Introduction
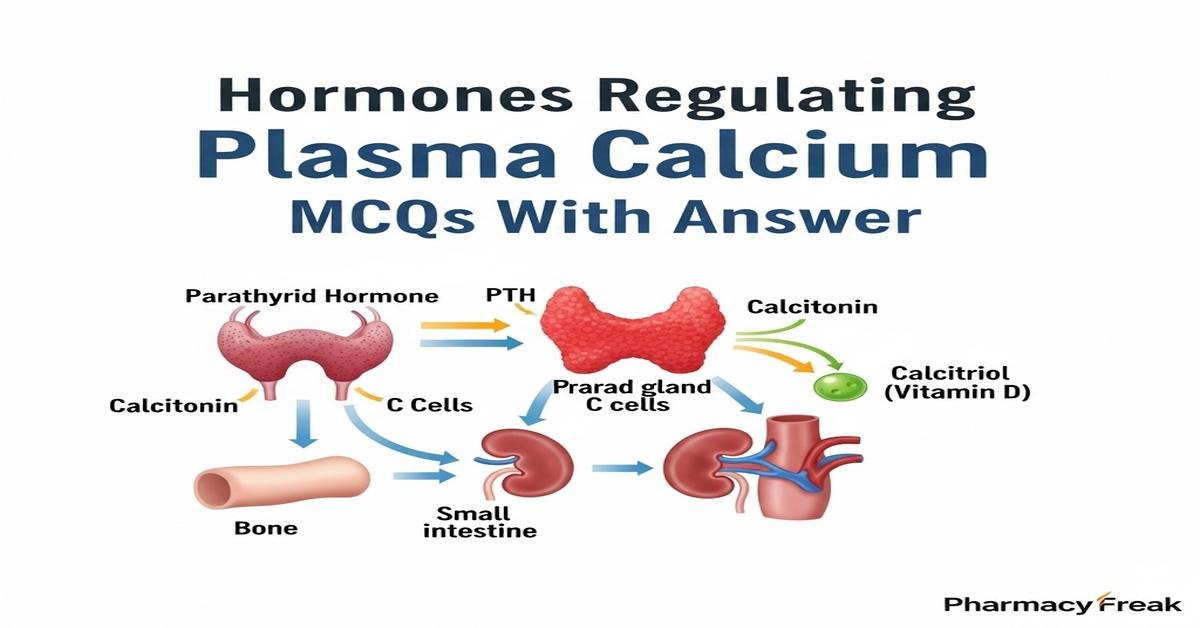
Understanding hormones regulating plasma calcium is essential for B. Pharm students studying physiology and pharmacotherapy. This concise overview covers key regulators—parathyroid hormone (PTH), calcitonin, and active vitamin D (calcitriol)—and their actions on bone resorption, renal calcium reabsorption, intestinal absorption, and signaling pathways like the PTH receptor and vitamin D receptor. Clinical correlations include hypocalcemia, hypercalcemia, osteoporosis, and drug targets such as bisphosphonates, calcimimetics, and vitamin D analogs. Mastering mechanisms, feedback loops, and laboratory markers (serum Ca2+, PTH, 25‑OH and 1,25‑(OH)2 vitamin D) prepares you for therapeutics and toxicities. Now let’s test your knowledge with 30 MCQs on this topic.
Q1. Which hormone primarily increases plasma calcium by stimulating osteoclast-mediated bone resorption?
- Calcitonin
- Parathyroid hormone (PTH)
- Insulin
- Aldosterone
Correct Answer: Parathyroid hormone (PTH)
Q2. Where is calcitonin produced?
- Parathyroid chief cells
- Thyroid parafollicular (C) cells
- Adrenal medulla chromaffin cells
- Pancreatic beta cells
Correct Answer: Thyroid parafollicular (C) cells
Q3. Which form of vitamin D is the hormonally active form that increases intestinal calcium absorption?
- Vitamin D2 (ergocalciferol)
- 25-hydroxyvitamin D
- 1,25-dihydroxyvitamin D (calcitriol)
- Cholecalciferol
Correct Answer: 1,25-dihydroxyvitamin D (calcitriol)
Q4. PTH acts on the kidney to increase calcium reabsorption in which segment of the nephron?
- Proximal tubule exclusively
- Thick ascending limb and distal convoluted tubule
- Collecting duct principal cells only
- Loop of Henle thin segment
Correct Answer: Thick ascending limb and distal convoluted tubule
Q5. Which receptor mediates most of PTH’s effects on target cells?
- Vitamin D receptor (VDR)
- PTH1 receptor (PTH1R)
- Calcium-sensing receptor (CaSR)
- Calcitonin receptor
Correct Answer: PTH1 receptor (PTH1R)
Q6. Activation of the calcium-sensing receptor (CaSR) on parathyroid cells leads to which effect?
- Increased PTH secretion
- Inhibition of PTH secretion
- Increased calcitriol synthesis
- Stimulation of osteoclastogenesis
Correct Answer: Inhibition of PTH secretion
Q7. Which of the following decreases plasma calcium concentration rapidly?
- Parathyroid hormone release
- Calcitonin administration
- Calcitriol synthesis
- Bone resorption
Correct Answer: Calcitonin administration
Q8. Secondary hyperparathyroidism is most commonly caused by chronic disease of which organ?
- Liver
- Kidney
- Thyroid
- Pancreas
Correct Answer: Kidney
Q9. Which laboratory pattern is typical of primary hyperparathyroidism?
- Low serum Ca2+, low PTH
- High serum Ca2+, high PTH
- High serum Ca2+, low PTH
- Normal serum Ca2+, high calcitonin
Correct Answer: High serum Ca2+, high PTH
Q10. Which drug class directly inhibits osteoclast-mediated bone resorption to lower plasma calcium?
- Bisphosphonates
- Loop diuretics
- Thiazide diuretics
- Beta blockers
Correct Answer: Bisphosphonates
Q11. Which enzyme in the kidney converts 25-hydroxyvitamin D to active 1,25-dihydroxyvitamin D?
- CYP27B1 (1-alpha-hydroxylase)
- CYP24A1 (24-hydroxylase)
- Renin
- Alkaline phosphatase
Correct Answer: CYP27B1 (1-alpha-hydroxylase)
Q12. Which condition increases PTH secretion despite normal calcium via reduced receptor sensitivity?
- Familial hypocalciuric hypercalcemia (CaSR mutation)
- Vitamin D intoxication
- Primary hypoparathyroidism
- Excess calcitonin
Correct Answer: Familial hypocalciuric hypercalcemia (CaSR mutation)
Q13. Calcitriol increases plasma calcium primarily by which mechanism?
- Direct stimulation of osteoclast differentiation only
- Increasing intestinal absorption of calcium and phosphate
- Inhibiting renal calcium reabsorption
- Stimulating calcitonin release
Correct Answer: Increasing intestinal absorption of calcium and phosphate
Q14. Which ion transport modification in the kidney does PTH promote to reduce urinary calcium loss?
- Decrease in TRPV5 expression in distal nephron
- Increase in apical TRPV5 channels in distal tubule
- Inhibition of Na+/K+ ATPase in proximal tubule
- Activation of aquaporin channels
Correct Answer: Increase in apical TRPV5 channels in distal tubule
Q15. Which hormone has the opposite effect to PTH on bone calcium mobilization?
- Calcitonin
- Aldosterone
- Growth hormone
- Catecholamines
Correct Answer: Calcitonin
Q16. High phosphate intake or retention affects PTH and vitamin D how?
- Decreases PTH and increases calcitriol
- Stimulates PTH secretion and reduces calcitriol synthesis
- No effect on PTH or vitamin D
- Directly increases calcitonin release
Correct Answer: Stimulates PTH secretion and reduces calcitriol synthesis
Q17. Which diagnostic marker best reflects long-term vitamin D status related to calcium regulation?
- 1,25-dihydroxyvitamin D
- 25-hydroxyvitamin D
- Parathyroid hormone
- Calcitonin
Correct Answer: 25-hydroxyvitamin D
Q18. Cinacalcet lowers plasma calcium by acting on which target?
- Vitamin D receptor agonist
- Calcitonin receptor antagonist
- Positive allosteric modulator of CaSR on parathyroid cells
- PTH receptor blocker on bone
Correct Answer: Positive allosteric modulator of CaSR on parathyroid cells
Q19. In hypoparathyroidism, the expected lab findings are:
- Low serum Ca2+, high PTH
- Low serum Ca2+, low PTH
- High serum Ca2+, high PTH
- High serum Ca2+, low PTH
Correct Answer: Low serum Ca2+, low PTH
Q20. Which of these increases bone formation when used pharmacologically and indirectly influences plasma calcium?
- Teriparatide (intermittent PTH analog)
- Continuous high-dose PTH infusion
- Calcitonin therapy daily
- Bisphosphonate overdose
Correct Answer: Teriparatide (intermittent PTH analog)
Q21. Which process does calcitonin primarily inhibit to lower plasma calcium?
- Osteoblast activity
- Osteoclast-mediated bone resorption
- Renal calcium reabsorption
- Intestinal calcium absorption
Correct Answer: Osteoclast-mediated bone resorption
Q22. Which statement about PTH-related peptide (PTHrP) is correct?
- PTHrP has no homology with PTH
- PTHrP can cause hypercalcemia in malignancy via PTH1R activation
- PTHrP reduces bone resorption exclusively
- PTHrP is produced only in the parathyroid gland
Correct Answer: PTHrP can cause hypercalcemia in malignancy via PTH1R activation
Q23. Which is a direct pharmacologic antagonist of PTH action at the receptor level?
- Teriparatide
- Denosumab
- No clinically used direct PTH1R antagonists are widely available
- Calcitriol
Correct Answer: No clinically used direct PTH1R antagonists are widely available
Q24. Rapid correction of severe hypercalcemia often includes which initial therapy to promote renal calcium excretion?
- Oral calcium supplementation
- Intravenous saline hydration and loop diuretics
- Thiazide diuretics
- Subcutaneous calcitriol
Correct Answer: Intravenous saline hydration and loop diuretics
Q25. Which transporter mediates transcellular calcium uptake in intestinal epithelial cells enhanced by calcitriol?
- ENaC
- TRPV6 (calcium channel)
- GLUT2
- Na+/K+ cotransporter
Correct Answer: TRPV6 (calcium channel)
Q26. Which genetic defect leads to hypocalcemia with low PTH due to parathyroid gland failure?
- Mutations in CaSR causing gain of function
- Autoimmune destruction of parathyroid glands
- Excessive PTHrP production
- Vitamin D receptor mutations
Correct Answer: Autoimmune destruction of parathyroid glands
Q27. Chronic use of loop diuretics affects calcium balance how?
- Promotes renal calcium reabsorption and hypercalcemia
- Increases urinary calcium excretion and can lower plasma calcium
- No effect on calcium handling
- Blocks intestinal calcium absorption directly
Correct Answer: Increases urinary calcium excretion and can lower plasma calcium
Q28. Which biomarker increases when bone turnover is high and may correlate with PTH activity?
- Serum albumin
- Alkaline phosphatase (bone isoform)
- Serum sodium
- Serum amylase
Correct Answer: Alkaline phosphatase (bone isoform)
Q29. Excessive vitamin D (calcitriol) leads to hypercalcemia by which combination of effects?
- Decreased intestinal Ca2+ absorption and increased renal loss
- Increased intestinal Ca2+ absorption, increased bone resorption, and increased renal reabsorption
- Only increased PTH secretion
- Exclusive stimulation of calcitonin release
Correct Answer: Increased intestinal Ca2+ absorption, increased bone resorption, and increased renal reabsorption
Q30. In renal failure, impaired 1-alpha hydroxylation causes which cascade affecting calcium?
- Increased calcitriol, hypercalcemia, suppressed PTH
- Decreased calcitriol, hypocalcemia, secondary hyperparathyroidism
- No change in calcium or PTH levels
- Increased calcitonin production only
Correct Answer: Decreased calcitriol, hypocalcemia, secondary hyperparathyroidism

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com