
- Why this matters on exams and at the bench
- “Printer broke” is a valid eRx exception if properly documented. “Doctor prefers paper” is not—in either state.
- NY’s 7-day acute opioid cap changes what you can dispense on Day 1. The same patient in CA could lawfully receive more if the prescription is appropriate and all other rules are met.
- PDMP timelines differ. In CA, know the prescriber’s periodic CURES check expectation; in NY, think “before most CS II–IV scripts.”
Legal difference #3: Dispensing, labeling, and records — California is stricter in surprising ways
California’s “patient-centered” label rules and documentation requirements are exam favorites. New York has robust rules too, but not the same emphasis.
- Patient-centered labels (California)
- Critical items—patient name, drug name/strength, directions, and purpose (if provided)—must be highlighted and printed in at least 12-point sans-serif type. About half the label surface should prioritize these items.
- Pharmacies must make interpreter services and translated directions available in common languages, with posted notices. You are expected to know what must be offered and what must be documented if declined.
- Counseling requirements
- California: A verbal consultation is required for new prescriptions and for changes in therapy, unless the patient refuses. The refusal must be documented.
- New York: An offer to counsel is required for new prescriptions. Actual counseling occurs if the patient accepts; documentation standards are less prescriptive than California’s “must counsel unless refused.”
- Record retention
- California: Most prescription and dispensing records must be kept for at least 3 years (note federal DEA rules still apply for controlled records, but California commonly exceeds federal minimums).
- New York: Pharmacies must retain prescription records for at least 5 years. This longer window drives audit exposure and is a common NY test point.
- Why you get burned if you mix them up
- In California, failing to provide mandatory verbal counseling—or to document refusal—can be a violation even when the drug is dispensed correctly.
- In New York, assume auditors can look back five years; your documentation depth must match the longer retention period.
How to re-learn fast for California
- Study by workflow, not statute. Map out exactly how you would furnish contraceptives, naloxone, PrEP/PEP, and travel meds. Include screening, counseling, labeling, PCP notification, and records.
- Drill PDMP/eRx scenarios. For each case, ask: Who must check CURES? Is a paper script permitted? What form features are required? What do I document?
- Memorize CA’s labeling and counseling triggers. Know the 12-point rule, what counts as “new” therapy, and refusal documentation.
- Create “NY vs. CA” flash pairs. Example: “NY acute opioid cap = 7 days” versus “CA = no state cap; rely on CURES + clinical judgment.”
- Practice CPJE-style stems. When a question looks clinical, ask yourself, “Is there a California law twist?” If yes, answer changes.
Mini-drills to test yourself
- Scenario 1: A 24-year-old requests oral contraceptives without a prescriber visit. What changes in CA vs. NY?
- California: You may furnish after a screening questionnaire, BP check as appropriate, counseling on risks/benefits, and documentation. Provide a fact sheet and arrange follow-up.
- New York: Community-wide independent furnishing is not broadly authorized; patient generally needs a prescription unless a specific standing order or program applies.
- Scenario 2: First-time oxycodone for acute ankle sprain.
- New York: Initial fill limited to 7-day supply; prescriber must consult the PMP before issuing.
- California: No 7-day cap; prescriber must check CURES at initiation. You verify legitimacy, apply red flags screening, and proceed if appropriate.
- Scenario 3: Clinic’s eRx system is down for 3 hours; they issue paper scripts for hydrocodone.
- California: Paper may be used under the temporary failure exception, but it must be on a CA-compliant security form with a unique serial number/barcode. Document the exception.
- New York: Paper may be used under an exception with documentation; the prescriber must use NY’s official serialized forms. Your pharmacy must report dispensing to the PMP on time.
Bottom line: New York trains you to follow tight controlled-substance oversight and broad immunization rules. California expects you to act as a front-line clinician under state protocols—and to prove it with documentation, labeling, and counseling. If you don’t relearn those details, your New York “law muscle” becomes a liability in California.

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com