Introduction:
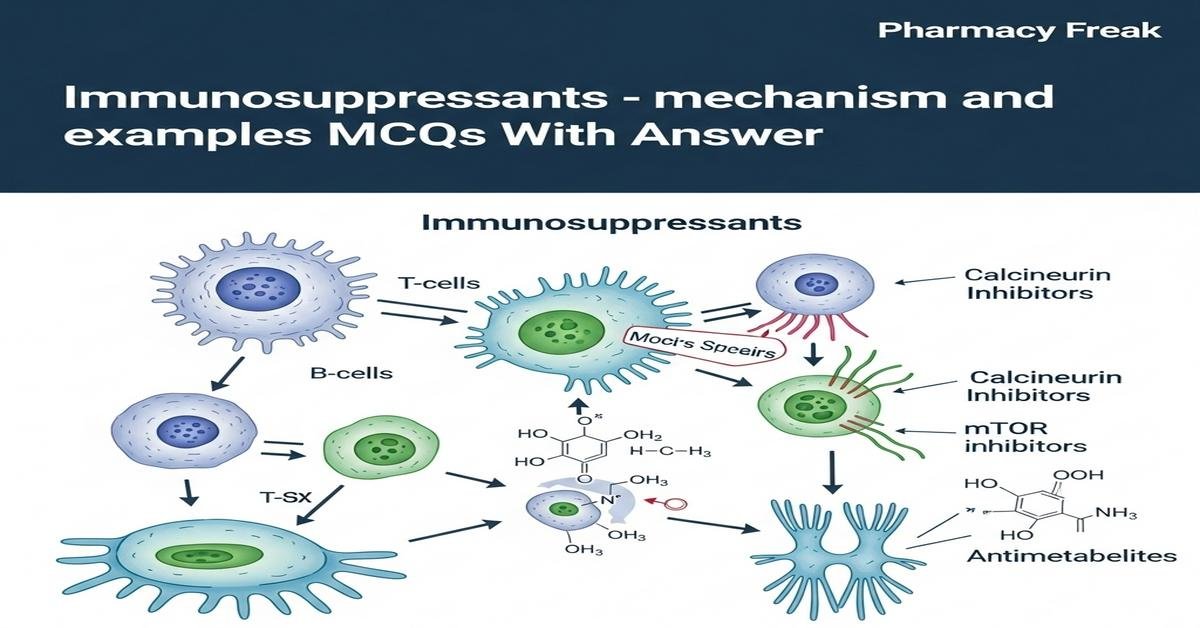
Immunosuppressants are drugs that reduce immune system activity to prevent transplant rejection and treat autoimmune diseases. Understanding mechanisms—such as calcineurin inhibition (cyclosporine, tacrolimus), mTOR blockade (sirolimus), antimetabolite action (azathioprine, mycophenolate), alkylation (cyclophosphamide), and targeted biologics (rituximab, basiliximab)—is essential for B. Pharm students. Key concepts include pharmacokinetics, therapeutic drug monitoring, adverse effects (nephrotoxicity, myelosuppression, infections), drug interactions (CYP3A4 substrates), and monitoring strategies. This topic links mechanism to clinical use and safety. Now let’s test your knowledge with 30 MCQs on this topic.
Q1. Which enzyme is directly inhibited by calcineurin inhibitors leading to reduced IL-2 transcription?
- Protein kinase A
- Calcineurin phosphatase
- DNA-dependent RNA polymerase
- Mammalian target of rapamycin (mTOR)
Correct Answer: Calcineurin phosphatase
Q2. Which immunosuppressant is primarily metabolized by CYP3A4 and often requires therapeutic drug monitoring due to a narrow therapeutic index?
- Mycophenolate mofetil
- Azathioprine
- Tacrolimus
- Methotrexate
Correct Answer: Tacrolimus
Q3. Mycophenolate mofetil exerts its immunosuppressive effect mainly by inhibiting which enzyme?
- Dihydrofolate reductase (DHFR)
- Inosine monophosphate dehydrogenase (IMPDH)
- Xanthine oxidase
- Thymidylate synthase
Correct Answer: Inosine monophosphate dehydrogenase (IMPDH)
Q4. Which adverse effect is most characteristically associated with calcineurin inhibitors like cyclosporine and tacrolimus?
- Pulmonary fibrosis
- Nephrotoxicity
- Ototoxicity
- Pancreatitis
Correct Answer: Nephrotoxicity
Q5. Sirolimus (rapamycin) primarily inhibits which intracellular pathway?
- JAK-STAT signaling
- mTOR signaling
- NF-κB activation
- Calcineurin pathway
Correct Answer: mTOR signaling
Q6. Azathioprine is a prodrug converted to which active metabolite that interferes with purine synthesis?
- 6-Mercaptopurine (6-MP)
- 5-Fluorouracil (5-FU)
- 6-Thioguanine nucleotide (6-TG)
- Allopurinol
Correct Answer: 6-Mercaptopurine (6-MP)
Q7. Which enzymatic polymorphism increases risk of azathioprine toxicity due to reduced metabolism of thiopurines?
- CYP2D6 polymorphism
- Thiopurine S-methyltransferase (TPMT) deficiency
- UDP-glucuronosyltransferase (UGT) deficiency
- Monoamine oxidase (MAO) deficiency
Correct Answer: Thiopurine S-methyltransferase (TPMT) deficiency
Q8. Which antibody targets CD20 on B cells and is used for autoimmune diseases and some transplant protocols?
- Basiliximab
- Rituximab
- Tocilizumab
- Infliximab
Correct Answer: Rituximab
Q9. Basiliximab acts by blocking which receptor on activated T cells?
- CD3 receptor
- CTLA-4
- IL-2 receptor alpha (CD25)
- TNF-α receptor
Correct Answer: IL-2 receptor alpha (CD25)
Q10. Which immunosuppressant commonly causes hyperlipidemia as a notable side effect?
- Cyclosporine
- Sirolimus
- Azathioprine
- Mycophenolate mofetil
Correct Answer: Sirolimus
Q11. Which drug class prevents lymphocyte proliferation by antagonizing folate metabolism?
- Antimetabolites like methotrexate
- Calcineurin inhibitors like tacrolimus
- mTOR inhibitors like sirolimus
- Monoclonal antibodies like rituximab
Correct Answer: Antimetabolites like methotrexate
Q12. Belatacept prevents T-cell activation by interfering with which co-stimulatory signal?
- CD28–CD80/86 interaction
- IL-2 binding to IL-2R
- TNF-α signaling
- TCR-MHC interaction
Correct Answer: CD28–CD80/86 interaction
Q13. Which of the following is a sphingosine-1-phosphate (S1P) receptor modulator that sequesters lymphocytes in lymph nodes?
- Fingolimod
- Tofacitinib
- Azathioprine
- Cyclosporine
Correct Answer: Fingolimod
Q14. Which adverse effect is most associated with alkylating agent cyclophosphamide?
- Hemorrhagic cystitis
- Cardiotoxicity
- Pulmonary fibrosis
- Peripheral neuropathy
Correct Answer: Hemorrhagic cystitis
Q15. Which monitoring parameter is most appropriate for tacrolimus dosing adjustment?
- Random plasma glucose
- Trough blood concentration (C0)
- Peak plasma concentration (Cmax) only
- Urinary creatinine
Correct Answer: Trough blood concentration (C0)
Q16. Tofacitinib, used in autoimmune disorders, acts by inhibiting which pathway?
- mTOR pathway
- JAK-STAT signaling
- Calcineurin phosphatase
- TNF-α production
Correct Answer: JAK-STAT signaling
Q17. Which pair of drugs are both calcineurin inhibitors?
- Cyclosporine and tacrolimus
- Sirolimus and everolimus
- Azathioprine and mycophenolate
- Rituximab and basiliximab
Correct Answer: Cyclosporine and tacrolimus
Q18. A major infectious risk in patients on long-term immunosuppression is reactivation of which latent infection?
- Varicella-zoster virus
- Human papillomavirus only
- Norovirus
- Rhinovirus
Correct Answer: Varicella-zoster virus
Q19. Which immunosuppressant is associated with gingival hyperplasia and hirsutism?
- Mycophenolate mofetil
- Cyclosporine
- Sirolimus
- Azathioprine
Correct Answer: Cyclosporine
Q20. Which drug’s interaction with allopurinol can increase risk of myelosuppression when co-administered?
- Methotrexate
- Azathioprine
- Cyclosporine
- Sirolimus
Correct Answer: Azathioprine
Q21. In organ transplantation, which regimen is commonly used as induction immunosuppression?
- Single-agent mycophenolate only
- High-dose corticosteroids with basiliximab or anti-thymocyte globulin
- Oral methotrexate alone
- Low-dose azathioprine only
Correct Answer: High-dose corticosteroids with basiliximab or anti-thymocyte globulin
Q22. Which biologic blocks TNF-α and is used in autoimmune diseases like rheumatoid arthritis?
- Infliximab
- Tocilizumab
- Basiliximab
- Belatacept
Correct Answer: Infliximab
Q23. Which immunosuppressive drug class carries a significant risk of progressive multifocal leukoencephalopathy (PML)?
- Anti-CD20 monoclonal antibodies (e.g., rituximab)
- Calcineurin inhibitors only
- mTOR inhibitors only
- Alkylating agents only
Correct Answer: Anti-CD20 monoclonal antibodies (e.g., rituximab)
Q24. Which statement about sirolimus is TRUE?
- It is highly nephrotoxic in therapeutic doses
- It inhibits T-cell proliferation by blocking mTOR
- It enhances IL-2 production
- It directly inhibits calcineurin
Correct Answer: It inhibits T-cell proliferation by blocking mTOR
Q25. Which monitoring is most important for patients on long-term azathioprine therapy?
- Complete blood count for myelosuppression
- ECG monthly
- Liver ultrasound monthly
- Fasting blood glucose weekly
Correct Answer: Complete blood count for myelosuppression
Q26. Which immunosuppressant is contraindicated with live vaccines due to risk of uncontrolled replication?
- Short course topical corticosteroids
- Any significant systemic immunosuppressant such as rituximab or high-dose corticosteroids
- Low-dose aspirin
- Vitamin D supplementation
Correct Answer: Any significant systemic immunosuppressant such as rituximab or high-dose corticosteroids
Q27. Everolimus is most closely related to which other immunosuppressant and shares a similar mechanism?
- Tacrolimus
- Sirolimus
- Azathioprine
- Mycophenolate mofetil
Correct Answer: Sirolimus
Q28. Which immunosuppressive agent requires attention to drug interactions with grapefruit juice due to CYP3A4 inhibition?
- Azathioprine
- Tacrolimus
- Mycophenolate mofetil
- Methotrexate
Correct Answer: Tacrolimus
Q29. Which is the primary therapeutic rationale for combining multiple immunosuppressants in transplant regimens?
- To increase cost and complexity
- To achieve synergistic immunosuppression at lower individual drug doses and reduce toxicity
- To target only B cells
- To avoid monitoring drug levels
Correct Answer: To achieve synergistic immunosuppression at lower individual drug doses and reduce toxicity
Q30. Which adverse effect is common to many systemic immunosuppressants and requires vigilant monitoring?
- Increased susceptibility to infections
- Excessive hair growth only
- Heightened wound healing
- Reduced risk of malignancy
Correct Answer: Increased susceptibility to infections

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com