Mechanism of anticonvulsant action MCQs With Answer
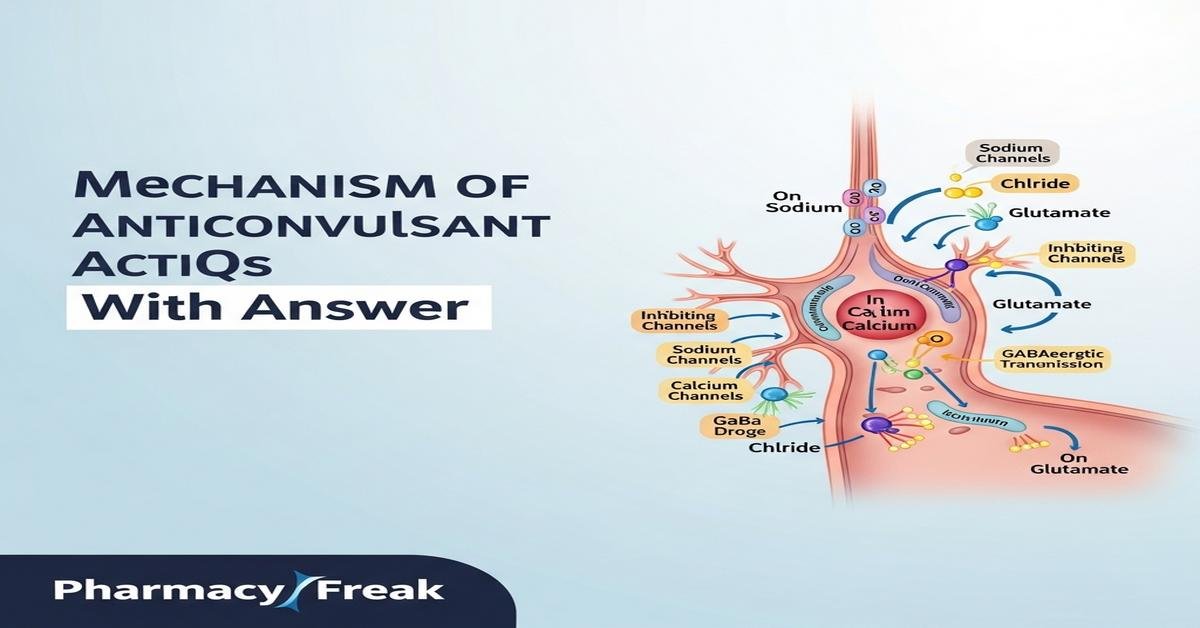
The mechanism of anticonvulsant action is central to understanding how antiepileptic drugs control seizures. This introduction summarizes key mechanisms — sodium and calcium channel blockade, enhancement of GABAergic inhibition, reduction of glutamatergic excitation, modulation of synaptic vesicle proteins, K+ channel opening, and enzyme/transporter effects — that B.Pharm students must master. Concepts such as use‑dependence, slow vs fast inactivation of Na+ channels, T‑type Ca2+ role in absence seizures, and drug resistance mechanisms (P‑gp efflux, CYP induction) are emphasized. Keywords: mechanism of anticonvulsant action, anticonvulsant drugs, antiepileptic mechanisms, GABA, sodium channels, calcium channels, B.Pharm, MCQs. Now let’s test your knowledge with 50 MCQs on this topic.
Q1. Which is the primary mechanism of action of phenytoin?
- Potentiation of GABA-A receptor function
- Blockade of voltage-gated sodium channels
- Binding to synaptic vesicle protein SV2A
- Inhibition of T-type calcium channels
Correct Answer: Blockade of voltage-gated sodium channels
Q2. Ethosuximide controls absence seizures mainly by:
- Enhancing GABA synthesis
- Blocking T‑type (low-voltage) calcium channels in thalamic neurons
- Antagonizing AMPA receptors
- Binding to SV2A
Correct Answer: Blocking T‑type (low-voltage) calcium channels in thalamic neurons
Q3. Benzodiazepines (e.g., diazepam) exert anticonvulsant effects by:
- Increasing the duration of GABA-A receptor chloride channel opening
- Blocking voltage-gated sodium channels
- Increasing the frequency of GABA-A receptor chloride channel opening
- Inhibiting glutamate release via SV2A
Correct Answer: Increasing the frequency of GABA-A receptor chloride channel opening
Q4. Barbiturates (e.g., phenobarbital) differ from benzodiazepines because they:
- Increase the frequency of GABA-A channel opening
- Directly block NMDA receptors
- Prolong the duration of GABA-A receptor chloride channel opening and can act as direct agonists at high doses
- Bind SV2A protein
Correct Answer: Prolong the duration of GABA-A receptor chloride channel opening and can act as direct agonists at high doses
Q5. Vigabatrin produces anticonvulsant action by:
- Reversible inhibition of GABA reuptake
- Irreversible inhibition of GABA transaminase (GABA-T)
- Blocking voltage-gated sodium channels
- Binding to SV2A
Correct Answer: Irreversible inhibition of GABA transaminase (GABA-T)
Q6. Tiagabine helps control seizures primarily via:
- Inhibition of glutamate release
- Inhibition of the GABA transporter GAT‑1 (blocking GABA reuptake)
- Opening KCNQ potassium channels
- Blocking T‑type calcium channels
Correct Answer: Inhibition of the GABA transporter GAT‑1 (blocking GABA reuptake)
Q7. Levetiracetam’s anticonvulsant mechanism is mainly due to:
- Inhibition of GABA transaminase
- Binding to the synaptic vesicle protein SV2A and modulating neurotransmitter release
- Noncompetitive antagonism of AMPA receptors
- Opening neuronal K+ channels
Correct Answer: Binding to the synaptic vesicle protein SV2A and modulating neurotransmitter release
Q8. Lamotrigine primarily reduces seizure activity by:
- Enhancing benzodiazepine receptor function
- Blockade of voltage-gated sodium channels and reduction of glutamate release
- Inhibiting carbonic anhydrase
- Binding to GAT-1
Correct Answer: Blockade of voltage-gated sodium channels and reduction of glutamate release
Q9. Gabapentin and pregabalin produce anticonvulsant effects by binding to:
- AMPA receptor subunits
- GABA-A receptor benzodiazepine site
- The α2-δ auxiliary subunit of voltage-gated calcium channels, reducing excitatory neurotransmitter release
- KCNQ potassium channels
Correct Answer: The α2-δ auxiliary subunit of voltage-gated calcium channels, reducing excitatory neurotransmitter release
Q10. Ezogabine (retigabine) exerts anticonvulsant action by:
- Blocking NMDA receptors
- Opening KCNQ (Kv7) voltage-gated potassium channels to stabilize the membrane potential
- Inhibiting GABA uptake
- Enhancing AMPA receptor currents
Correct Answer: Opening KCNQ (Kv7) voltage-gated potassium channels to stabilize the membrane potential
Q11. Perampanel is unique among many AEDs because it:
- Is a competitive NMDA receptor antagonist
- Noncompetitively antagonizes AMPA glutamate receptors
- Enhances GABA synthesis
- Blocks T‑type calcium channels
Correct Answer: Noncompetitively antagonizes AMPA glutamate receptors
Q12. Topiramate’s anticonvulsant mechanisms include all EXCEPT:
- Voltage-gated sodium channel blockade
- Potentiation of GABA-A receptor activity
- Antagonism of AMPA/kainate receptors
- Irreversible inhibition of GABA transaminase
Correct Answer: Irreversible inhibition of GABA transaminase
Q13. Valproate’s anticonvulsant action involves which combination of mechanisms?
- Selective SV2A binding only
- Increasing GABA levels, blocking voltage-gated sodium channels, and inhibiting T‑type calcium channels
- Pure carbonic anhydrase inhibition
- AMPA receptor potentiation
Correct Answer: Increasing GABA levels, blocking voltage-gated sodium channels, and inhibiting T‑type calcium channels
Q14. First-line acute treatment for status epilepticus is usually a drug that:
- Blocks T-type calcium channels
- Enhances GABA-A receptor-mediated inhibition (e.g., IV benzodiazepines)
- Opens KCNQ potassium channels
- Binds SV2A
Correct Answer: Enhances GABA-A receptor-mediated inhibition (e.g., IV benzodiazepines)
Q15. Lacosamide’s anticonvulsant mechanism is characterized by:
- Opening K+ channels
- Enhancing slow inactivation of voltage-gated sodium channels
- Inhibiting GABA transaminase
- Blocking AMPA receptors
Correct Answer: Enhancing slow inactivation of voltage-gated sodium channels
Q16. Rufinamide contributes to seizure control primarily by:
- Prolonging the inactive state of voltage-gated sodium channels
- Binding to SV2A
- Blocking GABA uptake
- Antagonizing AMPA receptors
Correct Answer: Prolonging the inactive state of voltage-gated sodium channels
Q17. Zonisamide has anticonvulsant effects because it:
- Only potentiates benzodiazepine receptors
- Blocks voltage-gated sodium channels and T‑type calcium channels, and weakly inhibits carbonic anhydrase
- Is an opioid receptor agonist
- Irreversibly inhibits GABA transaminase
Correct Answer: Blocks voltage-gated sodium channels and T‑type calcium channels, and weakly inhibits carbonic anhydrase
Q18. Felbamate’s anticonvulsant action includes which important mechanism?
- Selective inhibition of GAT-1
- Antagonism of NMDA receptors and potentiation of GABAergic transmission
- Selective SV2A binding only
- Only T-type calcium channel blockade
Correct Answer: Antagonism of NMDA receptors and potentiation of GABAergic transmission
Q19. Carbamazepine’s sodium channel blockade is best described as:
- Voltage- and use-dependent blockade that stabilizes the inactive state of sodium channels
- Irreversible binding to sodium channels
- Enhancement of sodium channel opening
- Specific blockade of T‑type calcium channels
Correct Answer: Voltage- and use-dependent blockade that stabilizes the inactive state of sodium channels
Q20. Which mechanism contributes to pharmacoresistance in epilepsy?
- Downregulation of P-glycoprotein in the blood–brain barrier
- Overexpression of efflux transporters like P-glycoprotein reducing CNS drug levels
- Increased GABA synthesis in hippocampus
- Higher synaptic SV2A expression increasing drug binding
Correct Answer: Overexpression of efflux transporters like P-glycoprotein reducing CNS drug levels
Q21. Which antiepileptic is most associated with irreversible peripheral visual field defects due to its mechanism?
- Tiagabine
- Vigabatrin (GABA transaminase inhibitor)
- Levetiracetam
- Ethosuximide
Correct Answer: Vigabatrin (GABA transaminase inhibitor)
Q22. Which AED is a strong hepatic enzyme inducer and thereby causes many drug interactions?
- Phenytoin
- Valproate
- Levetiracetam
- Vigabatrin
Correct Answer: Phenytoin
Q23. Which agent increases GABA levels by inhibiting GABA transaminase?
- Gabapentin
- Vigabatrin
- Topiramate
- Perampanel
Correct Answer: Vigabatrin
Q24. The ketogenic diet’s anticonvulsant effects are thought to involve:
- Direct blockade of voltage-gated sodium channels by ketones
- Metabolic changes (ketone bodies) that alter neuronal excitability and increase GABA synthesis
- Binding to SV2A
- Inhibition of carbonic anhydrase only
Correct Answer: Metabolic changes (ketone bodies) that alter neuronal excitability and increase GABA synthesis
Q25. Which AED most directly antagonizes AMPA receptors?
- Perampanel
- Ethosuximide
- Vigabatrin
- Lacosamide
Correct Answer: Perampanel
Q26. Which AED primarily targets absence seizures and is NOT useful for generalized tonic‑clonic seizures?
- Ethosuximide
- Carbamazepine
- Phenytoin
- Phenobarbital
Correct Answer: Ethosuximide
Q27. Brivaracetam differs from levetiracetam mainly by:
- Being a benzodiazepine receptor agonist
- Having higher affinity binding to SV2A than levetiracetam
- Blocking T-type calcium channels
- Inhibiting carbonic anhydrase
Correct Answer: Having higher affinity binding to SV2A than levetiracetam
Q28. Which mechanism best explains how carbonic anhydrase inhibitors (e.g., acetazolamide) reduce seizure activity?
- They directly block voltage-gated sodium channels
- They cause mild metabolic acidosis, which can reduce neuronal excitability
- They increase synaptic glutamate release
- They bind to SV2A
Correct Answer: They cause mild metabolic acidosis, which can reduce neuronal excitability
Q29. Which AED is known to inhibit histone deacetylases (HDAC), a mechanism implicated in teratogenicity?
- Carbamazepine
- Valproate
- Levetiracetam
- Topiramate
Correct Answer: Valproate
Q30. Which combination describes a common adverse pharmacokinetic interaction involving enzyme induction by AEDs?
- Phenytoin induces CYP enzymes leading to decreased plasma concentrations of oral contraceptives
- Levetiracetam induces CYP3A4 causing increased warfarin levels
- Vigabatrin induces CYP2D6 causing increased antidepressant levels
- Ethosuximide inhibits UGT leading to reduced lamotrigine levels
Correct Answer: Phenytoin induces CYP enzymes leading to decreased plasma concentrations of oral contraceptives
Q31. Which drug’s mechanism includes inhibition of presynaptic glutamate release by stabilizing sodium channels and reducing excitatory transmitter release?
- Lamotrigine
- Vigabatrin
- Ethosuximide
- Perampanel
Correct Answer: Lamotrigine
Q32. Which antiepileptic primarily acts by blocking high-frequency repetitive firing via sodium channel stabilization?
- Carbamazepine
- Tiagabine
- Perampanel
- Acetazolamide
Correct Answer: Carbamazepine
Q33. Which agent’s anticonvulsant action is least well defined and involves multiple targets including effects on adenosine and TRPV1 receptors?
- Cannabidiol (CBD)
- Phenytoin
- Ethosuximide
- Carbamazepine
Correct Answer: Cannabidiol (CBD)
Q34. Which AED is particularly useful for generalized myoclonic seizures and acts through multiple mechanisms including increasing GABA?
- Valproate
- Ethosuximide
- Carbamazepine
- Levetiracetam
Correct Answer: Valproate
Q35. Which mechanism explains why some sodium channel blockers are more effective during high-frequency neuronal firing?
- They act only at resting membrane potentials
- Use-dependent (state-dependent) blockade preferentially targets channels during repetitive action potentials
- They increase synaptic glutamate release during high-frequency firing
- They selectively bind to AMPA receptors during high-frequency activity
Correct Answer: Use-dependent (state-dependent) blockade preferentially targets channels during repetitive action potentials
Q36. Which AED can reduce glutamatergic excitation by antagonizing the glycine co-agonist site of NMDA receptors (contributing to efficacy in refractory epilepsy)?
- Felbamate
- Levetiracetam
- Ethosuximide
- Tiagabine
Correct Answer: Felbamate
Q37. Which AED is commonly used as an adjunct in focal seizures and acts by high‑affinity binding to SV2A?
- Topiramate
- Levetiracetam
- Ethosuximide
- Vigabatrin
Correct Answer: Levetiracetam
Q38. Which antiepileptic’s mechanism includes weak inhibition of carbonic anhydrase and is associated with kidney stone risk?
- Topiramate
- Lamotrigine
- Gabapentin
- Perampanel
Correct Answer: Topiramate
Q39. The α2-δ subunit ligands (gabapentin/pregabalin) primarily reduce seizures by:
- Increasing postsynaptic GABA-A sensitivity
- Decreasing calcium influx at presynaptic terminals and reducing neurotransmitter release
- Directly blocking sodium channels
- Potentiating AMPA receptor currents
Correct Answer: Decreasing calcium influx at presynaptic terminals and reducing neurotransmitter release
Q40. Which AED is most associated with significant enzyme inhibition that raises levels of co-administered drugs such as lamotrigine?
- Phenytoin
- Valproate
- Carbamazepine
- Phenobarbital
Correct Answer: Valproate
Q41. Which molecular target is directly involved in rapid excitatory synaptic transmission and is a focus for some newer AEDs?
- GABA-B receptors
- AMPA glutamate receptors
- Sodium‑dependent glutamate transporters
- Carbonic anhydrase
Correct Answer: AMPA glutamate receptors
Q42. Which mechanism explains how increased extracellular potassium contributes to seizure propagation?
- Increased extracellular K+ hyperpolarizes neurons, reducing excitability
- Increased extracellular K+ depolarizes neuronal membranes, promoting repetitive firing
- Increased extracellular K+ enhances GABAergic inhibition
- Increased extracellular K+ blocks sodium channels
Correct Answer: Increased extracellular K+ depolarizes neuronal membranes, promoting repetitive firing
Q43. Which AED is particularly effective for infantile spasms (as an option) and exerts effects via GABAergic modulation and neuroendocrine mechanisms?
- Vigabatrin
- Ethosuximide
- Phenytoin
- Perampanel
Correct Answer: Vigabatrin
Q44. Which mechanism best describes how inhibitory interneuron dysfunction can facilitate seizures?
- Loss of inhibitory GABAergic tone increases network excitability and synchronization
- Excessive GABA release causes hyperpolarization and seizures
- Overexpression of SV2A causes neuronal silence
- Enhanced carbonic anhydrase activity reduces pH and prevents seizures
Correct Answer: Loss of inhibitory GABAergic tone increases network excitability and synchronization
Q45. Which AED reduces release of excitatory neurotransmitters by stabilizing presynaptic sodium channels and inhibiting neurotransmitter release machinery?
- Lamotrigine
- Ethosuximide
- Tiagabine
- Acetazolamide
Correct Answer: Lamotrigine
Q46. Which mechanism is a recognized target for novel AEDs aiming to reduce neuronal hyperexcitability by enhancing inhibitory K+ currents?
- Blockade of AMPA receptors
- Opening of KCNQ (Kv7) potassium channels
- Inhibition of GABA synthesis
- Activation of NMDA receptors
Correct Answer: Opening of KCNQ (Kv7) potassium channels
Q47. A patient with Dravet syndrome (SCN1A mutation) typically has worsened seizures with which class of drugs?
- Sodium channel blockers (e.g., carbamazepine, lamotrigine)
- Benzodiazepines
- Valproate
- Clobazam
Correct Answer: Sodium channel blockers (e.g., carbamazepine, lamotrigine)
Q48. Which AED is known to have a major action of reducing presynaptic glutamate release in addition to sodium channel effects and is often used in focal epilepsy?
- Lamotrigine
- Ethosuximide
- Vigabatrin
- Tiagabine
Correct Answer: Lamotrigine
Q49. Which pharmacodynamic principle explains why some antiepileptics preferentially block neurons that are firing rapidly during a seizure?
- Equilibrium-dependent blockade
- Use‑dependence or state‑dependent blockade
- Frequency-independent antagonism
- Competitive receptor blockade only at resting state
Correct Answer: Use‑dependence or state‑dependent blockade
Q50. Which statement best summarizes strategies by which current AEDs suppress seizures?
- Only by enhancing GABAergic transmission
- By modulating ion channels (Na+, Ca2+, K+), enhancing GABAergic inhibition, inhibiting glutamatergic excitation, and altering synaptic release mechanisms
- Only by blocking glutamate receptors
- Only by inhibiting carbonic anhydrase
Correct Answer: By modulating ion channels (Na+, Ca2+, K+), enhancing GABAergic inhibition, inhibiting glutamatergic excitation, and altering synaptic release mechanisms

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com