Anatomy and functions of salivary glands MCQs With Answer
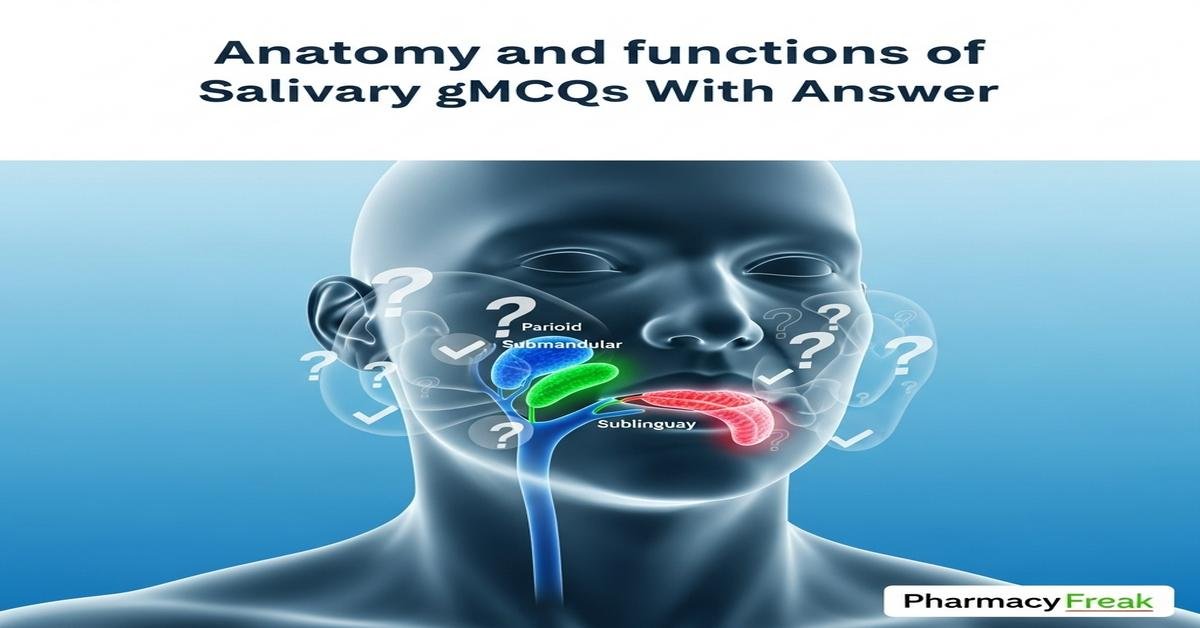
The salivary glands are essential exocrine organs whose anatomy and functions are core topics for B. Pharm students studying oral physiology, drug effects and clinical pharmacology. This concise guide focuses on major glands — parotid, submandibular and sublingual — covering duct anatomy (Stensen’s, Wharton’s, Bartholin’s), histology (serous and mucous acini, ductal cells), neural control (parasympathetic and sympathetic), secretion mechanisms, and saliva composition (amylase, mucins, electrolytes, IgA). Understanding salivary physiology helps predict drug-induced xerostomia, interpret salivary diagnostics and manage infections or sialolithiasis. Targeted MCQs reinforce concepts needed for exams and practical pharmacy applications. Now let’s test your knowledge with 50 MCQs on this topic.
Q1. Which is the largest salivary gland in humans?
- Parotid gland
- Submandibular gland
- Sublingual gland
- Minor salivary glands
Correct Answer: Parotid gland
Q2. The main excretory duct of the parotid gland is known as:
- Wharton’s duct
- Stensen’s duct
- Bartholin’s duct
- Rivinus duct
Correct Answer: Stensen’s duct
Q3. Which duct drains the submandibular gland into the oral cavity?
- Stensen’s duct
- Wharton’s duct
- Bartholin’s duct
- Salivary duct of Rivinus
Correct Answer: Wharton’s duct
Q4. The major sublingual duct that commonly opens into the submandibular duct is called:
- Stensen’s duct
- Rivinus duct
- Bartholin’s duct
- Wharton’s duct
Correct Answer: Bartholin’s duct
Q5. Which major salivary gland is composed almost entirely of serous acini?
- Sublingual gland
- Submandibular gland
- Parotid gland
- Minor mucous glands
Correct Answer: Parotid gland
Q6. Mucous acini in salivary glands primarily secrete:
- Enzyme-rich, watery fluid
- Mucins and glycoproteins for lubrication
- Secretory IgA exclusively
- Purely electrolytic fluid without proteins
Correct Answer: Mucins and glycoproteins for lubrication
Q7. Which enzyme in saliva initiates starch digestion in the oral cavity?
- Lipase
- Pepsin
- Alpha-amylase (ptyalin)
- Trypsin
Correct Answer: Alpha-amylase (ptyalin)
Q8. Lingual lipase, which begins lipid digestion, is secreted by which glands?
- Parotid glands
- Von Ebner’s glands on the tongue
- Submandibular glands
- Sublingual glands
Correct Answer: Von Ebner’s glands on the tongue
Q9. The approximate average daily saliva production in a healthy adult is:
- 50–200 mL/day
- Approximately 1–1.5 L/day
- 3–4 L/day
- Less than 10 mL/day
Correct Answer: Approximately 1–1.5 L/day
Q10. Parasympathetic secretomotor fibers to the parotid gland originate from which cranial nerve?
- Facial nerve (CN VII)
- Glossopharyngeal nerve (CN IX)
- Vagus nerve (CN X)
- Trigeminal nerve (CN V)
Correct Answer: Glossopharyngeal nerve (CN IX)
Q11. Which nerve (via chorda tympani) carries parasympathetic fibers to the submandibular and sublingual glands?
- Trigeminal nerve (CN V)
- Facial nerve (CN VII)
- Glossopharyngeal nerve (CN IX)
- Hypoglossal nerve (CN XII)
Correct Answer: Facial nerve (CN VII)
Q12. Sympathetic stimulation of salivary glands typically produces:
- Large volume of watery saliva
- High-volume, low-protein saliva
- Low-volume, protein-rich viscous saliva
- No change in secretion composition
Correct Answer: Low-volume, protein-rich viscous saliva
Q13. Parasympathetic stimulation of salivary glands results in which effect?
- Decreased saliva flow and increased protein
- Increased watery saliva flow with low protein concentration
- Complete cessation of salivation
- Only mucin secretion without enzymes
Correct Answer: Increased watery saliva flow with low protein concentration
Q14. Ductal cells modify primary saliva by which of the following actions?
- Reabsorbing Na+ and Cl-; secreting K+ and HCO3-
- Secreting large amounts of amylase
- Allowing free water movement to equilibrate osmolarity with plasma
- Producing secretory IgA exclusively
Correct Answer: Reabsorbing Na+ and Cl-; secreting K+ and HCO3-
Q15. Compared to plasma, resting saliva is usually:
- Isotonic with higher Na+ concentration
- Hypertonic with more Cl-
- Hypotonic with lower Na+ and higher K+
- Exactly identical in ionic composition
Correct Answer: Hypotonic with lower Na+ and higher K+
Q16. The principal salivary buffer that increases with stimulated flow is:
- Phosphate
- Proteins
- Bicarbonate
- Urea
Correct Answer: Bicarbonate
Q17. The major immunoglobulin present in saliva that provides mucosal immunity is:
- IgG
- IgM
- Secretory IgA
- IgE
Correct Answer: Secretory IgA
Q18. Which of the following is NOT a primary function of saliva?
- Lubrication and bolus formation for swallowing
- Initiation of carbohydrate digestion
- Providing enzymes for protein digestion in the stomach
- Antimicrobial defense and oral cleansing
Correct Answer: Providing enzymes for protein digestion in the stomach
Q19. Sialolithiasis (salivary stones) most commonly affects which gland?
- Parotid gland
- Submandibular gland
- Sublingual gland
- Labial minor glands
Correct Answer: Submandibular gland
Q20. The most common bacteria implicated in acute bacterial sialadenitis is:
- Streptococcus mutans
- Staphylococcus aureus
- Escherichia coli
- Pseudomonas aeruginosa
Correct Answer: Staphylococcus aureus
Q21. Which class of drugs is most commonly associated with drug-induced xerostomia?
- Beta blockers
- Anticholinergics (antimuscarinics)
- Antibiotics
- Thyroid hormones
Correct Answer: Anticholinergics (antimuscarinics)
Q22. Which major salivary gland is particularly sensitive to radiation, often causing permanent xerostomia when irradiated?
- Sublingual gland
- Minor palatal glands
- Parotid gland
- Submandibular gland
Correct Answer: Parotid gland
Q23. The dominant cellular mechanism of secretion in salivary acinar cells is:
- Apocrine release with part of cell shed
- Holocrine secretion with whole-cell disintegration
- Merocrine exocytosis of secretory granules
- Transcytosis without vesicle fusion
Correct Answer: Merocrine exocytosis of secretory granules
Q24. Which acinar cell type synthesizes and secretes salivary amylase?
- Mucous acinar cells
- Serous acinar cells
- Ductal principal cells
- Myoepithelial cells
Correct Answer: Serous acinar cells
Q25. Arrange the duct segments in the correct order from acinus to oral cavity:
- Excretory → Striated → Intercalated
- Intercalated → Striated → Excretory
- Striated → Intercalated → Excretory
- Intercalated → Excretory → Striated
Correct Answer: Intercalated → Striated → Excretory
Q26. Which duct displays basal striations due to abundant mitochondria and is important for ionic modification?
- Intercalated duct
- Striated duct
- Excretory duct
- Exocrine lobular duct
Correct Answer: Striated duct
Q27. Intercalated ducts are typically lined by which epithelium?
- Stratified squamous epithelium
- Simple cuboidal epithelium
- Pseudostratified columnar epithelium
- Transitional epithelium
Correct Answer: Simple cuboidal epithelium
Q28. Myoepithelial cells in salivary glands function primarily to:
- Secrete IgA into saliva
- Contract to expel saliva from acini
- Absorb sodium from primary secretion
- Produce mucin glycoproteins
Correct Answer: Contract to expel saliva from acini
Q29. The arterial blood supply to the parotid gland is primarily from branches of the:
- External carotid artery
- Internal carotid artery
- Facial artery only
- Vertebral artery
Correct Answer: External carotid artery
Q30. Lymphatic drainage from the parotid gland primarily goes to:
- Superficial and deep cervical lymph nodes
- Axillary lymph nodes
- Inguinal lymph nodes
- Mesenteric lymph nodes
Correct Answer: Superficial and deep cervical lymph nodes
Q31. Which statement about zymogens in saliva is correct?
- Saliva contains large amounts of pepsinogen
- Salivary enzymes are mostly secreted in active forms, not as zymogens
- Trypsinogen is secreted by salivary glands
- Saliva contains inactive lipase zymogens
Correct Answer: Salivary enzymes are mostly secreted in active forms, not as zymogens
Q32. During stimulated salivary flow (e.g., chewing), which ionic change is most marked?
- Decrease in bicarbonate concentration
- Large increase in bicarbonate concentration and pH
- Large increase in plasma-like Na+ concentration making saliva isotonic
- Significant decrease in K+ concentration
Correct Answer: Large increase in bicarbonate concentration and pH
Q33. The glycoproteins primarily responsible for saliva viscosity and lubrication are called:
- Immunoglobulins
- Mucins
- Albumins
- Peptidases
Correct Answer: Mucins
Q34. Saliva aids taste perception primarily by:
- Acting as an enzyme to break down taste receptors
- Dissolving tastants to allow interaction with taste buds
- Neutralizing taste receptor potentials
- Destroying gustatory nerves
Correct Answer: Dissolving tastants to allow interaction with taste buds
Q35. Excessive salivation is termed:
- Xerostomia
- Sialorrhea
- Sialadenitis
- Sialolithiasis
Correct Answer: Sialorrhea
Q36. The embryological origin of the parotid gland is from which germ layer?
- Mesoderm
- Ectoderm (oral ectoderm)
- Endoderm
- Neural crest only
Correct Answer: Ectoderm (oral ectoderm)
Q37. Which major salivary gland is considered purely serous in humans?
- Submandibular gland
- Sublingual gland
- Parotid gland
- Minor labial glands
Correct Answer: Parotid gland
Q38. The submandibular gland is characterized histologically as:
- Purely mucous gland
- Purely serous gland
- Mixed gland with predominantly serous components
- Non-secretory lymphoid tissue
Correct Answer: Mixed gland with predominantly serous components
Q39. The sublingual gland is predominantly which type of gland?
- Serous
- Mucous
- Mixed equally serous and mucous
- Lymphoepithelial
Correct Answer: Mucous
Q40. Which cellular structure between epithelial cells restricts paracellular movement and helps maintain saliva composition?
- Gap junctions
- Tight junctions (zonula occludens)
- Desmosomes only
- Hemidesmosomes
Correct Answer: Tight junctions (zonula occludens)
Q41. The basolateral membrane protein that drives Na+ reabsorption in striated duct cells is:
- Na+/K+ ATPase
- CFTR chloride channel
- Voltage-gated Na+ channel (Nav1.1)
- Na+/glucose cotransporter SGLT1
Correct Answer: Na+/K+ ATPase
Q42. Which cholinergic agonist is commonly used to stimulate salivary flow in xerostomia patients?
- Atropine
- Pilocarpine
- Propranolol
- Clonidine
Correct Answer: Pilocarpine
Q43. Which antimuscarinic agent is often used preoperatively to reduce excessive salivation?
- Glycopyrrolate
- Neostigmine
- Physostigmine
- Edrophonium
Correct Answer: Glycopyrrolate
Q44. Salivary amylase is synthesized in acinar cells on which cellular organelle before packaging into secretory granules?
- Mitochondria
- Rough endoplasmic reticulum and Golgi apparatus
- Smooth endoplasmic reticulum only
- Peroxisomes
Correct Answer: Rough endoplasmic reticulum and Golgi apparatus
Q45. Compared with plasma, resting saliva typically has which ionic profile?
- Higher Na+ and lower K+
- Lower Na+ and higher K+
- Identical Na+ and K+ concentrations
- Extremely high Ca2+ making it hypertonic
Correct Answer: Lower Na+ and higher K+
Q46. Central control of salivation involves which brainstem nuclei?
- Substantia nigra only
- Superior and inferior salivatory nuclei
- Red nucleus and locus coeruleus
- Nucleus ambiguus exclusively
Correct Answer: Superior and inferior salivatory nuclei
Q47. Which autoimmune disease primarily targets salivary and lacrimal glands, leading to xerostomia and dry eyes?
- Graves disease
- Sjögren’s syndrome
- Myasthenia gravis
- Systemic lupus erythematosus
Correct Answer: Sjögren’s syndrome
Q48. The papilla where Stensen’s duct opens is typically located opposite which tooth?
- Maxillary first molar
- Maxillary second molar
- Mandibular second premolar
- Mandibular canine
Correct Answer: Maxillary second molar
Q49. Compared to plasma, which ion tends to be relatively higher in saliva?
- Sodium (Na+)
- Chloride (Cl-)
- Potassium (K+)
- Glucose
Correct Answer: Potassium (K+)
Q50. Saliva is useful in therapeutic drug monitoring and diagnostics primarily because it:
- Reflects total plasma drug concentration including protein-bound fraction
- Is invasive and difficult to collect
- Frequently mirrors the free (unbound) fraction of drugs and is noninvasive
- Contains no measurable drugs or metabolites
Correct Answer: Frequently mirrors the free (unbound) fraction of drugs and is noninvasive

I am a Registered Pharmacist under the Pharmacy Act, 1948, and the founder of PharmacyFreak.com. I hold a Bachelor of Pharmacy degree from Rungta College of Pharmaceutical Science and Research. With a strong academic foundation and practical knowledge, I am committed to providing accurate, easy-to-understand content to support pharmacy students and professionals. My aim is to make complex pharmaceutical concepts accessible and useful for real-world application.
Mail- Sachin@pharmacyfreak.com