Introduction
Glycopeptides, most notably vancomycin, are a class of bactericidal antibiotics that inhibit bacterial cell wall synthesis by a mechanism distinct from β-lactams. Vancomycin is a crucial agent against Gram-positive infections, especially methicillin-resistant Staphylococcus aureus (MRSA) and Clostridium difficile.
These antibiotics are vital for USMLE, NCLEX, GPAT, and NEET-PG due to their life-saving role, narrow spectrum, and resistance considerations.
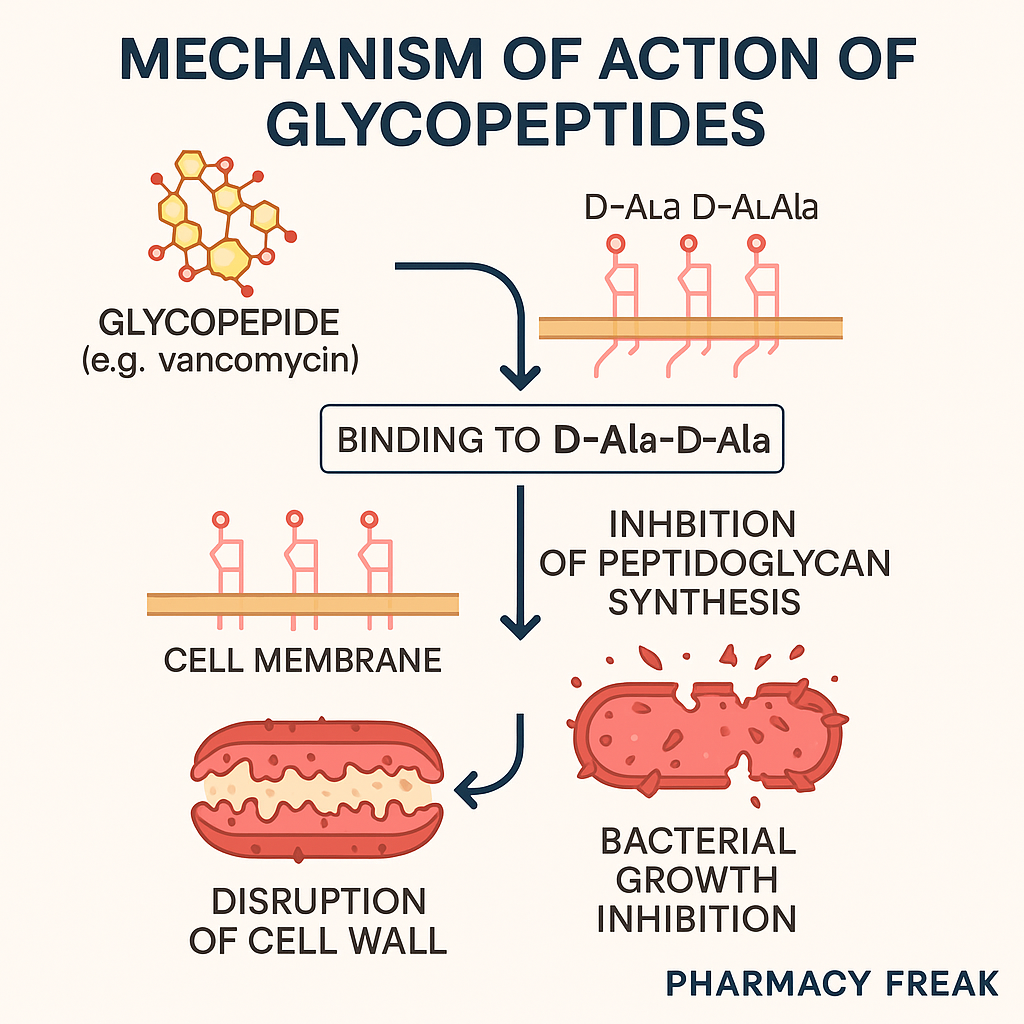
Stepwise Mechanism of Action of Glycopeptides
- Binding to D-Ala-D-Ala terminus of peptidoglycan precursors
Vancomycin binds firmly to the terminal D-Ala-D-Ala residues of nascent peptidoglycan units. - Inhibition of transglycosylation and transpeptidation
This binding blocks the action of transglycosylase and transpeptidase enzymes, which are responsible for polymerizing and cross-linking the peptidoglycan chains. - Prevention of cell wall synthesis
Without proper cross-linking and elongation, the bacterial cell wall becomes structurally weak. - Bacterial lysis and death
The disruption causes osmotic imbalance, leading to cell lysis in actively dividing bacteria. - Selective Gram-positive activity
Glycopeptides are too large to penetrate Gram-negative outer membranes, so they act only on Gram-positive bacteria.
Pharmacokinetic Parameters of Vancomycin
| Parameter | Value |
|---|---|
| Bioavailability | Very poor orally; used IV for systemic infections |
| Half-life | 6–10 hours (longer in renal failure) |
| Protein binding | ~50% |
| Metabolism | Minimal |
| Excretion | Renal (unchanged) |
| Therapeutic drug monitoring (TDM) | Required for IV use (trough levels) |
Clinical Uses of Glycopeptides
- MRSA infections (sepsis, pneumonia, endocarditis)
- Clostridium difficile colitis (oral vancomycin)
- Enterococcal infections (VSE)
- Surgical prophylaxis in penicillin-allergic patients
- Serious Gram-positive infections resistant to β-lactams
Adverse Effects of Glycopeptides
- Red man syndrome – flushing, rash due to histamine release
- Nephrotoxicity (dose-related; increased with aminoglycosides)
- Ototoxicity (rare but serious)
- Phlebitis at injection site
- Hypersensitivity reactions
- Neutropenia (with prolonged use)
Comparative Analysis: Vancomycin vs Teicoplanin
| Feature | Vancomycin | Teicoplanin |
|---|---|---|
| Dosing frequency | Twice or once daily (IV) | Once daily (IV/IM) |
| TDM required | Yes | Not routinely |
| Half-life | Shorter (~6 h) | Longer (~70–100 h) |
| Administration route | IV/Oral (non-absorbable) | IV/IM only |
| Red man syndrome | Common | Rare |
Practice MCQs
Q1. Vancomycin inhibits cell wall synthesis by binding to:
a. PBPs
b. D-Ala-D-Ala terminus ✅
c. DNA gyrase
d. 30S ribosome
Q2. Vancomycin is mainly effective against:
a. Gram-negative rods
b. Mycobacteria
c. Gram-positive bacteria ✅
d. Fungi
Q3. Which adverse reaction is specific to rapid IV infusion?
a. Nephrotoxicity
b. Red man syndrome ✅
c. Photosensitivity
d. Seizures
Q4. Oral vancomycin is used to treat:
a. MRSA pneumonia
b. UTI
c. Clostridium difficile colitis ✅
d. Syphilis
Q5. Vancomycin-resistant Enterococci modify:
a. PBPs
b. D-Ala-D-Ala to D-Ala-D-Lac ✅
c. Ribosomal subunit
d. Porins
Q6. Why is vancomycin ineffective against Gram-negatives?
a. Enzymatic degradation
b. Drug efflux
c. Cannot penetrate outer membrane ✅
d. No peptidoglycan layer
Q7. Which of the following requires TDM?
a. Oral metronidazole
b. IV vancomycin ✅
c. Amoxicillin
d. Linezolid
Q8. Vancomycin acts on bacteria that are:
a. Dormant
b. Actively dividing ✅
c. Anaerobic only
d. Spore-forming
Q9. What is the common route of excretion?
a. Liver
b. Lungs
c. Renal ✅
d. Skin
Q10. What monitoring is essential during vancomycin therapy?
a. Liver enzymes
b. ECG
c. Trough plasma levels ✅
d. Pulmonary function
FAQs
Q1: Can vancomycin be used orally for systemic infections?
No. Oral vancomycin is only for C. difficile colitis as it’s not absorbed systemically.
Q2: What causes red man syndrome?
Rapid IV infusion leads to histamine release, causing flushing and rash.
Q3: How is vancomycin dosed in renal failure?
Dosing must be adjusted and trough levels monitored due to renal excretion.
Q4: Is vancomycin safe in pregnancy?
Yes, it is Category B and can be used if needed.
Q5: What causes resistance in VRE?
Change in binding site from D-Ala-D-Ala to D-Ala-D-Lac, reducing affinity.
References
- KD Tripathi – Essentials of Medical Pharmacology
- Goodman & Gilman – The Pharmacological Basis of Therapeutics
- Sparsh Gupta – Review of Pharmacology
- NCBI: https://www.ncbi.nlm.nih.gov/books/NBK459455/
I am pursuing MBA in pharmaceutical management from NIPER Hyderabad with a strong academic record and proven success in national-level pharmacy entrance exams. I secured AIR 61 in NIPER 2024 (MS/M.Pharm) and AIR 27 in NIPER MBA, along with AIR 147 in GPAT 2024 and AIR 907 in GPAT 2023. I also achieved AIR 6 in AIIMS CRE-2025 for Drug Store Keeper and was selected as a Pharmacist (AIR 61) for ESIC. Additionally, I was the Runner-Up in Round 2 of the EY Case Study Competition.
At PharmacyFreak.com, I aim to guide future pharmacists through expert content, exam strategies, and insightful resources based on real experience and academic excellence.
Mail- harsh@pharmacyfreak.com