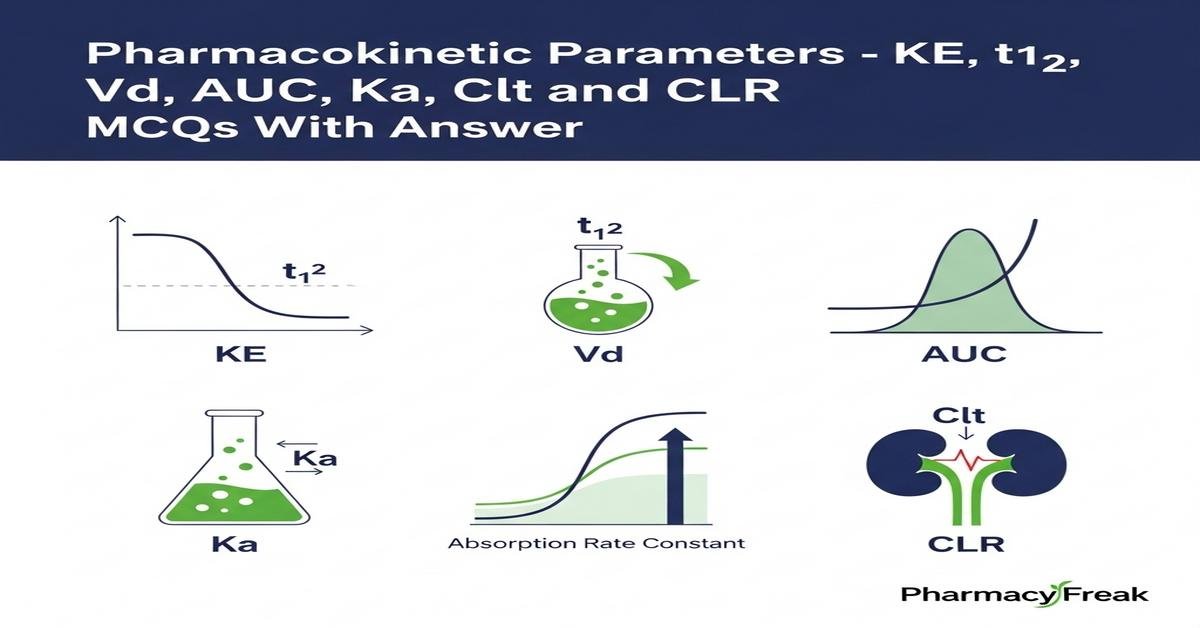
Pharmacokinetic parameters such as KE, t½, Vd, AUC, Ka, Clt and CLR form the quantitative foundation for drug dosing, therapeutic monitoring, and formulation design. B.Pharm students must grasp elimination rate constant (KE) and half‑life (t½) to predict drug persistence; volume of distribution (Vd) to infer tissue distribution; absorption rate constant (Ka) to assess onset of effect; area under the curve (AUC) for systemic exposure; total clearance (Clt) and renal clearance (CLR) for dose adjustments in renal or hepatic impairment. This concise, focused review emphasizes definitions, units, interrelationships, calculation methods, and clinical implications to strengthen problem‑solving skills. Now let’s test your knowledge with 30 MCQs on this topic.
Q1. What is the correct relationship between elimination rate constant (KE) and half‑life (t½)?
- KE = t½ / 0.693
- KE = 0.693 / t½
- t½ = KE / 0.693
- t½ = KE × 0.693
Correct Answer: KE = 0.693 / t½
Q2. Which unit is most appropriate for the elimination rate constant (KE)?
- mg·h/L
- L/kg
- h⁻¹
- mL/min
Correct Answer: h⁻¹
Q3. Volume of distribution (Vd) is best described as:
- The physical volume of plasma in the body
- Theoretical volume that relates amount of drug in body to plasma concentration
- The volume of urine excreted per hour
- The volume of the central compartment only
Correct Answer: Theoretical volume that relates amount of drug in body to plasma concentration
Q4. Which equation defines Vd for a drug when total amount in the body (A) and plasma concentration (Cp) are known?
- Vd = Cp / A
- Vd = A × Cp
- Vd = A / Cp
- Vd = A × ln Cp
Correct Answer: Vd = A / Cp
Q5. Area under the plasma concentration–time curve (AUC) primarily measures:
- Rate of absorption only
- Total systemic exposure to the drug
Correct Answer: Total systemic exposure to the drug
Q6. For an IV bolus dose, total clearance (Clt) can be calculated as:
- Clt = Dose / AUC
- Clt = AUC / Dose
- Clt = Vd × KE
- Clt = Vd / KE
Correct Answer: Clt = Dose / AUC
Q7. Which statement about renal clearance (CLR) is true?
- CLR always equals total clearance
- CLR = (Urine concentration × Urine flow) / Plasma concentration
- CLR is independent of urine flow rate
- CLR has units of mg/L
Correct Answer: CLR = (Urine concentration × Urine flow) / Plasma concentration
Q8. The absorption rate constant (Ka) primarily affects which pharmacokinetic parameter?
- Half‑life (t½) only
- Onset of plasma concentration increase after extravascular dosing
- Total clearance (Clt)
- Volume of distribution (Vd)
Correct Answer: Onset of plasma concentration increase after extravascular dosing
Q9. If a drug has a large Vd, this implies:
- Drug is mostly confined to plasma
- Drug extensively distributes into tissues
- Drug is rapidly eliminated by kidneys
- Drug has low lipid solubility
Correct Answer: Drug extensively distributes into tissues
Q10. The relationship between clearance (Clt), Vd and KE is:
- Clt = Vd / KE
- Clt = Vd × KE
- Ke = Clt + Vd
- Vd = Clt / KE
Correct Answer: Clt = Vd × KE
Q11. For oral dosing, which parameter directly influences bioavailability (F)?
- Ka only
- First‑pass metabolism and absorption processes
- Vd alone
- KE only
Correct Answer: First‑pass metabolism and absorption processes
Q12. At steady state, the average steady‑state concentration (Css,avg) is determined by:
- Css,avg = Dose / Vd
- Css,avg = Infusion rate / Clt
- Css,avg = Ka / Ke
- Css,avg = AUC × Vd
Correct Answer: Css,avg = Infusion rate / Clt
Q13. Which formula gives the loading dose for achieving a target plasma concentration (Cp,target) assuming known bioavailability (F)?
- Loading dose = Cp,target × Vd × F
- Loading dose = Cp,target × Vd / F
- Loading dose = Cp,target / (Vd × F)
- Loading dose = Clt × Cp,target / F
Correct Answer: Loading dose = Cp,target × Vd / F
Q14. Fraction excreted unchanged in urine (fe) can be calculated by:
- fe = CLR / Clt
- fe = Clt / CLR
- fe = AUC urine / AUC plasma
- fe = Vd × KE
Correct Answer: fe = CLR / Clt
Q15. Which method is used to estimate Ke from plasma concentration–time data after IV bolus?
- Plot Cp versus time and measure peak height
- Plot ln Cp versus time and take negative slope
- Calculate area under the curve only
- Measure urine output over 24 hours
Correct Answer: Plot ln Cp versus time and take negative slope
Q16. AUC0–∞ is calculated as AUC0–t + C(t)/KE. What does C(t)/KE represent?
- Error term that should be ignored
- Residual area from last measurable concentration to infinity
- Volume of distribution at time t
- Clearance divided by dose
Correct Answer: Residual area from last measurable concentration to infinity
Q17. In a one‑compartment model with first‑order elimination, doubling the dose will:
- Double the AUC and double Cmax (for IV bolus)
- Halve the AUC and halve Cmax
- Change Ke
- Change Vd
Correct Answer: Double the AUC and double Cmax (for IV bolus)
Q18. Which scenario describes “flip‑flop” kinetics?
- Ke much greater than Ka so absorption is faster than elimination
- Ka much less than Ke so observed terminal phase reflects absorption
- Vd is extremely small
- Clearance increases with dose
Correct Answer: Ka much less than Ke so observed terminal phase reflects absorption
Q19. Which parameter is most useful to compare systemic exposure between two formulations?
- Ka only
- Cmax only
- AUC
- t½ only
Correct Answer: AUC
Q20. If renal function declines, which pharmacokinetic parameter is most directly affected?
- Vd
- Clt and especially CLR
- Ka
- Protein binding only
Correct Answer: Clt and especially CLR
Q21. Clearance (Clt) is best defined as:
- The fraction of drug eliminated per hour
- The theoretical volume of plasma cleared of drug per unit time
- Total urine volume produced per hour
- Time required to eliminate 50% of drug
Correct Answer: The theoretical volume of plasma cleared of drug per unit time
Q22. Which of the following affects AUC after an extravascular dose?
- Bioavailability (F)
- Absorption rate (Ka) only
- Vd only
- Elimination rate constant (KE) only
Correct Answer: Bioavailability (F)
Q23. For a first‑order elimination drug, how many half‑lives are required to reach ~94% of steady state after continuous infusion?
- 1 half‑life
- 3 half‑lives
- 10 half‑lives
- 20 half‑lives
Correct Answer: 3 half‑lives
Q24. Which equation links maintenance infusion rate (R) to target Css and clearance?
- R = Css × Vd
- R = Css × Clt
- R = Css / Clt
- R = AUC / Css
Correct Answer: R = Css × Clt
Q25. If CLR equals Clt for a drug, this indicates:
- Drug is cleared exclusively by renal excretion unchanged
- Drug is highly metabolized by liver
- Drug has very large Vd
- Drug undergoes extensive protein binding
Correct Answer: Drug is cleared exclusively by renal excretion unchanged
Q26. The primary clinical importance of knowing t½ is to:
- Decide dose frequency and estimate time to steady state
- Calculate urine concentration
- Determine bioavailability directly
- Measure protein binding
Correct Answer: Decide dose frequency and estimate time to steady state
Q27. Which scenario will reduce renal clearance (CLR) of a drug eliminated by glomerular filtration?
- Increased glomerular filtration rate (GFR)
- Severe renal impairment lowering GFR
- Increased urine flow without changing plasma levels
- Decreased protein binding increasing free fraction
Correct Answer: Severe renal impairment lowering GFR
Q28. AUC is directly proportional to which of the following after an IV bolus?
- Dose / Clearance
- Clearance / Dose
- Vd × Ka
- t½ × Ka
Correct Answer: Dose / Clearance
Q29. What does a high Ka relative to Ke typically produce after oral dosing?
- Delayed Tmax and low Cmax
- Faster absorption with earlier Tmax and higher Cmax
- Flip‑flop kinetics
- Lower AUC
Correct Answer: Faster absorption with earlier Tmax and higher Cmax
Q30. Which practical step helps adjust dosing when Clt is decreased?
- Increase dose without changing interval
- Reduce dose or extend dosing interval to avoid accumulation
- Ignore renal function since Vd compensates
- Always switch to oral dosing
Correct Answer: Reduce dose or extend dosing interval to avoid accumulation

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com