Table of Contents
Mechanism of Action of SSRIs (Selective Serotonin Reuptake Inhibitors)
Introduction
Selective Serotonin Reuptake Inhibitors (SSRIs) are first-line antidepressants commonly used in the treatment of major depressive disorder, generalized anxiety disorder, panic disorder, and other psychiatric conditions. They act by increasing the availability of serotonin (5-HT) in the synaptic cleft and are preferred for their favorable side effect profile compared to older antidepressants.
Common SSRIs include:
- Fluoxetine
- Sertraline
- Paroxetine
- Citalopram
- Escitalopram
- Fluvoxamine
SSRIs are heavily tested in exams like USMLE, NCLEX, GPAT, and NEET-PG.
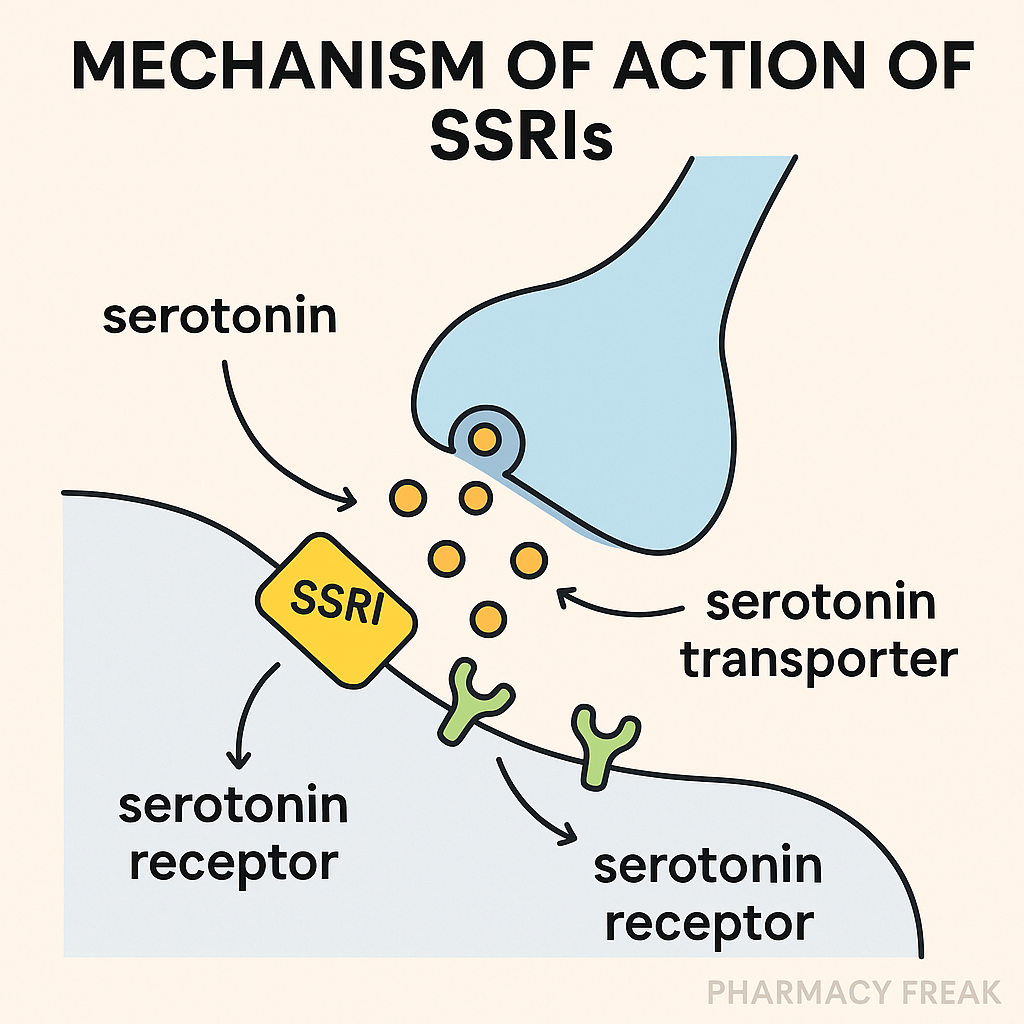
Stepwise Mechanism of Action of SSRIs
- Presynaptic inhibition of serotonin reuptake
SSRIs bind to and inhibit the serotonin transporter (SERT) on the presynaptic neuron. - Increased serotonin in synaptic cleft
This inhibition leads to increased extracellular serotonin levels at serotonergic synapses. - Enhanced serotonin signaling
The elevated 5-HT levels increase serotonergic neurotransmission, particularly in brain regions involved in mood regulation such as the prefrontal cortex and hippocampus. - Downregulation of post-synaptic 5-HT receptors
Chronic SSRI use leads to adaptive receptor changes, including desensitization of certain post-synaptic serotonin receptors, which contributes to the delayed clinical response. - Mood stabilization and anxiolytic effect
These changes collectively improve mood, reduce anxiety, and stabilize emotional response over 2–6 weeks.
Pharmacokinetic Parameters of SSRIs
| Drug | Half-life | Metabolism | CYP Interaction | Excretion |
|---|---|---|---|---|
| Fluoxetine | 1–3 days (norfluoxetine ~7 days) | Hepatic (CYP2D6) | Strong CYP2D6 inhibitor | Renal + fecal |
| Sertraline | ~26 hours | Hepatic (CYP2C19, CYP2B6) | Moderate | Renal + fecal |
| Paroxetine | ~21 hours | Hepatic (CYP2D6) | Strong CYP2D6 inhibitor | Renal |
| Citalopram | ~35 hours | Hepatic (CYP2C19) | Mild | Renal |
| Escitalopram | ~27–32 hours | Hepatic (CYP2C19, CYP3A4) | Mild | Renal |
| Fluvoxamine | ~15–22 hours | Hepatic (CYP1A2) | Strong CYP1A2 inhibitor | Renal |
Clinical Uses of SSRIs
- Major depressive disorder (MDD)
- Generalized anxiety disorder (GAD)
- Panic disorder
- Social anxiety disorder
- Obsessive-compulsive disorder (OCD)
- Premenstrual dysphoric disorder (PMDD)
- Post-traumatic stress disorder (PTSD)
- Bulimia nervosa (fluoxetine)
- Off-label uses: premature ejaculation, fibromyalgia
Adverse Effects of SSRIs
- Gastrointestinal symptoms – nausea, diarrhea
- Sexual dysfunction – decreased libido, anorgasmia
- Weight changes – gain (paroxetine), loss (fluoxetine)
- Sleep disturbances – insomnia or drowsiness
- Initial anxiety/agitation
- Serotonin syndrome – when combined with other serotonergic agents
- Suicidal ideation – increased risk in adolescents (boxed warning)
- Withdrawal symptoms – especially with paroxetine (short half-life)
Comparative Analysis: SSRIs vs TCAs
| Feature | SSRIs | TCAs |
|---|---|---|
| Receptor selectivity | Highly selective for SERT | Non-selective (SERT + NET + others) |
| Side effect profile | Better tolerated | More anticholinergic effects |
| Lethal in overdose | Rare | Yes |
| Onset of action | 2–4 weeks | 2–4 weeks |
| Weight gain | Moderate | Common |
Practice MCQs
Q1. What is the primary target of SSRIs?
a. Norepinephrine transporter
b. Monoamine oxidase
c. Serotonin transporter ✅
d. GABA receptor
Q2. SSRIs increase serotonin by:
a. Inhibiting its synthesis
b. Enhancing receptor binding
c. Blocking its reuptake ✅
d. Stimulating its release
Q3. Which SSRI has the longest half-life?
a. Sertraline
b. Paroxetine
c. Fluoxetine ✅
d. Fluvoxamine
Q4. A major sexual side effect of SSRIs is:
a. Premature ejaculation
b. Increased libido
c. Anorgasmia ✅
d. Priapism
Q5. Which condition is fluoxetine specifically approved for besides depression?
a. PTSD
b. Bulimia nervosa ✅
c. ADHD
d. Schizophrenia
Q6. SSRIs are contraindicated with:
a. NSAIDs
b. Antacids
c. MAO inhibitors ✅
d. Beta-blockers
Q7. What causes serotonin syndrome?
a. SSRI overdose
b. SSRIs combined with other serotonergic drugs ✅
c. Abrupt SSRI discontinuation
d. Antipsychotic use
Q8. Which SSRI is most associated with withdrawal symptoms?
a. Escitalopram
b. Sertraline
c. Paroxetine ✅
d. Fluoxetine
Q9. SSRIs take how long to produce clinical benefit?
a. 24–48 hours
b. 1 week
c. 2–6 weeks ✅
d. Immediately
Q10. Which enzyme metabolizes fluoxetine?
a. CYP1A2
b. CYP2D6 ✅
c. CYP3A4
d. CYP2E1
FAQs
Q1: Can SSRIs be used in children?
Yes, but with caution. Fluoxetine is FDA-approved for pediatric depression and OCD.
Q2: Do SSRIs work immediately?
No. Clinical effects typically appear after 2–4 weeks of regular dosing.
Q3: Can SSRIs cause withdrawal symptoms?
Yes. Abrupt discontinuation can cause dizziness, nausea, irritability, especially with short-acting SSRIs like paroxetine.
Q4: Are SSRIs addictive?
No. They are not habit-forming or addictive in the traditional sense.
Q5: Can SSRIs be combined with other antidepressants?
Generally avoided due to serotonin syndrome risk, especially with MAO inhibitors or other serotonergic agents.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Review of Pharmacology – Sparsh Gupta
- FDA Labeling and Prescribing Info
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK538495/
I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com